The clinical practice patterns of fetal ultrasonography in the first-trimester: A questionnaire survey of members of the Korean Society of Ultrasound in Obstetrics and Gynecology
Article information
Abstract
Objective
This study aimed to survey the current clinical practice of first-trimester ultrasonography among members of the Korean Society of Ultrasound in Obstetrics and Gynecology (KSUOG) and to provide basic data for making practical recommendations about first-trimester ultrasonography scan in Korea.
Methods
This survey was conducted using a self-administered anonymous questionnaire. The first-trimester in this survey was divided into two parts: early and late first-trimester. The survey was focused on safety issue, nuchal translucency (NT) cutoff, the anatomic structures they check, and the need for practical recommendations or educational courses during the first-trimester.
Results
During the study period, 194 KSUOG members participated into this survey. The survey on early first-trimester scan reveal that 173 (89.2%) of respondents had used pulsed-wave Doppler or color Doppler imaging to monitor fetal heart beat. For the late first-trimester scan, 145 (74.7%) of respondents was found to check for fetal anatomical assessments during their NT screening performance; however, the clinical practice patterns were considerably varied among participants. More than half of the respondents used the criterion of NT ≥3.0 mm to define increased NT. Approximately 80% of respondents stated that the screening ultrasonography of fetal structures in the first-trimester was necessary. Furthermore, 187 (96.4%) of respondents were in favor of a recommendation for first-trimester ultrasonography in Korea.
Conclusion
This is the first survey of the current clinical practice of first-trimester ultrasonography in Korea. Our survey findings highlight the need for the practical recommendation or educational course for first-trimester ultrasonography.
Introduction
Since the first use of ultrasonography for the diagnosis of an abdominal mass by Ian Donald in 1958, it has been routinely used in modern obstetric practice [1]. Much technical advancements, including high-frequency transvaginal probe, have made it possible to obtain detailed images of early fetal structures. Nuchal translucency (NT) in the first-trimester has been proven the most important ultrasonography marker for fetal aneuploidy and various malformations. Thus, first-trimester is an essential period for prenatal diagnosis. Most pregnant women want to know whether their baby is healthy as early as possible [2].
The advantages of first trimester anomaly scanning are earlier reassurance and easier termination [3,4,5]. Disadvantages are need for experienced sonographers, additional cost, and some late developmental structures which cannot be detected during the late first trimester [6,7,8]. Although the second trimester ultrasonography scan is still a gold-standard method for fetal anatomic evaluation, detailed and systematic examination in the late first trimester can detect almost half of major fetal anomalies [9]. In 2013, the International Society of Ultrasound in Obstetrics and Gynecology guidelines for first-trimester fetal ultrasonography were published to provide instructions for healthcare practitioners performing routine or indicated first-trimester fetal ultrasonography [10]. According to these guidelines, first-trimester ultrasonography is performed to determine the followings: 1) accurate gestational age, 2) the number of fetuses, 3) chorionicity and amnionicity in a multiple pregnancy, 4) NT thickness when possible, and 5) fetal structural abnormalities at the end of the first-trimester. However, no recommendations or guidelines for first-trimester ultrasonography are optimal for use in Korea. Therefore, we conducted an organizational survey regarding first-trimester ultrasonography among members of the Korean Society of Ultrasound in Obstetrics and Gynecology (KSUOG) via an internet-based self-reporting questionnaire. The survey was focused on safety issue, NT cutoff, the anatomic structures they check, and the need for practical recommendations or educational courses during the first-trimester.
This study aimed to survey the current clinical practice of first-trimester ultrasonography among members of the KSUOG and to provide baseline data for making recommendations regarding first-trimester ultrasonography in Korea.
Materials and methods
1. Data collection and analysis
From February 24 to March 14 2014, KSUOG members were assessed using a self-administered anonymous questionnaire survey. This survey was supervised by a KSUOG-affiliated ultrasonography research group. The survey data were collected via an online system using a Google Drive form. The questionnaire (in Korean) can be viewed at the following website: https://docs.google.com/forms/d/1knPWgHXN6FD1Y5PekH7RyQVI2K2GdtZ3whliI5T-Pgs/viewform. The survey was developed in coordination with the authors in this study. The survey was divided into two parts: early first-trimester (presence of a gestational sac to 10+6 weeks' gestation) and late first-trimester (11+0 weeks' gestation to 13+6 weeks' gestation). Data were analyzed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive and frequency data were computed for primary analysis.
2. Participant characteristics
We obtained the demographic and clinical characteristics of the KSUOG members (age, sex, years of experience in obstetrics, and whether the member performed delivery) and their institutional background (clinic at which deliveries were performed or not, and general or university hospital). We also investigated the institutional practice of performing first-trimester ultrasonography (number of procedures, and the person who performed ultrasonography).
3. Outcome variables
Responses to multiple-choice or yes/no questions were obtained by clicking the appropriate button. The respondents were asked to indicate the parameters examined for in the early first-trimester from a checklist that included the following: fetal viability; exact gestational age; size and location of gestational sac; fetal heart beat (FHB); method used to for confirm FHB (visual, M-mode, power Doppler, color Doppler, etc.); size and shape of yolk sac; number of fetuses; chorionicity and amnionicity for multiple gestations; abnormalities of the uterus and ovary; and use of three-dimensional ultrasonography.
Next, from a second checklist that included items to determine the clinical practice pattern, they were asked to indicate the procedures performed in late first-trimester: basic examination (crown-rump length [CRL], FHB, abnormalities of the uterus and ovary); basic examination + NT measurement; a basic examination + NT measurement + nasal bone (NB) measurement; basic examination + NT measurement + NB measurement + examination for other structural deformities; basic examination + NT measurement + examination for other structural deformities; and other methods of examination. The checklist for the first trimester included the following: NT screening; measurement between 11+0 and 13+6 weeks' gestation; measurement from 45 to 84 mm of the CRL; the fetus occupying >75% of the image; mid-sagittal plane, including echogenic tip, palate, and diencephalon; neutral position of the fetus; discrimination of fetal skin and amnion; measurement at the widest space of the NT; and use of calipers on the inner borders of the nuchal space. Other questions on NT measurement included those on the number of repeat measurements (one, two, three, or more) and the indications for repeat NT measurement (≥2.5 mm, ≥3.0 mm, or ≥95th percentile according to gestational age). The adequate timing of ultrasonography for fetal anatomy assessment and appropriate methods for the late first-trimester screening were surveyed. Respondents were asked to indicate which of the following they had checked/performed during late first-trimester: NT; NB; head (head shape, cranial ossification, midline falx, and choroid plexus); face (orbit and profile); neck; thorax; heart (heart activity, size, cardiac axis, and four-chamber view); abdomen (stomach, bowel, kidneys, urinary bladder, cord insertion/abdominal wall, and cord vessels); spine; limb (including hand and foot); sex; three-dimensional ultrasonography; and Doppler ultrasonography (including cord vessel or uterine artery).
Finally, the respondents were asked whether they considered late first-trimester screening ultrasonography necessary for detecting fetal structural abnormalities, and what they think the reasons for considering it unnecessary and not performing late first-trimester ultrasonography. The respondents were asked whether they would consider a recommendation made by the KSUOG for first-trimester ultrasonography, and whether they have a willingness to participate in an educational course on first-trimester ultrasonography if it would conducted by the KSUOG.
Results
1. Characteristics of the clinicians and institutional background information
During the study period, 194 KSUOG members participated into this survey. Table 1 shows the individual characteristics and institutional background information. The mean age of the respondents was 41.2 years. Of the respondents, 84% (163 of 194) performed delivery in their obstetric practice. During the first-trimester, ultrasonography was most commonly performed three times.
2. Clinical practice pattern of early and late first-trimester ultrasonography
During early first-trimester, >95% of respondents confirmed that they had examined for all of the following: fetal viability, exact gestational age, size and location of the gestational sac, FHB, number of fetuses, chorionicity and amnionicity in multiple pregnancies, size and shape of the yolk sac, and abnormalities of the uterus and ovaries. However, 173 (89.2%) had used pulsed-wave Doppler or color Doppler imaging to monitor FHB during the early first-trimester, and only 21 (10.8%) had used visual or M-mode ultrasonography. Of the respondents, 39% stated that they had used three-dimensional ultrasonography during the early first-trimester.
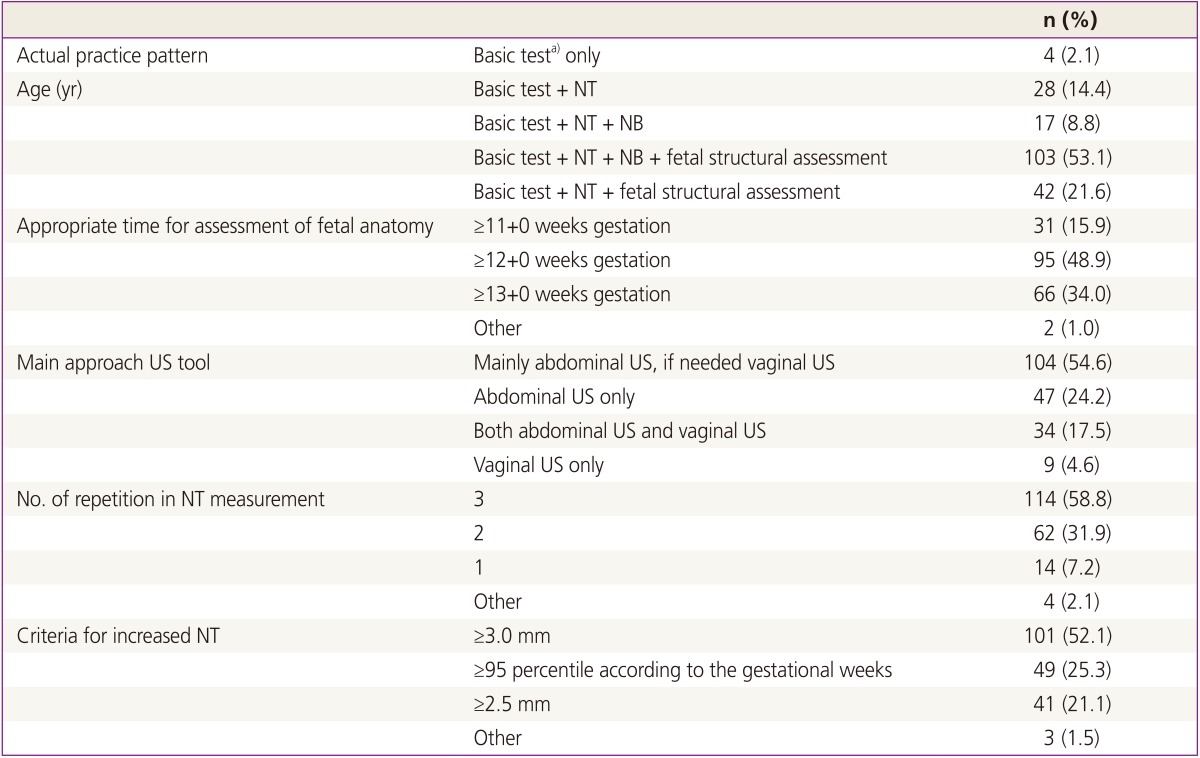
Table 2 shows the clinical practice patterns of fetal ultrasonography during the late first-trimester. Of the respondents, 145 (74.7%) stated that they investigated fetal structural abnormalities in the late first-trimester using ultrasonography. 95 (48.9%) of respondents considered the appropriate time for fetal anatomy assessment to be 12+0 weeks' gestation. More than half of the respondents (n=114, 58.8%) performed NT measurements thrice. One hundred four (54.6%) respondents usually used trans-abdominal scanning as the main approach, sometimes trans-vaginal scanning was performed if it was necessary. A small number of respondents (n=9) performed vaginal ultrasonography alone. Also, for the criteria used to diagnose increased NT; more than half of the respondents used the criterion of NT ≥3.0 mm. Table 3 summarizes the screening procedures performed before NT measurement. Mid-sagittal plane measurement (including echogenic tip, palate, and diencephalon) and measurement from 45 to 84 mm of CRL were considered the most difficult criteria to satisfy. Table 4 shows the fetal structures assessed by the obstetricians during the late first-trimester. The proportion of respondents, who assessed fetal structures besides NT, NB, and the head, was low (48.9% to 69.0%). In particular, the ultrasonographic practice patterns for eight fetal structure parts (head, face, neck, thorax, heart, abdomen, spine, and limb) differed significantly among respondents (Fig. 1).
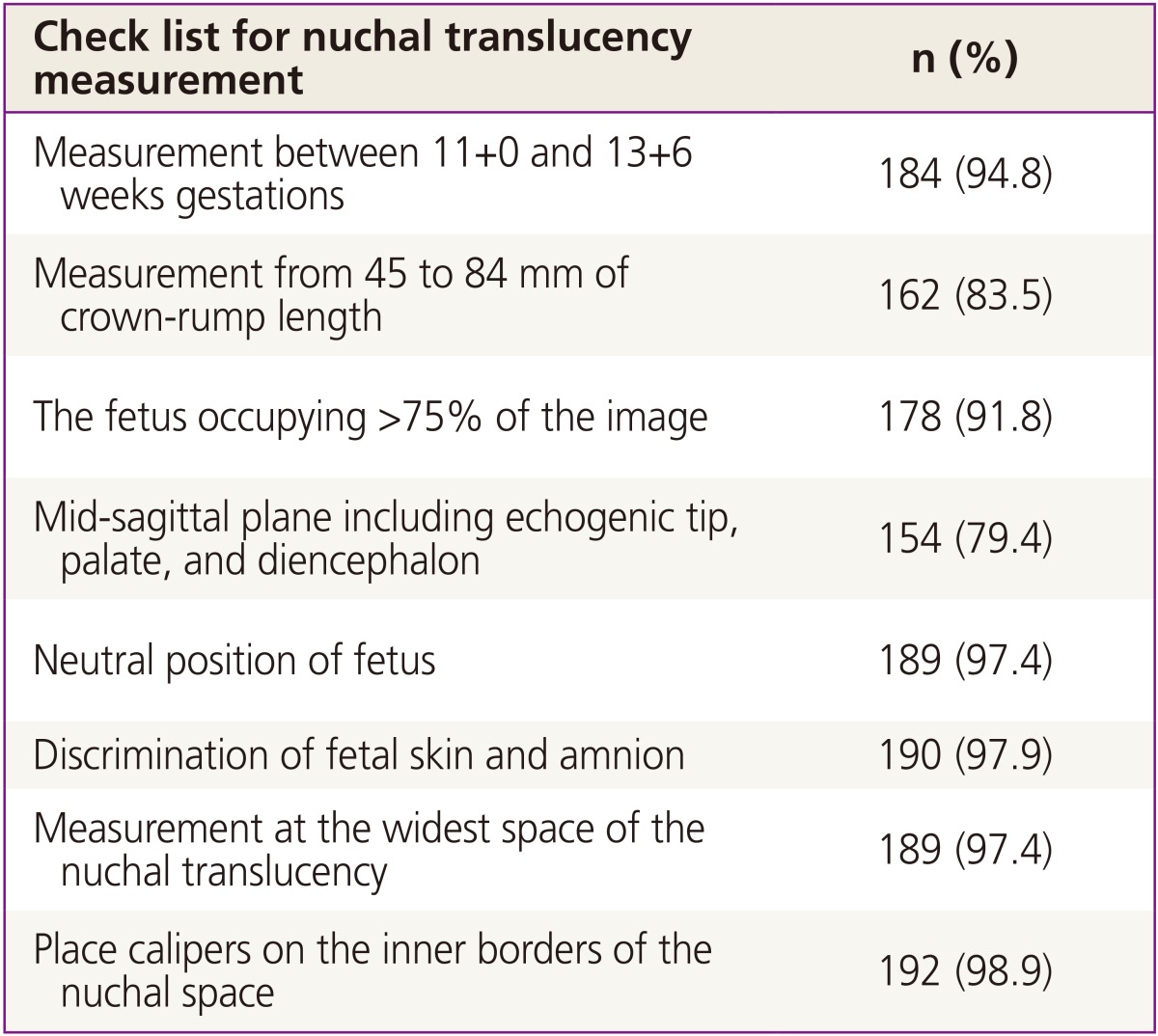
Screening procedures performed before nuchal translucency examination during the late first trimester
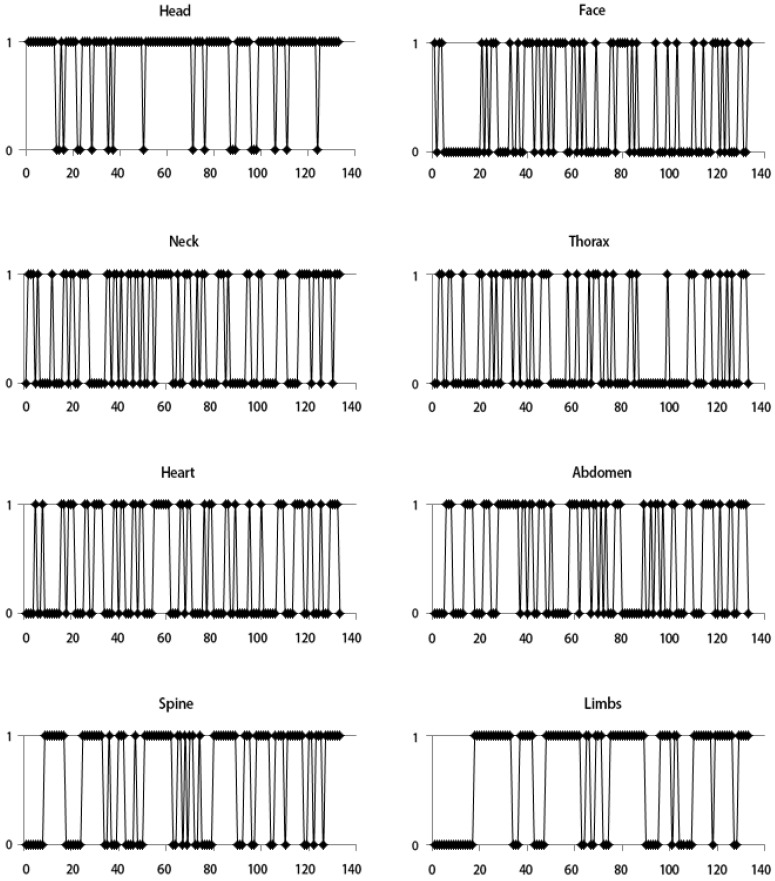
Ultrasonographic tracings for eight fetal structural parts during the late first-trimester. The pattern of tracings for the eight parts (head, face, neck, thorax, heart, abdomen, spine, and limbs) differed significantly among respondents. X axis means individual respondents and Y axis means answers for checking the parts; 1 means checking and 0 means not checking.
3. The perception of respondents concerning first-trimester screening fetal ultrasonography
Approximately 80% of respondents stated that they considered ultrasonographic examination for fetal structures in the first-trimester necessary; 94 responded "it is necessary and performed", 61 responded "it is necessary but not performed", and 38 responded "it is not necessary" (Fig. 2). The 61 respondents did not perform first-trimester ultrasonography for fetal structures, although they considered it necessary, for the following reasons: no relevant clinical guideline (34%, 21 of 61); low medical fee (24%, 15 of 61); no experience of performing examination during the late first-trimester (18%, 11 of 61); and other reasons (lack of time, no evidence of safety, and redundant US machine). The 38 respondents stated that they considered ultrasonography for fetal structure assessment in the first-trimester unnecessary because reexamination is needed during the second trimester irrespective of examination during the first-trimester (55%, 21 of 38); few anomalies can be detected in the first-trimester (28%, 11 of 38); chorionic villi sampling cannot be performed, and amniocentesis has to be performed for the chromosome study (7%, 3 of 38)

The need for late first-trimester ultrasonography to detect fetal structural abnormalities; 79.9% considered it necessary.
In terms of the usage of the clinical recommendation if it was provided by the KSUOG, 33.5% (65 of 194) of the respondents answered "absolutely yes", whereas more than 60% (122 of 194) answered "depends on the content of the recommendation". Considered together, 187 (96.4%) of the respondents were in favor of a recommendation for first-trimester ultrasonography. Similarly, in terms of attendance at the KSUOG educational course, 35.6% (69/194) of the respondents confirmed that they would attend the course, 58.2% (113 of 194) stated that they would attend if they could, and 182 respondents clearly indicated their clear reasons for attending such an educational course.
Discussion
This is the first survey on the current clinical practice of first-trimester ultrasonography in Korea. This survey showed that practice patterns for first-trimester ultrasonography varied considerably among respondents. In the present study, most of the survey responses were provided by the obstetricians who performed the delivery. Approximately 87% of respondents who performed ultrasonography in the first-trimester were obstetricians. During the first-trimester, ultrasonography was most commonly performed three times. In the early first-trimester (presence of a gestational sac to 10+6 weeks' gestation), most clinicians (95% of respondents) checked all of the items on the checklist during the first-trimester scanning. The majority of respondents had performed first-trimester ultrasonography to determine gestational age, the number of fetuses, chorionicity and amnionicity in multiple pregnancies, and to measure NT.
There have been many concerns about the safety of ultrasonography scan during the first-trimester. The main biologic effect of ultrasonography is thermal effect. Doppler ultrasonography is associated with higher energy output and therefore potential harmful thermal effect [11,12]. According to guidelines of International Society of Ultrasound in Obstetrics and Gynecology, in the first-trimester Doppler ultrasonography examination should only be used, if clinically indicated [10]. However, it was found that almost 90% of respondents used pulsed-wave Doppler or color Doppler imaging to determine FHB in the early first-trimester. In the late first-trimester (11+0 weeks' gestation to 13+6 weeks' gestation), approximately 75% of the respondents stated that they had already checked for fetal structural anomalies during NT measurement. However, the methods used for fetal anomaly screening differed significantly among respondents. There was no unified indication for performing abdominal or transvaginal ultrasonography in the late first-trimester. To ensure accurate NT measurement, many organizations such as the Fetal Medicine Foundation issued strict guidelines [13,14,15]. The results of this survey showed that approximately 20% seemed not measure NT with the optimal mid-sagittal plane. Fetal NT measurement by ultrasonography in the first-trimester is effective method for the screening of major chromosomal abnormalities, and structural anomalies. When it is combined with maternal serum pregnancy-associated plasma protein A, and free β-human chorionic gonadotropin, the sensitivity of screening would exceed 80% at a screen positive rate of 5% [16,17,18]. However, there is no consensus on optimal cutoff value that may allow us to leave out maternal serum screening confirmation before proceeding chromosomal study directly. Recently published studies on fetal outcome in fetuses with increased NT have used different cutoff values of 2.5 mm, 3.0 mm, 95th percentile and 99th percentile [18,19,20,21]. In this survey, the criteria used to define increased NT varied, but more than half of the respondents (101, 52.6%) used the criterion of NT ≥3.0 mm to represent an increased NT. Fourteen respondents (7.2%) stated that they had performed an NT measurement only once.
Approximately 80% of respondents considered detailed screening ultrasonographic examination of fetal structures in the first-trimester necessary. If a recommendation for first-trimester ultrasonography was in place, 95% of respondents stated that they would be willing to use it. In terms of educational courses, 90% of respondents stated that they would willingly participate in an educational program regarding fetal structural ultrasonography for the first-trimester. Therefore, a recommendation for first-trimester ultrasonography that can be applied to the Korean population is required, along with a suitable educational program.
A limitation of this survey is that the majority of participants enrolled in this survey were doctors working in tertiary hospitals. In terms of clinical resources, there might be a large difference between primary clinics and tertiary hospitals. Thus, we need to extend our survey further to include KSUOG members from primary clinics. Practitioners should receive certified training on accurately measuring NT. Many global organizations/programs provide certified training on measuring NT, the most popular being the Fetal Medicine Foundation and Nuchal Translucency Quality Review programs. Both these organizations offer an online course for training and certification. Ideally, all practitioners who perform combined screening program for Down's syndrome in the first-trimester should undergo basic measurement criteria for NT measurement. Otherwise serum screening alone should be suitable for accurate screening [22,23,24].
This is the first survey to investigate the clinical practice patterns of first-trimester ultrasonography in Korea. Thus far, there has been no adequate recommendation for first-trimester ultrasonography in Korea, and hence this survey is very important. The survey findings highlight the lack of any practical recommendations or educational courses for first-trimester ultrasonography. Systematic screening procedures are important for detecting structural anomalies during first-trimester ultrasonography. A predefined recommendation and satisfactory education would help establish a system to perform systematic scanning.
Acknowledgments
We thank the members of KSUOG for their assistance with data collection for this survey.
Notes
No potential conflict of interest relevant to this article was reported.