 |
 |
- Search
| Obstet Gynecol Sci > Volume 66(5); 2023 > Article |
|
Abstract
Objective
We present an educational technique for the safe completion of complete cytoreduction of diaphragmatic disease for the management of advanced ovarian malignancy.
Methods
We demonstrated these steps with attention to anatomical landmarks and surgical approaches, considering intraoperative and postoperative morbidity and mortality.
Results
We present the case of a 49-year-old female patient diagnosed with suspected stage 3C ovarian malignancy following diagnostic laparoscopy. We demonstrate the surgical application of the Pringle manoeuvre, type 3 liver mobilisation, and full-thickness diaphragmatic resection. This was completed with a primary closure technique, with integrity ensured through the performance of an air test and Valsalva manoeuvre. Final histology confirmed a serous borderline tumour with invasive implants within a port site nodule (stage 4A).
Type 3 liver mobilisation and full-thickness diaphragmatic resection with primary closure are the primary debulking surgical procedures used to manage advanced ovarian malignancies [1]. This requires a precise understanding of the anatomical landmarks, in addition to the surgical approach. Subspecialists must develop skills in this technique whilst avoiding potential complications, including injury to surrounding structures, nerves, and vessels, as well as post-operative morbidity. This video demonstrates the procedure in a 49-year-old female patient with a medical history of borderline serous ovarian cystadenoma. Investigation of symptoms revealed a CA125 level of 128, while imaging revealed a 9.8 cm complex ovarian mass with ascites, pelvic lymphadenopathy, possible metastatic liver serosa, and peritoneal nodularity. After multi-disciplinary team meeting and diagnostic laparoscopy, the patient underwent primary debulking of a suspected stage 3C ovarian malignancy (Table 1). During the laparotomy, extensive pelvic and peritoneal disease involving the right hemidiaphragm, bladder surface, appendix, and rectosigmoid were observed. On palpation, a diaphragmatic nodule raised the suspicion of full-thickness involvement with no evident cleavage plane in consideration of diaphragmatic stripping. Following total abdominal hysterectomy, salpingo-oophorectomy, omentectomy, appendectomy, and pelvic and para-aortic lymph node assessments (with pelvic lymph node dissection), type three liver mobilisation was performed using the Pringle maneouvre (Video 1, Table 2) [2,3]. Following the identification of the suprahepatic inferior vena cava and insertion of the right hepatic vein, the falciform and coronary ligaments were divided, allowing exposure of the right adrenal gland and retrohepatic inferior vena cava. The diaphragm was stripped and the muscle was opened to achieve full-thickness diaphragmatic resection with pleurectomy under direct vision of the surrounding lung parenchyma using an advanced energy device (Fig. 1) [4]. Primary closure was achieved using a single size 1 monofilament locking suture [5]. Diaphragmatic integrity was ensured by performing an air test and the Valsalva maneouvre. Further peritonectomy was performed on the bladder surface, rectosigmoid, and MorrisonŌĆÖs pouch, and a suspected port-site nodule (following diagnostic laparoscopy) was excised, achieving zero residual macroscopic disease. Final histology confirmed a serous borderline tumour with invasive implants within the port site nodule (stage 4A), warranting a medical oncology referral. Here, we highlight a challenging case requiring advanced surgical skills and knowledge, with specific consideration of intraoperative multidisciplinary decision-making regarding operative morbidity and mortality. The procedure was performed after consultation with the hepatobiliary and colorectal teams to achieve optimal cytoreduction and R0.
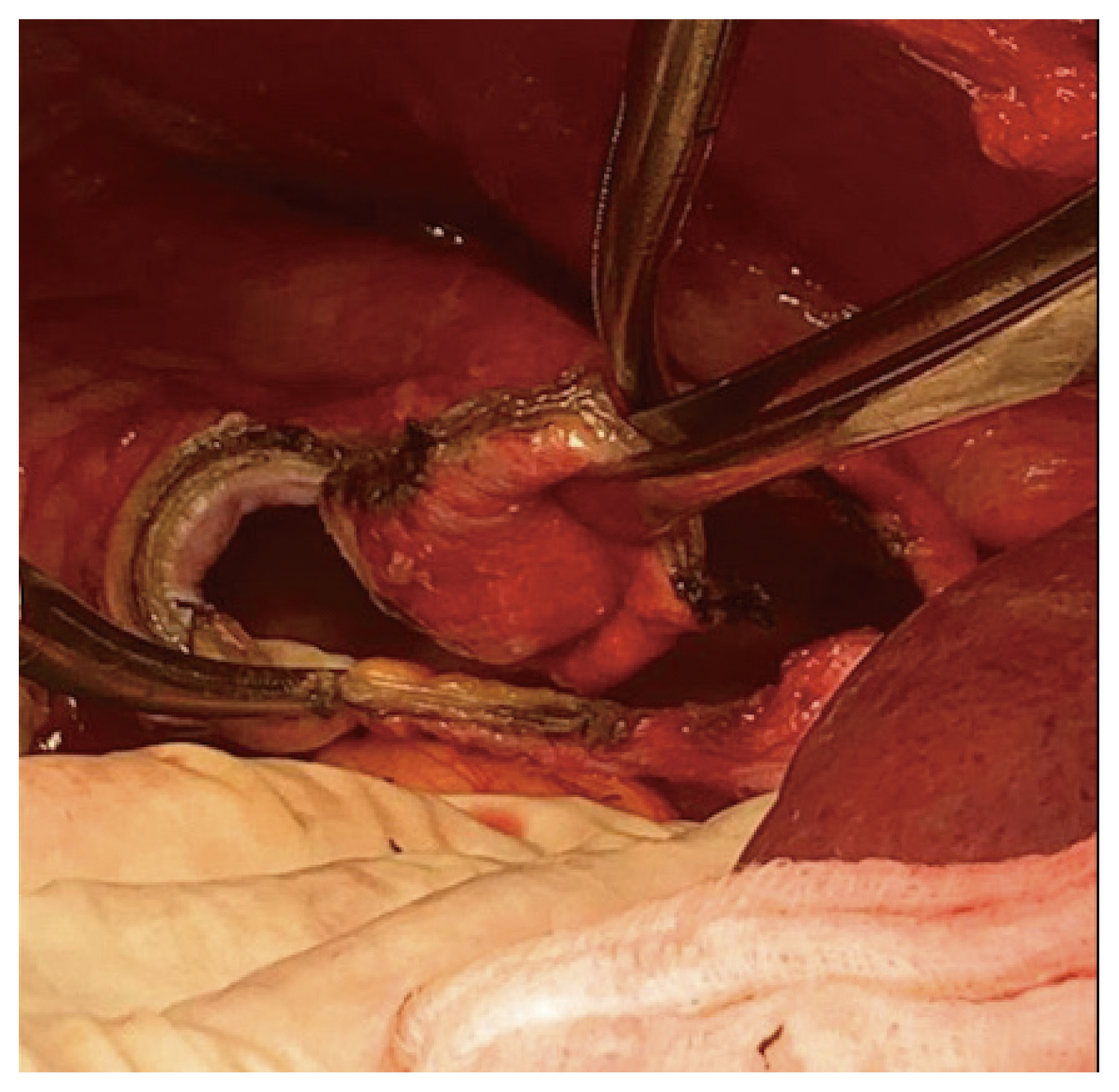
Fig.┬Ā1
Advanced energy device excising full thickness diaphragmatic nodules to include pleurectomy, ensuring appropriate macroscopic excision margins.
Table┬Ā1
Procedure materials
Table┬Ā2
Procedure summary
References
1. Buruiana FE, Ismail L, Ferrari F, Majd HS. The role of ultra-radical surgery in the management of advanced ovarian cancer: state of the art [Internet] London: IntechOpen; c2021 [cited 2022 Aug 3]. Available from: https://www.intechopen.com/chapters/78061
.
2. Tozzi R, Traill Z, Garruto Campanile R, Ferrari F, Soleymani Majd H, Nieuwstad J, et al. Porta hepatis peritonectomy and hepato-celiac lymphadenectomy in patients with stage IIIC-IV ovarian cancer: diagnostic pathway, surgical technique and outcomes. Gynecol Oncol 2016;143:35-9.


3. Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Engl J Med 2019;380:822-32.


4. Soleymani Majd H, Ferrari F, Manek S, Gubbala K, Campanile RG, Hardern K, et al. Diaphragmatic peritonectomy vs. full thickness resection with pleurectomy during visceral-peritoneal debulking (VPD) in 100 consecutive patients with stage IIIC-IV ovarian cancer: a surgical-histological analysis. Gynecol Oncol 2016;140:430-5.























