|
 |
- Search
| Obstet Gynecol Sci > Volume 67(2); 2024 > Article |
|
Abstract
Objective
To evaluate the effectiveness of additional low-pressure pulmonary recruitment in reducing postoperative shoulder pain.
Methods
A double-blind randomized controlled trial was conducted at Srinagarind Hospital between May 2021 and October 2021. Forty patients who underwent laparoscopic gynecologic surgery were randomized into either an intervention group that received additional low-pressure pulmonary recruitment (30 cmH2O) (n=20) or a control group (n=20). Shoulder pain was evaluated using a numerical rating scale from 0 to 10, 24, and 48 hours after the operation.
Results
The mean±standard deviation of shoulder pain at 24 hours after the operation of both the intervention and control groups were 2.10±2.27 and 1.45±1.73 points, respectively. The shoulder pain at 48 hours after the operation of the intervention and control groups were 1.15±1.46 and 0.85±1.73 points, respectively. There were no statistical differences in the mean difference between the two groups at 24 and 48 hours after operation (P=0.49; 95% confidence interval [CI], −0.61 to 1.91 and P=1.00; 95% CI, −0.96 to 1.56, respectively). No statistically significant differences were observed in additional analgesic medications used in either group, such as intravenous morphine or oral acetaminophen.
Laparoscopic surgery is increasingly performed for benign gynecologic diseases [1]. Less wound pain, small wound incisions, better anesthetics, shorter hospitalization, fast recovery time, and earlier return to normal daily life are advantages over exploratory laparotomy and can be safely performed with caution during the pandemic coronavirus disease-19 infection [2,3].
Pain after laparoscopic surgery was considered to be less than that after exploratory laparotomy. However, pain after minimally invasive surgery interferes with quality of life, delays normal activity, and postpones hospital discharge [3,4]. Post laparoscopic surgical pain can be divided into incisional, shoulder, pelvic, and upper abdominal pain. Up to 80% of the patients experience pain and require analgesic medication after laparoscopic procedures [1,5,6].
Several causes of post-laparoscopic shoulder pain have been described, which may be multifactorial. There are three common causes for this. The first is carbonic acid production from CO2 gas during the laparoscopic procedure, which induces a decrease in peritoneal pH, leading to peritoneal and diaphragmatic nerve damage and irritation, causing shoulder pain. Second, the condition of remaining residual gas in the abdominal cavity causes visceral ligament traction, leading to shoulder pain. Stretching of the peritoneum and diaphragm by the pneumoperitoneum results in traction of the phrenic nerve, tearing of blood vessels, and release of inflammatory mediators that evoke shoulder pain [1]. The last possible cause is foreign material stimulation, such as remaining blood or fluid above the liver [1].
To reduce post-laparoscopic shoulder pain, the pulmonary recruitment maneuver (PRM) with positive pressure ventilation of 40-60 cmH2O at the end of the operation is an effective modality that can alleviate shoulder pain by promoting CO2 gas removal from the peritoneal cavity [1].
Data from a network meta-analysis published in 2020 [7] found that PRM with 40 cmH2O performed alone or in combination with intraperitoneal saline showed promising results in reducing post-laparoscopic shoulder pain within 48 hours after gynecologic laparoscopy. A pulmonary pressure of 40-60 cmH2O can increase the risk of barotrauma and hemodynamic deterioration, although this is uncommon [8,9].
Therefore, we sought to determine whether the difference in postoperative shoulder pain improved by more than 2 points if a low pulmonary pressure recruitment maneuver (30 cmH2O) was performed at the end of gynecologic laparoscopic surgery.
A double-blind randomized controlled trial was conducted at Srinagarind Hospital between May 2021 and October 2021. This study was approved by the Ethics Committee (HE641054).
Women who planned to undergo gynecological laparoscopic surgery at the hospital were given the option to participate in the trial. The participants were aged between 18-60 years of age and had benign gynecological diseases. Pregnant women and those with a history of allergy to nonsteroidal anti-inflammatory drugs or lidocaine injections, peptic ulcer disease, coagulopathy, chronic kidney disease, pelvic infection, shoulder or upper extremity trauma, or surgery were excluded from the study. Patients who underwent conversion to laparotomy were excluded from the analysis. Written informed consent was obtained from all the eligible participants. This trial was performed and reported in compliance with the CONSORT statement and registered with the Thai Clinical Trial Register (TCTR20210513002).
Participants who met the inclusion criteria were randomly allocated to the two groups using computer-generated randomization. A random sequence analysis was performed by a statistician who was not involved in the study. All randomization sequences were kept in sequentially numbered opaque sealed envelopes. Before the end of the surgical procedure, the anesthesiologist was asked to pick the envelopes in subsequent order and perform the intervention accordingly. The assessors and participants were blinded to the study protocol.
The intervention consisted of additional pressure pulmonary recruitment at the end of the surgical procedure before trocar removal. Pulmonary recruitment was performed by an anesthesiologist with a pulmonary pressure of 30 cmH2O and held 10 seconds for five times. No participants in the control group underwent pulmonary recruitment.
All participants underwent conventional laparoscopic gynecological surgery under standardized general anesthesia. Conventional 4 ports placement was performed. The umbilical port was 12 mm thick and the three ancillary ports were 5 mm. The procedure was performed using temtanakitpaisan, and intraperitoneal pressure was maintained at 15 mmHg during the laparoscopic procedures. At the end of the procedure, all trocars were left open for 1 minute while pressing the abdomen in the Trendelenburg position 30° to release CO2 gas. Pulmonary recruitment was simultaneously performed in the intervention group. Analgesics were administered to all participants. Parecoxib was administered intravenously (40 mg) preoperatively and 12 hours later. In addition, etoricoxib 90 mg was administered orally once daily.
Based on the primary outcomes, the shoulder pain score after additional pulmonary recruitment was compared with that of the control group in laparoscopic gynecological surgery. Secondary outcomes analyzed were wound pain and side effects between the two groups. The pain scores were assessed using a numerical rating scale (NRS) from 0 (no pain) to 10 (maximum level of pain experienced). An assessor (a research nurse) asked all participants to indicate their pain scores at 24 hours and 48 hours interval after laparoscopic surgery. The pain score was accessed routinely if pain score is greater than or equal 4, additional analgesic agents were prescribed with acetaminophen and/or morphine. Other outcomes were assessed including any adverse events and postoperative complications.
The sample size was calculated based on the primary outcome, which was a comparison of the shoulder pain score in low-pressure pulmonary recruitment versus the control. A difference in the NRS score of 2.0 points was considered clinically significant. The reason for using clinically significant differences of 2.0 points was that the baseline shoulder pain was considerably low. We used the means and standard deviations of the NRS score at 24 hours from the pilot study with 10 participants, which were 3.8±2.3 points in the control group and 1.8±1.4 points in the intervention group. Therefore, the sample size was calculated as 18 per group at a power of 80% and an alpha value of 5%. Forty patients were recruited to compensate for the possible dropouts (10%).
Statistical analyses were performed using Stata version 10 (Stata Corporation, College Station, TX, USA). Descriptive statistics were used to report participants’ baseline characteristics. Student’s t-test was used to compare continuous variables. In addition, the chi-square or Fisher’s exact test was used to compare categorical variables. Differences between the comparison groups were evaluated in terms of the mean difference or relative risk with a 95% confidence interval (CI). Statistical analyses were conducted using generalized estimating equations. A P-value <0.05 was considered to be clinically significant. All analyses were performed in accordance with intention-to-treat principles.
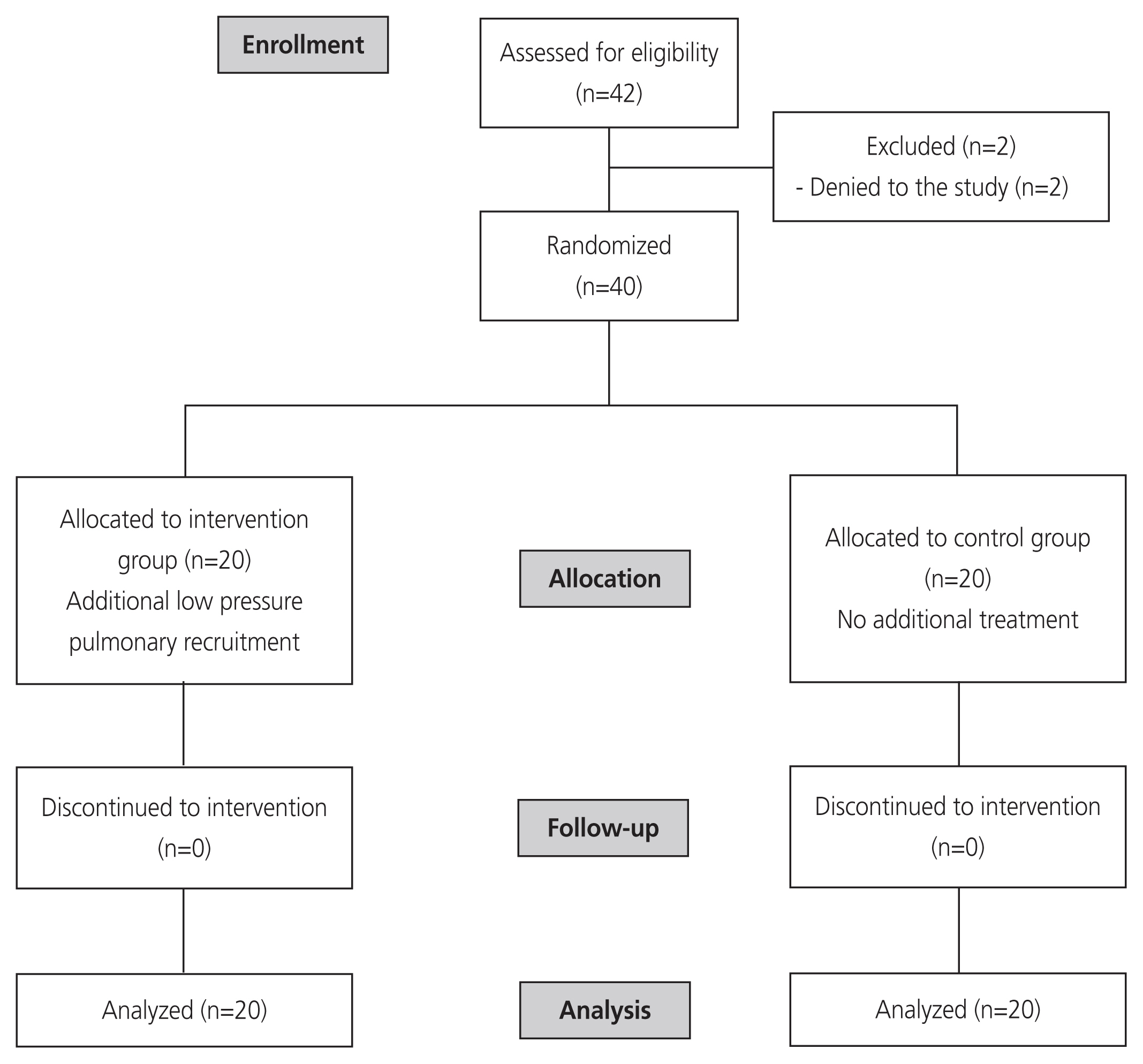
Of the study population, 42 were assessed for eligibility, and two candidates denied participating in the study. Forty participants were recruited and randomly allocated to the intervention group (pulmonary recruitment group) (n=20) or the control group (n=20). Fig. 1 presents the CONSORT flow diagram used in this study. No dropouts during the study period. None of the patients were subjected to any changes according to the doctor’s decision.
The baseline characteristics of the study participants are shown in Table 1. The mean age±standard deviation (SD) was 38.7±10.9 years. A total of 40% of the patients were multiparous, 10% were postmenopausal, and 87.5% had no underlying disease. The median body mass index (interquartile range, IQR) was 23.1 kg/m2 (21.0 to 24.7). Adnexal surgery was the most common laparoscopic procedure performed in both groups. During the intraoperative period, there were no statistically significant differences in the total CO2 volume used during the operation, operative time, amount of blood loss, and hospital stay between the two groups, as shown in Table 2. There was a statistically significant difference in immediate postoperative oxygen saturation between the two groups. The median (IQR) was 98.5 (98 to 99) in the intervention group and 98 (96.8 to 98.2) in the control group (P=0.024). However, there was no statistically significant difference in oxygenation at 24 hours after operation (P=0.195).
Regarding to shoulder pain at 24 hours and 48 hours after operation, the mean±SD of shoulder pain at 24 hours after the operation of intervention and control groups were 2.10±2.27 and 1.45±1.73 points, respectively. The shoulder pain at 48 hours after the operation of intervention and control groups were 1.15±1.46 and 0.85±1.73 points, respectively. There were no statistical differences between two groups (P=0.493; 95% CI, −0.61 to 1.91 and P=1.000; 95% CI, −0.96 to 1.56, respectively). There were also no statistical differences in incisional pain at 24 hours and 48 hours after operation between two groups (P=0.698; 95% CI, −0.63 to 1.53 and P=1.000; 95% CI −0.83 to 1.33, respectively), as shown in Table 2. No statistically significant differences in the additional analgesic medications used, such as intravenous morphine or oral acetaminophen, were observed in either group. Only one patient in the control group had subcutaneous emphysema, which resolved spontaneously.
Shoulder pain is a common problem that affects patients after laparoscopic surgery. It delays ambulation and prolonged hospitalization [1]. There are several strategies for reducing shoulder pain after laparoscopic procedure [1]. Pulmonary recruitment is an effective method for significantly reducing shoulder pain, with a pulmonary pressure of 40 cmH2O [7]. However, barotrauma can occur as a consequence of such pressure, even with a low incidence.
Our study applied pulmonary recruitment with low pulmonary pressure (30 cmH2O) to elucidate the differences in shoulder pain between patients who received low-pressure pulmonary recruitment and those who did not. Our study did not show a significant benefit of pulmonary recruitment in reducing shoulder pain at 24 hours and 48 hours after the procedure, similar to the Cho et al. [10], which investigated low pulmonary recruitment (30 cmH2O) with an intra-abdominal pressure of 15 mmHg during the operation.
In contrast, Lee et al. [11] found that the use of pulmonary recruitment with a positive pressure of 30 cmH2O significantly reduced postoperative shoulder pain compared to the control at 24 hours and 48 hours. Moreover, Yilmaz et al. [12] noted that there was a significant benefit of pulmonary recruitment with 30 cmH2O and 15 cmH2O to reduce shoulder pain. The reason why our study was inconsistent with other previous studies might be explained primarily by the differences in intraperitoneal pressure during the laparoscopic procedure, with 12 mmHg in the Yilmaz et al. [12] and 10 mmHg in the Lee et al. [11], while our study and Cho et al. [10] used 15 mmHg. It has been reported that low intra-abdominal pressure during laparoscopic procedures significantly reduces shoulder pain compared to standard intra-abdominal pressure (15 mmHg) presumably due to the reduction of abdominal and diaphragmatic distension from the lower pressure of CO2 insufflation. However, low intra-abdominal pressure during a procedure may cause technical difficulties due to inadequate pneumoperitoneum [1,5,13].
Second, analgesic control in the perioperative setting uses a multimodal approach that varies across settings, potentially affecting shoulder pain. We opted for multimodal analgesia for optimal management in postoperative pain control, which is a key component of enhanced recovery after surgery (ERAS). Early ambulation, stimulation of bowel movement, and shorter hospital stays are the benefits of ERAS [14]. Lee et al. [11] used intravenous patient-controlled analgesia (IV-PCV) as a pain reliever, while our study prescribed parecoxib intravenous injection and oral etoricoxib in a timely manner as around-the-clock pain control, so our pain score might be less than that in a previous study [11] that used IV PCA controlled by the patients themselves. This means that when patients experience pain, they will initiate analgesic medication by themselves, so the pain score may not be as low as around-clock pain control. Multimodal analgesic control using the around-the-clock method can reduce postoperative pain and is an effective and safe alternative to IV-PCA [15]. When the pain score value is too small, near zero baseline, additional pulmonary recruitment may not be necessary but may be a significant benefit in situations with IV-PCA. Potent selective cyclooxygenase-2 inhibiting analgesic medication with around-the-clock pain control (parecoxib intravenous injection and oral etoricoxib, on time) should be prescribed as the analgesic of choice to reduce postoperative shoulder pain.
Regarding adverse events after pulmonary recruitment, there was a statistically significant difference in oxygen saturation immediately after surgery between the two groups (P=0.024); however, it did not appear to be of any clinical significance (98.5 vs. 98). Moreover, oxygen saturation in both groups remained greater than 95%; therefore, no clinical significance was considered.
Other pulmonary complications such as tachypnea, dyspnea or pneumothorax were not detected. It should be noted that the power of this randomized controlled trial may not be adequate to determine the difference in post-gynecological laparoscopic shoulder pain between the additional low-pressure pulmonary recruitment group and the control group. One explanation is that the sample size calculation was based on the assumption of at least 2 point-difference in the pain score. However, the results of the study revealed very low postoperative shoulder pain scores in the control group at 24 hours (1.45) and 48 hours (0.85). Therefore, pulmonary recruitment may not be required to reduce post-operative pain. However, the complications associated with pulmonary recruitment are rare. However, if this occurs, patients may experience serious consequences.
Additional low-pressure pulmonary recruitment after laparoscopic surgery for benign gynecologic diseases to reduce shoulder pain did not show a significant benefit compared to the control group, especially when applied with postoperative around-the-clock administration of analgesics. No complications related to barotrauma with a pulmonary pressure of 30 cmH2O were detected.
Notes
Table 1
Baseline characteristics of the participants
Table 2
Perioperative and postoperative outcomes
References
1. Sao CH, Chan-Tiopianco M, Chung KC, Chen YJ, Horng HC, Lee WL, et al. Pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. J Chin Med Assoc 2019;82:819-26.

2. Deura I, Shimada M, Azuma Y, Komatsu H, Nagira K, Sawada M, et al. Comparison of laparoscopic surgery and conventional laparotomy for surgical staging of patients with presumed low-risk endometrial cancer: the current state of Japan. Taiwan J Obstet Gynecol 2019;58:99-104.


3. Saha S, Roy KK, Zangmo R, Das A, Bharti J, Rai R, et al. Gynecological laparoscopic surgeries in the era of COVID-19 pandemic: a prospective study. Obstet Gynecol Sci 2021;64:383-9.




4. Ortenzi M, Montori G, Sartori A, Balla A, Botteri E, Piatto G, et al. Low-pressure versus standard-pressure pneumoperitoneum in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc 2022;36:7092-113.




5. Radosa JC, Radosa MP, Schweitzer PA, Radosa CG, Stotz L, Hamza A, et al. Impact of different intraoperative CO2 pressure levels (8 and 15 mmHg) during laparoscopic hysterectomy performed due to benign uterine pathologies on postoperative pain and arterial pCO2 : a prospective randomised controlled clinical trial. BJOG 2019;126:1276-85.



6. Madsen MR, Jensen KE. Postoperative pain and nausea after laparoscopic cholecystectomy. Surg Laparosc Endosc 1992;2:303-5.

7. Kietpeerakool C, Rattanakanokchai S, Yantapant A, Roekyindee R, Puttasiri S, Yanaranop M, et al. Pulmonary recruitment maneuver for reducing shoulder pain after laparoscopic gynecologic surgery: a network meta-analysis of randomized controlled trials. Minim Invasive Surg 2020;2020:7154612.




8. García-Fernández J, Canfrán S, de Segura IA, Suarez-Sipmann F, Aguado D, Hedenstierna G. Pressure safety range of barotrauma with lung recruitment manoeuvres: a randomised experimental study in a healthy animal model. Eur J Anaesthesiol 2013;30:567-74.

9. Lovas A, Szakmány T. Haemodynamic effects of lung recruitment manoeuvres. BioMed Res Int 2015;2015:478970.




10. Cho M, Kim CJ, Hahm TS, Lee YY, Kim TJ, Lee JW, et al. Combination of a pulmonary recruitment maneuver and intraperitoneal bupivacaine for the reduction of postoperative shoulder pain in gynecologic laparoscopy: a randomized, controlled trial. Obstet Gynecol Sci 2020;63:187-94.




11. Lee J, Park C, Kim J, Ki Y, Cha SH, Kim JY. Effect of low-pressure pulmonary recruitment maneuver on postlaparoscopic shoulder pain: randomized controlled trial. J Minim Invasive Gynecol 2020;27:173-7.


12. Yilmaz G, Kiyak H, Akca A, Salihoglu Z. Low-pressure pulmonary recruitment maneuver: equal to or worse than moderate-pressure pulmonary recruitment maneuver in preventing postlaparoscopic shoulder pain? A randomized controlled trial of 72 patients. Wideochir Inne Tech Maloinwazyjne 2020;15:519-25.


13. Sroussi J, Elies A, Rigouzzo A, Louvet N, Mezzadri M, Fazel A, et al. Low pressure gynecological laparoscopy (7mmHg) with AirSeal® system versus a standard insufflation (15mmHg): a pilot study in 60 patients. J Gynecol Obstet Hum Reprod 2017;46:155-8.