Cesarean section does not increase the prevalence of allergic disease within 3 years of age in the offsprings
Article information
Abstract
Objective
In this study, we evaluated the prevalence of allergic disease in offsprings delivered via the delivery modes of vaginal delivery vs. planned Cesarean section vs. Cesarean section with labor.
Methods
This study included 175 mother-neonate pairs from Severance Hospital who were enrolled in the Cohort for Childhood Origin of Asthma and allergic diseases study. Information regarding prenatal environmental factors, delivery, and diagnosis of allergic diseases was obtained from a questionnaire and medical record review. Patients with at least 3 years of follow-up data were included in this study. Results were adjusted for sex, birth weight, gestational age at birth, season of birth, neonatal intensive care unit admission, parity, breastfeeding, and maternal factors.
Results
A total of 175 offsprings were eligible for analysis. Among the subjects, 52.0% were delivered by vaginal delivery, 34.3% by planned Cesarean section, and 16.6% by Cesarean section with labor. Fifty-nine offsprings (33.7%) were diagnosed with allergic disease at a median age of 1 year (range 0.5–3 years). The prevalence of allergic disease was not associated with delivery mode after adjusting for confounding variables. Time period from membrane rupture to delivery, duration of the active phase, and the beginning of the pelvic division prior to Cesarean section were not associated with allergic disease development in offsprings.
Conclusion
Cesarean section, irrespective of the occurrence of labor before surgery, did not increase the prevalence of allergic disease in infants up to 3 years of age.
Introduction
The mechanism of how allergic diseases such as asthma, allergic rhinitis, and atopic dermatitis arise has yet to be determined. The number of people suffering from allergic disease since birth is increasing; consequently, the financial burden of the disease is also increasing [1]. It is well studied that the development of allergic and autoimmune disease may be associated with the microbiome environment at birth [23456789]. Currently, one of the popular hypotheses is the hygiene hypothesis [1011], according to which exposure to an environment that is not absolutely hygienic allows a child to develop normal immunity against the microbiome environment [12].
Biasucci et al. [13] suggested that the reduced microbiome stimulation at an early age is related to imbalances in postnatal immune development. Since the maternal vagina is the major microbiome reservoir to which the infant is exposed at the time of birth, the mode of delivery and its relationship with allergic diseases have been studied worldwide [267814]. A meta-analysis showed that the prevalence rate of asthma and allergic rhinitis was 20% higher in offsprings delivered by Cesarean section [15]. The author explained that the increased prevalence rate was due to the lack of exposure to maternal vaginal flora [1516], whereas offsprings delivered by vaginal delivery acquire the normal immunity against allergic disease after the “seeding” of normal microbiota to the gastrointestinal tract [5].
However, the hygiene hypothesis is not universally accepted. Some studies did not find an increased risk of allergic disease among children delivered by Cesarean section compared to that among children delivered by vaginal delivery [1718192021]. McKeever et al. [19] showed that there was no significant association between the incidence of allergic disease in children with the microbiome environment at birth and infections in general such as personal infections, infections in siblings, and the use of antibiotics in early life. McKeever et al. [17] also showed that Cesarean section does not increase the prevalence rate of allergic disease based on data derived from a birth cohort of 24,690 children whose data was contributed to the West Midlands General Practice Research Database.
Previous studies on the mode of delivery and its relationship to allergic diseases dichotomized the study population into the vaginally delivered group and the planned Cesarean section group. It has remained unclear whether offsprings delivered by Cesarean section with labor are prevented from developing allergic diseases because they are exposed to maternal microbiota from the cervix and vagina during labor prior to the operation [415]. Moreover, confounding factors such as parental history of allergic disease and maternal or fetal medical conditions have been generally overlooked [22].
Accordingly, we evaluated the prevalence of allergic disease in offsprings delivered through different modes, i.e., vaginal delivery vs. planned Cesarean section vs. Cesarean section with labor, using national prospective birth cohort data to examine the childhood origin of asthma and allergic diseases. Furthermore, we assessed the effect of various maternal-fetal and obstetrical characteristics on the prevalence of allergic disease in the offsprings.
Materials and methods
1. Study population
A prospective birth cohort study in Korea, the Cohort for Childhood Origin of Asthma and allergic diseases (COCOA) study, recruited participants from November 19, 2007 to December 31, 2015 at 5 medical centers and 8 public health centers in Seoul for antenatal care. The offsprings were tracked from before birth to adolescence. From this registry, 175 mother-neonate pairs who delivered at Severance Hospital were extracted and divided into 3 groups: the vaginal delivery, planned Cesarean section, and Cesarean section with labor groups. In this study, Cesarean section with labor was defined as emergency Cesarean section that was conducted after labor regardless of both the time period from the beginning of labor until delivery and the indication for the operation.
2. Assessment of allergic manifestations
Prenatal environmental factors including mode of delivery, sex of the neonate, gestational age at birth, birth weight, history of allergic disease in both parents, season of birth, and history of admission to the neonatal intensive care unit (NICU) were recorded using a questionnaire. The delivery information was obtained through a medical record review. All infants were regularly followed up at the department of pediatrics for clinical and laboratory evaluations of allergic diseases including atopic dermatitis, food allergy, bronchiolitis, recurrent respiratory tract infection, recurrent wheezing, asthma, and allergic rhino-conjunctivitis, which were diagnosed according to COCOA guidelines and protocols [23]. Data on allergic diseases were collected from medical records, and those offsprings were categorized as the allergy group. The normal group was defined as the offsprings who had not been diagnosed with any allergic disease listed above by up to 3 years postnatally. Offsprings diagnosed with allergic disease were included regardless of their age at diagnosis. Obstetrical characteristics such as the time period between the rupture of membranes to delivery, duration from the active phase to delivery, beginning of the pelvic division (defined as cervical dilatation beyond 8 cm with fetal head station of 0 or more), and indications for emergency Cesarean section were collected from the medical record review.
3. Statistical analysis
The clinical characteristics of the vaginal delivery group, planned Cesarean section group, and Cesarean section with labor group were compared using the χ2 test or Fisher's exact test. To specifically evaluate the influence of the delivery mode, we first made a univariable logistic regression model for maternal-fetal characteristics. For the multivariable logistic regression model, we selected the sex of the offspring that showed a certain tendency among different delivery model groups and the gestational age at delivery with statistical significance in the univariable regression model. The data analysis was performed using SAS version 9.4 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
1. Patient characteristics
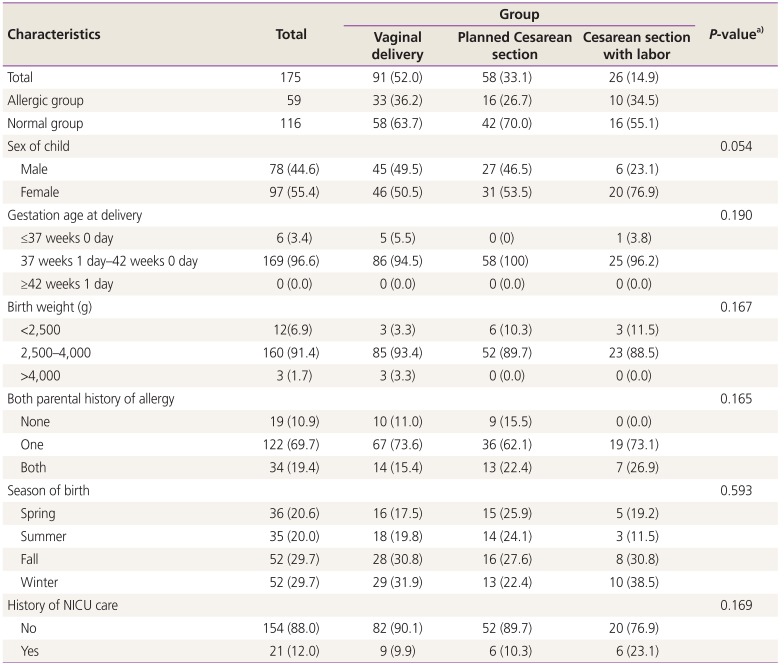
A total of 175 offsprings were eligible for analysis; among the subjects, 52.0% were delivered by vaginal delivery, 34.3% by planned Cesarean section, and 16.6% by Cesarean section with labor. Fifty-nine offsprings (33.7%) were diagnosed with allergic disease at a median age of 1 year (range 0.5–3 years) (Table 1). No significant difference was found between the allergic and normal groups in terms of the maternal-fetal characteristics including the sex of the child, gestational age at delivery, birth weight, parental history of allergic disease, season of birth, and history of NICU admission.
2. Prevalence of allergic disease analyzed by the delivery mode
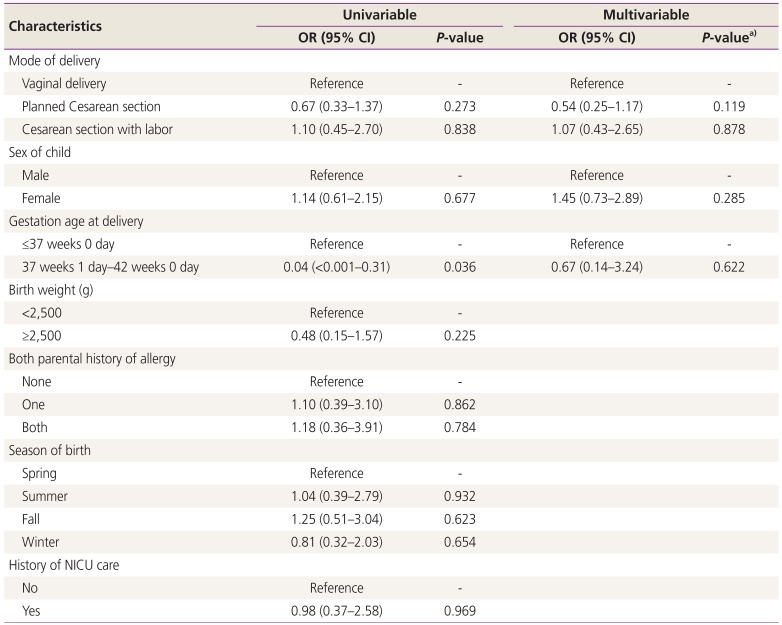
Table 2 shows the univariable and multivariable logistic regression models for the prevalence of allergic disease. Mode of delivery, sex, birth weight, parental history of allergic disease, season of birth, and history of NICU care did not demonstrate an effect on the prevalence of allergic disease. However, delivery at term as compared to preterm was associated with a reduced prevalence of allergic disease (odds ratio, 0.04; 95% confidence interval, <0.001–0.31; P=0.036). When adjusted for the sex of the child and the gestational age at delivery, Cesarean section with or without labor prior to surgery did not increase the prevalence of allergic disease.
3. Obstetrical characteristics of the Cesarean section with labor group
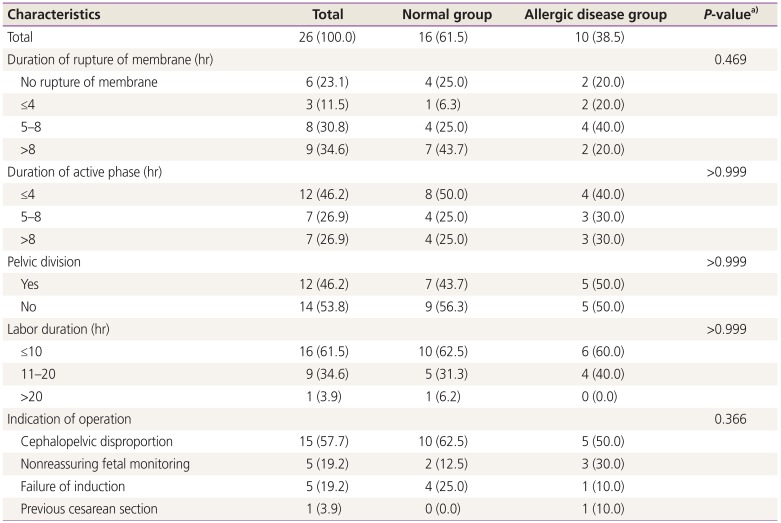
The most common indication for Cesarean section was cephalopelvic disproportion, which accounted for 15 (57.7%) out of 29 infants (Table 3). Cases with prior rupture of the membrane accounted for 76.9%, and we analyzed the time period from the rupture to the delivery. Even though a long period from rupture of the membrane to delivery implies a longer exposure to the vaginal flora, the length of the period was not associated with the prevalence of allergic disease (P=0.47). In addition, we analyzed the association between allergic disease and duration of the active phase and start of the pelvic division of labor. Neither the duration of the active phase nor the start of the pelvic division increased the prevalence of allergic disease. The group with an active phase between 4 and 8 hours and longer than 8 hours developed allergic disease with the same prevalence, 3 (30.0%) out of 10 offsprings, the duration of the active phase was not associated with the prevalence rate of allergic disease (P=0.99). The prevalence of allergic disease in offspring who underwent surgery after the start of the pelvic division was the same as that in offspring who went through surgery before (50%).
Discussion
It remains controversial whether the delivery mode affects the incidence of allergic disease in newborns [2456789101517]. According to a recently published study, delivery by Cesarean section was one of the perinatal characteristics that were not significantly different between children with asthma and those without [24]. According to a recent meta-analysis, on the other hand, birth by Cesarean section can be considered one of the risk factors for childhood allergic disease, as neonates are unexposed to the maternal vaginal microbiota and consequently unable to acquire a normal bacterial population [4]. However, the surgical procedure itself should not be held responsible; rather, if exposure to the vaginal flora at the time of birth is critical to the establishment of an infant's microbiota and long-term health, the prevalence of infant allergic disease should be evaluated irrespective of whether labor had occurred before delivery. Thus, we further divided the Cesarean section group into the planned Cesarean section group and Cesarean section with labor group to compare the prevalence of allergic disease in the offsprings according to delivery mode and found no significant difference.
A few recent studies have distinguished between planned Cesarean section and Cesarean section with labor. Of the 37,171 children included in the Norwegian Mother and Child Cohort Study, those delivered by Cesarean section showed a higher likelihood of current asthma at 36 months of age, and the results were similar for the children delivered by Cesarean section with labor. Two studies based on the Swedish national health registries showed an increased risk of asthma in children delivered by Cesarean section but provided different and conflicting results between the Cesarean section with labor and planned Cesarean section groups [713]. In previous studies analyzing Cesarean section with labor, the maternal or fetal indications for Cesarean section such as preterm labor or preeclampsia were overlooked. Moreover, other medical conditions that may exert effects on the microbiome environment were not assessed [25].
Potential mechanisms to explain the association between birth mode of delivery and subsequent asthma or atopy could involve confounders such as maternal smoking, socioeconomic status, or family history of allergic diseases. Sibling studies provide the chance to study the association between Cesarean section and allergic diseases independent of shared environmental and genetic factors. Pyrhönen et al. [26] had too few siblings to perform this type of control analyses. However, in both studies based on the Swedish national health registries, there was a lack of positive association between Cesarean section and the emergence of allergic manifestations [226]. These results strengthened the argument of recent studies that the microbiome of offsprings is affected by various factors and not merely by exposure to maternal vaginal environment [22].
In 2010, Dominguez-Bello et al. [27] investigated the development of neonatal gut microbiota according to the delivery mode. Their results showed that the gut bacterial taxa of the newborns born vaginally resembled that of the maternal vagina, whereas in Cesarean section, the gut bacterial taxa of the newborns resembled that of maternal skin. Based on their findings, they suggested that the delivery mode affects neonatal microbiota and that this shift in the bacterial communities may impact the infant's health. A subsequent trial to transfer maternal vaginal flora to the neonate at the time of Cesarean section, described as “vaginal seeding,” was conducted [28]. Dominguez-Bello et al. [28] incubated a piece of gauze in the maternal vaginal cavity prior to the surgery; then, the gauze was swabbed on the newborn's mouth, face, and body within 2 minutes of delivery. Interestingly, at 1 month of life, the infants delivered via Cesarean section followed by the vaginal seeding demonstrated similar taxa in oral and skin samples as vaginally delivered infants. Based on this result, they suggested that exposure of the newborn to maternal vaginal fluid at the time of surgery may help establish the optimal microbiota. The vaginal seeding was welcomed by mothers in the hope that such a procedure could prevent allergic disease later in life in Cesarean section-delivered infants [2930].
However, care should be taken when interpreting these studies for the following reasons. First, the effect of delivery mode on the development of allergic disease in offsprings remains controversial [2456789101517]. Second, the study conducted by Dominguez-Bello et al. [27] was a pilot study including only a few cases, and they did not assess the long-term health impacts on offsprings of aberrant microbial colonization due to Cesarean section or restoration of microbiota by vaginal seeding. Third, aberrant bacterial colonization in the very first month of life is not reflective of the microbiota status at later stages of life. Recently, a longitudinal sampling of infants demonstrated that despite a significant difference between the infants’ microbial populations at birth, the microbiome community structure underwent expansion and maturation within the first 6 weeks of life and was ultimately similarly populated irrespective of the delivery mode [31].
Overall, while the delivery mode may affect the infant microbiota immediately after delivery, it is less likely to be associated with the later development of allergic disease in the offsprings. This is in accordance with our finding that the prevalence of allergic disease in the offspring was not affected by the delivery mode or extent of vaginal exposure at the time of birth. Thus, performing a “vaginal seeding” procedure at the time of Cesarean section in an effort to prevent allergic disease is currently not recommended [3233].
In this study, we included not only maternal-fetal characteristics but also the obstetrical characteristics in the analysis. The obstetrical characteristics were rupture of the membrane, duration of the active phase, beginning of the pelvic division of labor, and labor duration before surgery, which may correlate to the degree of exposure of the infant to the maternal vaginal microbial environment. However, we found no significant association between these characteristics and allergic disease prevalence in infants up to 3 years of age. The strength of our study is that this data was archived from a national prospective birth cohort study, COCOA, with prospective and standardized clinical monitoring by pediatricians and obstetricians [23]. However, there is a limitation in that the patients analyzed herein were from a single center; as a result, a small number of mother-offspring pairs were enrolled, especially in the Cesarean section with labor group. Therefore, further studies with a larger sample size are recommended to confirm our findings.
In conclusion, Cesarean section, irrespective of the occurrence of labor prior to the surgery, did not increase the prevalence of allergic disease in infants up to 3 years of age.
Acknowledgements
This research was supported by a fund (2008-E33030-00, 2009-E33033-00, 2011-E33021-00, 2012-E33012-00, 2013-E51003-00, 2014-E51004-00, 2014-E51004-01, and 2014-E51004-02) by the Research of Korea Centers for Disease Control and Prevention.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Ethical approval: The study was approved by the Institutional Review Board (IRB) of Yonsei University Health System, Severance Hospital (IRB No. 4-2017-0355) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent: In the COCOA study, written informed consent was obtained from each mother before the interview. The obtainment of consent was confirmed by Institutional Review Board.