Introduction
Although most obstetric ultrasound examinations are performed to make antenatal diagnoses of fetal abnormalities, the use of ultrasound for women in labor is increasing as a result of accumulating evidence of its usefulness for objectively evaluating the progress of labor.
When progress failure or fetal distress occurs, obstetricians should choose between an operative vaginal delivery or a cesarean section. For the fetus successful instrumental delivery is safer than emergency cesarean delivery. Because the fetal head is impacted deeply in the maternal pelvis, second-stage cesarean section is in association with increased maternal risks such as major hemorrhage, bladder injury, and extension tears of the uterine angle resulting in broad ligament hematoma. Furthermore, cesarean section after failed vacuum extraction is also associated with an increased risk of fetal trauma. The incidence of intracranial hemorrhage with cesarean section following failed operative vaginal delivery is 1/334 compared to 1/860 with successful vacuum delivery [1]. Therefore, it remains to be determined if intrapartum ultrasound can be used to diagnose the presence of abnormal labor and predict the possibility of successful instrumental delivery, consequently improving maternal and fetal outcomes.
As determinants of normal vs. abnormal labor, the specific targets of intrapartum ultrasound are the engagement of the fetal head into the maternal pelvis, fetal head station, the detection of occiput posterior position during labor, and placental separation. In this review, we discuss the usefulness of intrapartum ultrasound for the evaluation of labor progress and predicting successful operative vaginal delivery.
Fetal head position
During labor, the fetus exhibits the cardinal movements of labor, which include engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion. Regarding cardinal movement, ultrasound examination may provide more accurate information about fetal position than digital examination.
In a study of 496 single pregnancies in labor at term, digital examination failed to detect the fetal head position in 166 cases (33.5%); moreover, the digital and sonographic findings were concordant in only 163 cases [2]. Similarly, another study of 112 patients in the second-stage of labor at term with normal single cephalic-presenting fetuses and membrane rupture demonstrated a high rate of error (65%) of the vaginal digital assessment of fetal head position compared to ultrasound assessment as the gold standard [3]. Interestingly, in that study, there was no difference in the technique of senior residents and attending physicians. However, during active labor, attending physicians were almost twice as successful at measuring the correct fetal head position by physical examination. Nevertheless, the discordance rate between vaginal examination and ultrasound assessment was also high (76%) during active labor [4].
The main reason for using sonography to define fetal position is to diagnose persistent occiput posterior position (POPP). POPP is a well-known cause of abnormal labor and occurs in approximately 5% of deliveries and 20% at labor onset. POPP is associated with approximately 4- and 13-fold higher rates of operative vaginal and cesarean deliveries, respectively [5,6]. Occiput posterior position during labor mostly changes to the anterior position even at full cervical dilatation. Nevertheless, most occiput posterior positions at delivery are the initial occiput posterior position rather than misrotation from an original occiput anterior or transverse position [5,6]. Several recent studies support this notion of POPP as the main cause of occiput posterior delivery, although the concept of malrotation of the initial occiput anterior or transverse position for POPP prevailed even until approximately a decade ago [5,7,8].
Blasi et al. [7] suggest that the positions of the head and spine during the second stage of labor could be practical indicators for predicting the occiput posterior position at delivery. In their prospective cohort study, 100 singleton pregnant women underwent intrapartum ultrasound during the first and second stages of labor, and the positions of the fetal head and spine were defined. The rate of occiput posterior position during the first stage of labor was 51%, but the majority of these cases rotated to an anterior position before delivery. There were 6 cases of occiput posterior position at delivery; all of these were among the 23 fetuses in an occiput posterior position during the second stage of labor. With occiput posterior and spine anterior position on ultrasound, none of the babies was born in the occiput posterior position. On the other hand, the fetuses presenting occiput posterior position at delivery also had a posterior spine position during the second stage of labor. If the results of this study are confirmed with larger sample sizes, they could be very helpful for managing POPP pregnancies.
Furthermore, digital pelvic examination is inferior to ultrasound for assessing the fetal head transverse position during labor. In particular, the caput succedaneum related to the deep transverse position decreases the diagnostic accuracy of vaginal digital examination. The transverse position of the fetal head can interrupt fetal descent through asynclitism. A recent study by Malvasi et al. [9] shows that "squint sign" and "sunset of thalamus and cerebellum signs" are 2 simple ultrasonographic signs for anterior and posterior asynclitism, respectively. The most frequent transverse position was the left one, while the most frequent asynclitism was the anterior one. The transverse head positioning with anterior or posterior asynclitism is unlikely to be promoted by drug- or performance-related mechanisms but should rather be a consequence of cephalopelvic disproportion. Furthermore, epidural analgesia does not raise the rate of dystocic labor [10].
Fetal head station
According to the classification of the American College of Obstetricians and Gynecologists, station divides the pelvis above and below the ischial spines into fifths at 1-cm intervals. Zero station means that the lowermost fetal presenting part is at the level of the spines. Meanwhile, station +5 is the status of the fetal head being visible at the introitus. However, the digital examination of fetal head station is unreliable. Dupuis et al. [11] investigated the reliability of digital examination of fetal head station assessed by 32 residents and 25 attending physicians using a newly designed birth simulator mannequin. The error rates of residents and attending physicians were 50% to 88% and 36% to 80%, respectively. Furthermore, caput succedaneum, which forms during labor, can also hinder accurate digital examination of fetal station. Therefore, objective measurements for the engagement and station in labor are required.
Currently used ultrasonographic markers to measure the fetal station during labor include head-perineum distance, angle of progression, fetal head-symphysis distance, intrapartum translabial ultrasound station, and fetal direction.
1. Head-perineum distance
In 2006, Eggebo et al. [12] proposed the head-perineum distance for evaluating fetal head engagement, the time from premature membrane rupture to delivery, and the need for operative delivery. The head-perineum distance is measured by calculating the shortest distance from the perineal skin surface to the outmost bony limit of the fetal skull in a transverse view (Fig. 1). A shorter head-perineum distance was significantly associated with shorter time to delivery, fewer cesarean deliveries, and decreased use of epidural analgesia. The authors state that this parameter is easy to measure even by non-experts and is relatively safe for women with membrane rupture.
2. Angle of progression
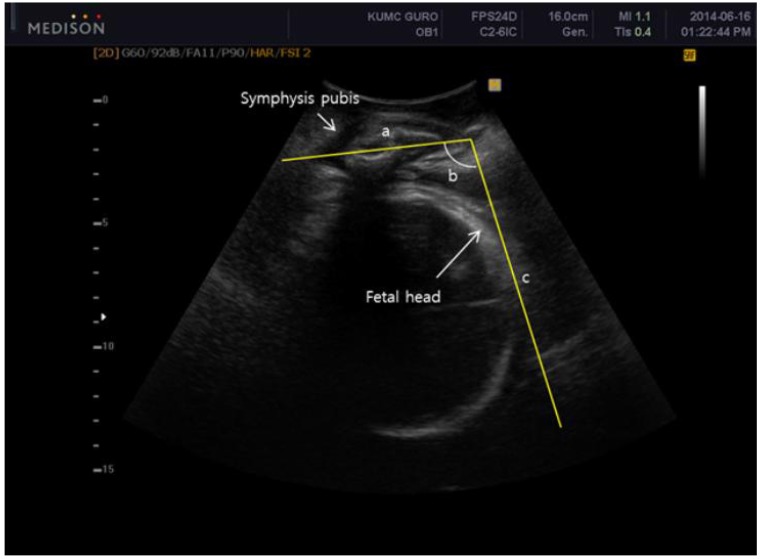
The angle of progression is defined as the angle between a line drawed the midline of the pubic symphysis and a line running from the inferior apex tangentially to the fetal skull (Fig. 2) [13]. The level of the ischial spine is a clinically important indicator of zero station. Barbera et al. [14] developed a geometric model from computed tomographic images of 70 non-pregnant women and measured the angle between the mid-point of the line connecting the 2 ischial spines and the long axis of the symphysis pubis. They found that a transperineal ultrasonographic angle of 99° is correlated with zero station.
Furthermore, Barbera et al. [13] assessed the reproducibility of the angle of progression (they use the term "angle of head descent" instead) in transperineal ultrasound. The analysis of 75 subjects with repeated measurements by the same observer concurrently showed the average standard deviation of intraobserver variability was 2.9°; meanwhile, the interobserver error estimate calculated from 15 assessments with repeated measurements by a second observer was 1.24°. Thus, they conclude that transperineal ultrasound provides an objective, accurate, and reproducible methods for assessing of fetal head station by angle of progression during labor.
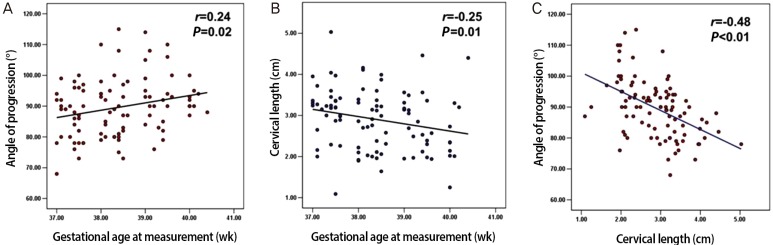
The measurement of the angle of progression may be a novel predictor of spontaneous onset of labor at term. Our data of 77 nulliparous women show that women who experienced spontaneous onset of labor within 7 days had a significantly larger angle of progression than those who underwent labor after 7 days [15]. Logistic regression analysis shows that a larger angle of progression is an independent indicator of spontaneous labor in next 7 days. Furthermore, the angle of progression is negatively correlated with cervical length and positively correlated with gestational age (Fig. 3) [15].
The concept of angle of progression to predict the mode of delivery has been actively researched over the last decade and will be discussed separately in a later section.
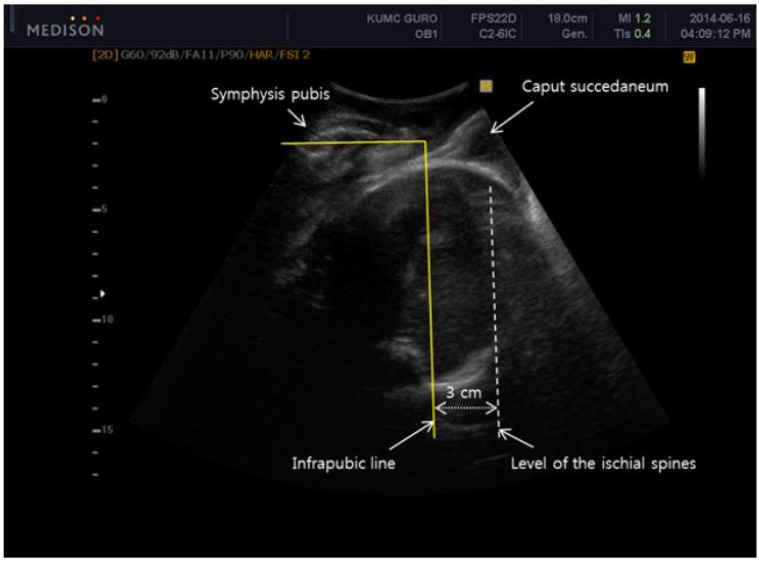
3. Intrapartum translabial ultrasound station
Tutschek et al. [16] suggest using intrapartum translabial ultrasound station to measure fetal station. They measured the longest visible axis of the fetal head between the intersections with the deepest bony part of the fetal head and the infrapubic line; they subtracted 3 cm for the level of the ischial spines, because the infrapubic line indicates the plane 3 cm cranial to a parallel plane crossing through the ischial spines (Fig. 4). The intrapartum translabial ultrasound station is strongly and linearly correlated with the angle of progression according to the following function: head station=angle of progression×0.0937-10.911 [17].
4. Head-symphysis distance
Youssef et al. [18] introduced a new parameter measured by three-dimensional ultrasound: fetal head-symphysis distance. The head-symphysis distance is the distance between the lowest margin of the symphysis pubis and the nearest part of the fetal skull along a line crossing perpendicular to the long axis of the symphysis pubis (Fig. 5). The fetal head-symphysis distance is significantly negatively correlated with both fetal head station assessed by digital examination and angle of progression. Thus, fetal head-symphysis distance is another simple and reliable indicator of fetal head descent in labor. The measurement of head-symphysis distance has high intraobserver reliability (r=0.995, P<0.001) and interobserver reliability (r=0.991, P<0.001).
In a recent study, several ultrasound parameters including intrapartum transperineal ultrasound head station, angle of progression, head-symphysis distance, and head-perineum distance showed good correlations with each other as well as moderate correlations with digital examination for assessing fetal head station [17].
In summary, updated data on intrapartum ultrasound for fetal head engagement and station support its use as a supplementary or alternative tool to digital examination in labor.
5. Head direction
Many authors have aimed to describe fetal head station by using ultrasound landmarks including the head direction with respect to the long axis of the symphysis. Considering the cardinal movement of the fetal head and curved pathway of the pelvis, the concept of head direction is reasonable for assessing station (Fig. 6). As mentioned above, horizontal or downward head direction is associated with poor success for operative vaginal delivery [19]. Ghi et al. [20] report results consistent with previous the previous data. In their study of 60 patients at term gestation with vertex presentation fetuses in the second stage of labor, serial transperineal ultrasound in a sagittal section was performed using digital examination for assessing station. The downward, horizontal, and upward directions of the fetal head were ≤+1, ≤+2, and ≥+3 cm from the ischial spine, respectively. The probability of a station ≥+3 cm was especially high with an upward direction of the head, combined with a rotation <45°.
6. Prediction of normal vaginal delivery vs. operative delivery
One major question in obstetric history is who should undergo unplanned operative interventions. Many researchers have tried to elucidate the predictors of operative delivery. Intrapartum ultrasound has recently been the focus of many investigations. Earlier, we mentioned the angle of progression is a useful tool for assessing fetal station. An interesting study determined if the narrow angle of progression in nulliparous non-laboring women is associated with a higher rate of cesarean delivery at term. Levy et al. [21] performed transperineal ultrasound in pregnant women with no labor at 39 or more weeks of gestation. They compared the angle of progression between women who underwent cesarean section and vaginal delivery as well as between nulliparous and parous women. A narrow angle of progression <95° in nulliparous non-laboring women at term was associated with an increased rate of cesarean delivery. Parous women had a narrower angle of progression than nulliparous women; however, in parous women, this was not associated with cesarean delivery. Our prospective observational study also produced similar results. We measured the angle of progression in nulliparous pregnant women with no labor at ≥37 weeks of gestation who delivered within 1 week of sonography. The angle of progression was compared between women who underwent cesarean and vaginal delivery. The median angle of progression before labor onset was narrower in women who underwent cesarean section than those who delivered vaginally (86.81±5.49° vs. 95.21±10.86°, P<0.001). An angle of progression ≥99° (derived from clinical station "0 or more") was associated with vaginal delivery in 100% of women. This result suggests the angle of progression is an objective and noninvasive method for predicting the delivery mode before labor [22]. Kalache et al. [23] prospectively studied 41 women at term ≥37 weeks with progress failure to the second stage of labor in comparison to the angle of progression on transperineal ultrasound imaging. An angle of progression of 120° lead to the probability of an easy and successful vacuum or spontaneous vaginal delivery in 90%.
Some studies have evaluated the predictors for successful operative vaginal delivery. Henrich et al. [19] used head station and head direction assessed by transperineal sonography during maternal pushing in the second stage of labor as predictors of successful operative vaginal delivery. They propose 3 landmarks with the transducer placed infrapubically: 1) the infrapubic line which extends dorsally from its inferior margin in a mid-sagittal plane, 2) the widest fetal head diameter and its movement regarding the infrapubic line during pushing, and 3) the head direction in relation to the long axis of the symphysis. They show that head-up sign and objective descent of the fetal head under the infrapubic line during maternal pushing result in successful operative delivery. Ghi et al. [20] used the direction and rotation of the fetal head to define fetal station in the second stage of labor in uncomplicated singleton pregnancies at term gestation. Head rotation was categorized as ≥45° or <45° with respect to the angle formed by the echogenic midline of the fetal head and anteroposterior diameter of the pelvis (Fig. 7) [20]. On the sonogram, when the fetal head direction was downward, horizontally, and upward, the most frequent stations were ≤+1, ≤+2, and ≥+3 cm from the ischial spines, respectively (44/57, 77.2%; 53/59, 89.8%; and 46/52, 88.5% of cases; respectively). Failure to detect the cerebral midline or a rotation ≥45° was associated with a station of ≤+2 cm in 98/103 (95.1%) examinations. In comparison, a rotation <45° was associated with a station of ≥+3 cm in 45/65 (69.2%) examinations. Most vacuum extractions were only performed when the clinical station was ≥+2 cm; mostly, the fetal head was directed upward (9/11) in these cases. In the 6 cases with cesarean section, the head direction was horizontal and downward in 4 and 2 cases, respectively; rotation was undetectable or ≥45° in all 6 cesarean cases. Given the simplicity and good predictability for successful vacuum delivery, the head direction and rotation can be easily applied to diagnose obstructed labor.
It was recently revealed that pubic arch angle in prolonged second stage of labor is another significant predictor of delivery mode. For the measurement of pubic arch angle, the transducer is tilted 45° on the perineum to obtain an image showing the pubic symphysis and the 2 symmetrical inferior pubic rami. The angle between the lowermost borders of the pubic rami that converge at the middle of the pubic symphysis is measured. A study of 62 women at ≥37 weeks of gestation who fail to progress in the second stage of labor showed that the probability for operative delivery increased with decreasing pubic arch angle [24].
Obstetricians can choose various ultrasonographic techniques to obtain a successful spontaneous or operative vaginal delivery (Table 1).
Cervical change assessed by elastography
The cervical change, called ripening, occurs in preparation for labor and delivery; it comprises dilatation, shortening, and softening and is essential for labor progress. Regarding labor, ultrasonography of the cervix usually focuses on length. However, many investigators have recently paid attention to softening and stiffness as well. Elastography is a tool for evaluating stiffness on the basis of the estimated displacement of moving tissues while oscillatory pressure is applied. The background physical properties are stress, strain, and deformation. The clinical use of ultrasound elastography for characterizing tissue hardness is increasing because it is better, safer, and easier than other methods. For example, breast elastography is a useful complementary tool for undetermined breast lesions or cystic lesions [25]. Moreover, ultrasound elastography has been used successfully in the diagnosis and classification of breast cancer [26]. Malignant masses evaluated by elastography are usually heterogeneous and irregular; furthermore, they are larger on elastography than on grayscale imaging. Ultrasound elastography was recently introduced in the field of obstetrics. Hernandez-Andrade et al. [27] evaluated cervical stiffness during pregnancy by estimating the average tissue displacement (i.e., strain) within a defined area of interest. A total of 1,557 strains were checked in 262 patients at 8 to 40 weeks of gestation. Their results show the strain is greater in the endocervix than the entire cervix, in the external os than the internal os, and in parous women than nulliparous women. A new method using the quantification of cervical elastographic colors has been introduced as well [27]. However, Molina et al. [28] indicate that this does not mean the measurements of rate-of-change in tissue placement is equal to histological changes in cervical ripening, although this point remains to be clarified. Hwang et al. [29] recently evaluated the ability of cervical elastography for predicting successful labor induction in nulliparous women at term. In their study of 145 women, receiver operating characteristic curves and the areas under the curve for the combination of cervical length, cervical area, mean elastographic index, and cervical hard area were calculated. The combined data of cervical length and elastographic data were more predictive of successful labor induction than any other combination.
Cervical elastography is limited because of the absence of reference tissue in that anatomical area, in contrast to the breasts where adipose tissue is a reliable one [30]. Therefore, it has been difficult to quantitatively compare cervical stiffness among women. Hee et al. [31] report quantitative elastography using Young's modulus (N/mm2), which is the approximate tissue stiffness based on reference caps made of silicone and oil. The Young's modulus of the anterior cervical lip is 0.08 and 0.03 N/mm2 in mid- and full-term pregnant women, respectively. The same group recently evaluated elastographic data using Young's modulus for the prediction of prolonged cervical dilation time. They found that the Young's modulus is associated with cervical dilation time during active labor (P<0.01) and predicts increased cervical dilation time (>330 min) with a sensitivity of 74% and specificity of 69% [32].
Considering the important role of the cervix in normal labor and the technology of elastography to reflect structural changes such as tissue hydration, collagen structure, and tissue elasticity, cervical elastography is promising for predicting successful labor induction [33].
Third stage of labor
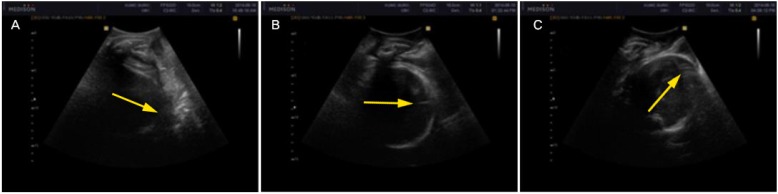
Abnormal placental separation contributes to hemorrhagic morbidity and mortality in pregnancy. The placental separation has been evaluated using ultrasound. Ultrasonographic findings indicate the placental separation is divided into 3 (or 4) phases: the latent, (contraction), detachment, and expulsion phases. The latent phase is the interval between fetal delivery and the beginning of placental separation. The contraction phase is characterized by thickening the placenta site wall. The detachment phase involves monophasic or multiphasic separation of the placenta. Finally, the expulsion phase is the interval between completed separation and vaginal delivery of the placenta. The characteristic finding of normal placental separation is the cessation of blood flow between myometrium and basal placenta after the birth of the fetus; continuous flow on color Doppler between those structures may indicate placenta accreta [34].
The most important issue regarding placental separation is how the separation proceeds. Recent data show that the placental separation is usually an multiphasic phenomenon in sequence that starts mostly from the lower pole of the placenta and spreads upwards. The fundal placenta separates first at the poles and last at the fundal part [35]. Understanding the mechanism of placental separation may help the management of complications in the third stage of labor; ultrasound will undoubtedly play a central role in elucidating this mechanism.
Conclusion
Intrapartum ultrasound not only provides objective and quantitative data in labor, thus expanding knowledge about the pathophysiology of abnormal labor, but also improves obstetric outcomes of both the mother and fetus as a supplementary tool for active management. With increasing resolution and easier accessibility, ultrasound is receiving more and more attention during labor. Practicing obstetricians can use intrapartum ultrasonographic findings on fetal head status (i.e., engagement, station, and position), cervical status (i.e., shortening, dilatation, and softening), and placental separation to make more reliable clinical decisions.