|
 |
- Search
| Obstet Gynecol Sci > Volume 58(6); 2015 > Article |
Abstract
There are few reports of pregnancy complicated by a primary borderline parovarian tumor. A 32-year-old pregnant woman was found to have an ovarian tumor. At 13 weeks of gestation, cystectomy was performed and a diagnosis of primary borderline parovarian tumor was made. At 38 weeks of gestation, she underwent cesarean section combined with a restaging operation. A normal infant was delivered and there were no signs of recurrence. Currently, the patient is being followed for 24 months after the initial treatment and all imaging data show no evidence of recurrence. This report includes a short review of the existing literature on this topic and documents this case in detail. This case demonstrates the appropriate procedure for evaluating and treating a primary borderline parovarian tumor during pregnancy.
A parovarian cyst is a benign tumor that is observed in mesosalpinx in between an ovary and a fallopian tube. primary borderline parovarian tumor is extremely rare and its complication with pregnancy is even rarer. It is almost impossible to diagnose primary borderline parovarian tumor prior to surgery and treatment for this tumor has not been suggested since its biological characteristics have not been addressed due to its rare occurrence. Here, we report a very rare case of observed primary borderline parovarian tumor with a literature review. We observed this case through a histological examination after performing a laparoscopic parovarian cystectomy on a 32-year-old female patient who visited our clinic with an ovarian cystic tumor in the thirteenth week of her pregnancy.
A 32-year-old woman (gravida 2, para 2) at a gestational age of 13 weeks and two days was referred to our hospital after her first trimester ultrasound scan at another institution had revealed a huge ovarian mass. The patient was asymptomatic, denying weight loss and abdominal pain.
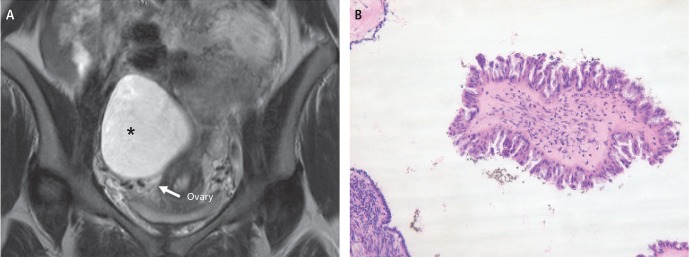
On presentation to our institution, an ultrasonography showed that the fetus had a biparietal diameter of 37 mm, indicating appropriate growth for a 13-week singleton pregnancy and an adnexal mass, measuring approximately 17├Ś12 cm, with a homogenous and unilocular cystic component, arising from the right ovary. Magnetic resonance imaging of the abdomen revealed a homogeneous unilocular parovarian cyst, measuring 17├Ś12├Ś10 cm, located close to the ipsilateral ovary (Fig. 1A). Preoperative investigations (cell blood test, biochemistry, electrocardiogram, chest X-ray, and CA-125) were normal.
A laparoscopy was performed under general anesthesia at 14 weeks of gestation. No ascites were detected. A right parovarian cystic mass, which was the same size as an infant's head and which had an intact capsule, was detected posterior to the uterus. The uterus and the left ovary were normal. A right parovarian cystectomy was performed, and the tumor capsule was not ruptured. A permanent pathological examination demonstrated a borderline serous tumor. A microscopic evaluation revealed papillary epithelial proliferation, which refers to multiple papillary structures lined by serous epithelium showing stratification in some places without nuclear atypia. No stromal invasion was recognized (Fig. 1B).
After the available treatment methods and their possible risks were thoroughly explained and consent was obtained, the pregnancy was allowed to continue under close observation on an outpatient basis.
The remaining weeks of the pregnancy progressed normally and a cesarean section was performed at 38 weeks of gestation and a normal infant weighing 3.2 kg was delivered. After delivering the baby, subsequent restaging surgery was performed. This included a right adnexectomy, omentectomy, appendectomy, peritoneal biopsies, and right pelvic lymphadenectomy. No evidence of disease was found.
The final histology revealed that peritoneal washing and multiple biopsies were negative for malignany, staging the case as IA (International Federation of Gynecology and Obstetrics). Currently, we are monitoring the patient for 24 months following the initial treatment and none of the imaging data shows any evidence of recurrence.
Adnexal mass is one of the most frequent reasons for surgical intervention during pregnancy. Incidence of adnexal mass during pregnancy ranges from 0.2% to 2%. Most of the adnexal masses are functional cysts in pregnancy, and approximately 90% will resolve spontaneously as the pregnancy progresses [1]. Therefore, surgical intervention is not recommended until early in the second trimester. The majority of lesions that persist are benign, and include teratomas, serous cystadenoma, paraovarian cysts, mucinous cystadenoma and endometriomas. Malignant and borderline ovarian tumors are rare during pregnancy [1,2].
A parovarian cyst is found between the ovarian hilus and mesosalpinx, and it is derived from a paramesonephric element, mesothelium, or mesonephric element. Although the formation of a malignant tumor in the parovarium has not been well documented or researched, we made three assumptions as follows. 1) It forms from an existing parovarian cystic tumor. 2) It forms from an endosalpingiotic cyst that is derived from an accessory ovary or supernumerary ovary. 3) It forms from an endosalpingiotic focus within the parovarium [3].
The majority of women with parovarian cyst have vague and nonspecific symptoms, and are usually detected by accident during an examination or laparotomy prescribed for another reason. It can occur in any age group but is usually observed in age between 20s and 30s and rare in preadolescence and in postmenopause.
Approximately less than 5% of ovarian tumors associated with pregnancy are malignant. Despite this, it is very important to evaluate such carcinomas for malignancy because ovarian tumors during pregnancy can become malignant, and early diagnosis and treatment are critical factors for prognosis.
Ultrasonography is often useful in detecting adnexal masses and distinguishing cystic and solid features. At an ultrasound, a paraovarian cyst may be seen as a cyst clearly separate from a normal ovary. Magnetic resonance imaging can provide additional diagnostic information to better distinguish the source, details, and spread of the mass, particularly when the ultrasound examination is equivocal.
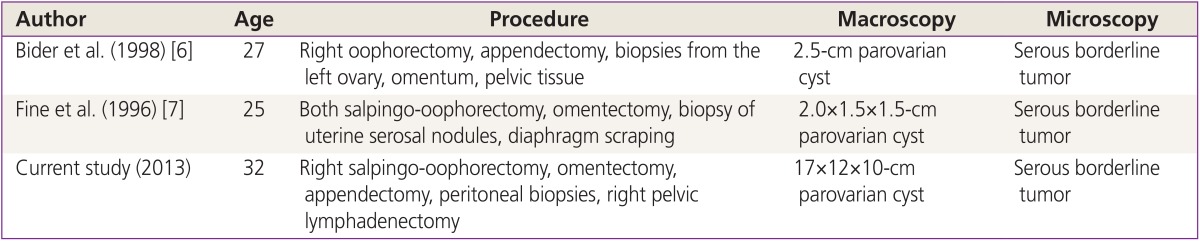
However, it is very difficult to diagnose borderline tumor and malignant tumor in the parovarium before surgery. Its visual inspection is also complicated, but it can be diagnosed using a histopathological method [4]. The pathological diagnosis criteria of a primary borderline tumor in the parovarium are as following. Firstly, it has to be located within the parovarium and be separated from the ovary, fallopian tube and uterus. Secondly, it has to exhibit characteristics of a parovarian cystic tumor under microscopic examination. Finally, it has to show stratification of the papillary surface epithelium, dysplasia of nucleus and cells, and polymorphism and active mitosis of the epithelium, but no infiltration into the cell substrate [5]. Table 1 shows the borderline parovarian tumors published in the literature including our case [6,7].
The biological traits of primary borderline parovarian tumor have not well known because it is extremely rare. Although there are no consistent opinions on its effective treatment, its treatment usually depends on its stage that is classified by the same measure used in ovarian cancer because they share the same affected age and histological appearance and both tumors are derived from coleomic epithelium. For patients who are old enough and do not want a further pregnancy, a total hysterectomy and bilateral salpino-oophorectomy should be performed and omentectomy and lymphadenectomy might be performed if required. On the other hand, for patients who are young and want to maintain their fertility, doctors can try to conserve the uterus and uterine adnexa on the opposite side. However, careful follow-up will be required to detect malignancy if it reoccurs [8,9].
Despite of lack of confident reports on the improved prognosis by additive chemotherapy or radiation therapy after surgical treatment, we recommend chemotherapy and radiation therapy as adjuvant therapy for relapsing or residual disease using the same principles used in the treatment of ovarian cancer [10]. The prognosis of primary borderline parovarian tumor is not well known, but previous literature has reported an approximate 80% to 90% survival rate five years after diagnosis [11]. However, long-term follow-up observation is required due to the high possibility of late relapse, which is also observed in borderline ovarian tumors.
In conclusion, since early diagnosis and the early onset of treatment are important factors for good prognosis in the case of a malignant ovarian tumor, careful physical examinations and ultrasonographic examinations are required throughout pregnancy, especially during the early stage of pregnancy. The best timing for treatment and the best measures should be selected to ensure optimal prognosis and progression of a pregnancy. This requires a thorough evaluation of possible malignancy in patients with ovarian tumors. In addition, additional case reports will lead to further research on the biological and clinical characteristics of primary borderline parovarian tumor.
References
1. Whitecar MP, Turner S, Higby MK. Adnexal masses in pregnancy: a review of 130 cases undergoing surgical management. Am J Obstet Gynecol 1999;181:19-24. PMID: 10411786.


2. Jacob JH, Stringer CA. Diagnosis and management of cancer during pregnancy. Semin Perinatol 1990;14:79-87. PMID: 2180079.

3. Honore LH, O'Hara KE. Serous papillary neoplasms arising in paramesonephric parovarian cysts: a report of eight cases. Acta Obstet Gynecol Scand 1980;59:525-528. PMID: 7457096.


4. Altaras MM, Jaffe R, Corduba M, Holtzinger M, Bahary C. Primary paraovariancystadenocarcinoma: clinical and management aspects and literature review. Gynecol Oncol 1990;38:268-272. PMID: 2201587.


5. Seltzer VL, Molho L, Fougner A, Hong P, Kereszti B, Gero M, et al. Parovarian cystadenocarcinoma of low-malignant potential. Gynecol Oncol 1988;30:216-221. PMID: 3371747.


6. Bider D, Rabinovitch O, Schinder OM, Menczer J. Parovarian serouscystadenocarcinoma of borderline malignancy diagnosed during pregnancy. Gynecol Obstet Invest 1988;26:262-264. PMID: 3240895.


7. Fine BA, Valente PT, Schroeder B. Parovarian borderline malignancy inpregnancy. Arch Gynecol Obstet 1996;258:105-108. PMID: 8779610.


8. Fain-Kahn V, Poirot C, Uzan C, Prades M, Gouy S, Genestie C, et al. Feasibility of ovarian cryopreservation in borderline ovarian tumours. Hum Reprod 2009;24:850-855. PMID: 19098070.


9. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Surgical management of borderline ovarian tumors: the role of fertility-sparing surgery. Gynecol Oncol 2009;113:75-82. PMID: 19171373.


10. Kaur K, Gopalan S, Gupta SK, Dhaliwal LK. Parovarian cystadenocarcinoma: a case report. Asia Oceania J Obstet Gynaecol 1990;16:131-135. PMID: 2378591.


11. Rojansky N, Ophir E, Sharony A, Spira H, Suprun H. Broad ligament adenocarcinoma: its origin and clinical behavior. A literature review and report of a case. Obstet Gynecol Surv 1985;40:665-671. PMID: 4058816.


-
METRICS

-
- 2 Crossref
- 2,502 View
- 27 Download
- Related articles in Obstet Gynecol Sci
-
A case of fetus papyraceus in twin pregnancy.1991 February;34(2)
Three cases of ovarian pregnancy.1992 March;35(3)
Two cases of ovarian pregnancy.1992 April;35(4)
A study for acute pyelonephritis during pregnancy.1992 June;35(6)