 |
 |
- Search
| Obstet Gynecol Sci > Volume 58(1); 2015 > Article |
Abstract
Solitary fibrous tumors (SFTs) are unique soft-tissue tumors of submesothelial origin. These tumors are mainly located in the pleural space but they can be originated within a variety of sites, including the abdomen, the pelvis, the soft tissues and the retroperitoneum. SFTs from all sites are usually benign, and the surgical resection is curative in almost all cases. According to the review of literatures, during the surgical resection, massive hemorrhage could occur due to the hypervascular nature of SFTs. This is a case report on SFT in the pelvis presenting great vessel injury, which resulted in life threatening hemorrhage during the resection of tumor. We wish this paper alerts gynecologists about the risk of massive bleeding during the resection of tumor located at adjacent to great vessels in the pelvis.
Solitary fibrous tumors (SFTs) are uncommon soft-tissue tumors. They usually develop in the pleura. However, according to the case series, extrapleural SFTs can develop in anywhere inside the body, including the retroperitoneum, the deep and soft tissue of proximal extremities, the head and neck, and the abdominal cavity [1]. The paper presents a case of SFT in the presacral area of the pelvis. It describes the experience of unpredictable and uncontrolled intraoperative hemorrhage during the resection. The purpose of this case report is to emphasize the potential risk of severely intraoperative hemorrhage and the importance of thorough preoperative diagnosis and the cautious dissection during the surgery through the reported experience.
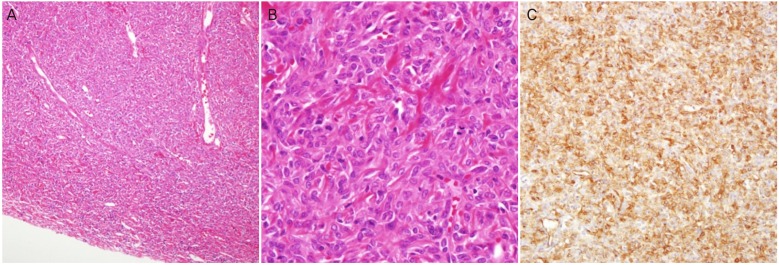
A 52-year-old woman (gravida 1, para 1, and abortion 1) was referred due to the pelvic mass which was found by the transvaginal ultrasound in private clinic. Transvaginal ultrasound demonstrated a large irregularly marginated solid mass in the pelvic cavity. She denied the abdominal bloating and the pain except for the vaginal discharge. Her appetite, bowel and urinary function were normal with no recent weight loss. The medical history was unremarkable; there was no history of the abdominal surgery, gynecologic disorders, and family history was not notable. On the physical examination, there was no palpable mass in the abdomen and the cervix appeared normal. Laboratory tests, including tumor markers (CA-125, CEA, and CA-19-9) were within the normal range. Pelvic computed tomography (CT) revealed a 12×9 cm2, lobulated and well-enhanced mass (Fig. 1). Expected origin was the left ovary and the patient was underwent laparoscopic surgery. On the laparoscopy, the uterus and both sides of adnexa were appeared normal. The tumor was not originated from ovary and located in the presacral retroperitoneal space. The tumor was bluish-colored, and adhered densely to the adjacent tissues. The surface of tumor was fragile to bleed easily during dissection (Fig. 2). Since the mass was large and fixed with adjacent tissue, the mass was removed with several pieces. The frozen section biopsy (FSB) was conducted with those pieces. The FSB test result revealed the stromal tumor which cannot be excluded the chance of malignancy. We decided to the laparotomy considering result of FSB. After midline incision, the whole abdomen, including appendix, liver, and diaphragm, were explored carefully and revealed no other abnormalities. Tumor was adhered to the sigmoid colon on the right side of the pelvis and to the iliac vessels and the ovary on the left side of the pelvis. During the sharp dissection around tumor, the left internal iliac vein was injured. It caused fatally massive hemorrhage. It was hard to identify exact site of the torn vessel which was caused by compressing the left common iliac vein and distal part of left internal iliac vein with two suction tips. Immediately, we called a vascular surgeon for help. The vascular surgeon repaired torn vessel. After the tumor resection, the patient was transferred to intensive care unit. Several hours later, rebleeding occurred. The patient was transferred to other tertiary hospital and underwent second surgery which was successful to repair the vessel injuries of external and internal iliac vein. Grossly, the maximum diameter of the tumor was 12 cm, and the appearance of the tumor was white and lobulated mass encapsulated with fibrous coating. Multifocal degenerative areas were found. Histologically, the tumor showed a richly vascular pattern consisting of large and small vessels lined by a single layer of flattened endothelial cells (Fig. 3A). The tumor was composed of spindle cells arranged patternlessly next to dense collagen. The tumor cells had high cellularity, and it was mild to moderate cytologic atypia. Mitosis was 1/10 on the average in high power fields (HPF) as shown in Fig. 3B. However, focal area showed increased mitotic rate (7/10 HPF). Immunohistochemically, these cells were positive for CD34 (Fig. 3C) but negative for pancytokeratin, smooth muscle actin, desmin, S-100 protein, CD31, factor VIII, c-kit, and HMB45. Finally, the tumor was diagnosed as a SFT with focally malignant feature. The postoperative course was uneventful. The patient had refused any adjuvant treatment and has been followed up for 3 years. There was no clinical evidence of disease recurrence.
SFT was first reported in 1931 by Klemperer and Rabin. It was an uncommon neoplasm originated from pleura but previously referred to as a solitary mesothelioma, or localized fibrous tumor of the pleura, since it generally develops in the visceral and parietal pleura, lung parenchyma, mediastinum or pericardium [1].
Nasal cavity and upper respiratory tract are the most common among extrathoracic locations for these tumors. These tumors are also found in deep soft tissues of the proximal extremities, abdominal cavity, and head and neck [2]. The retroperitoneal location is rare. Less than 30 cases have been reported in the literatures [3].
SFTs usually affect mid-adults in both genders. There were no symptom in thoracic SFTs but in extrathoracic SFTs. Clinical manifestation depends on the location of tumor. It includes local pressure symptom, arthralgia and painless mass. It has been reported that around 5% of SFTs are associated with hypoglycemia due to the secretion of insulin-like growth factors [4].
Although typical SFTs show sporadic or no mitotic figures and mild nuclear atypia, England et al. [5] proposed pathologic criteria of malignant SFT which were high cellularity with crowded and overlapping nuclei and had more than 4 mitotic figures per 10 HPFs. Most SFTs in the literatures were usually benign and about 10% of SFTs had malignant histologic features, but some SFTs with benign histologic feature also behave aggressively while others with a malignant appearance may not [5].
The results of initial report about SFTs were based on pathologic aspects without long-term follow up. Most SFTs in the literatures were usually benign and even with malignant pathologic features, their clinical course were not necessarily correlated with poor prognosis [5]. Hasegawa et al. [6] reported 24 extrathoracic SFTs and 10 of them were located in the retroperitoneum or pelvis. One case displaying malignant histologic feature such as increased cellularity and nuclear pleomorphism, has remained free of recurrence for 14 years, whereas there were 2 cases having the local recurrences and 1 case having the distant metastasis after 7 years. These three cases had had no malignant histologic feature at the time of initial diagnosis.
Recently, malignant extrathoracic SFTs have a higher rate of locoregional recurrence and distant metastasis, and patients with malignant SFTs were at increased risk of death on the report of Cranshaw et al. [7]. They suggested that extrathoracic SFTs with malignant histologic feature have aggressively malignant tumors with a poor prognosis (5-year survival 40%) and that even in the presence of benign histopathological features. Long term follow up is necessary to identify and manage the relatively high rate of recurrent disease.
Immunohistochemistry of CD34 is crucial for diagnosis of SFTs, and Hasegawa et al. [6] suggested the both of Bcl-2 and CD34 immunostaining for making differential diagnosis from spindle cell neoplasia. In this report, tumor was immunoreactive for CD34, and had focal malignant histologic feature such as high cellularity, mild to moderate cytologic atypia and mitosis (1/10 HPF on the average, 7/10 HPF on the focal area).
Characteristic radiologic finding of SFTs is limited in the literature, in the few case series it was reported that well-defined and lobulated mass with well-enhancement was typical finding of SFTs. Wignall et al. [8] reported that radiologic and clinical findings of 3 pleural and 31 extrapleural SFTs; 56% of SFTs had the large tumors > maximum 10-cm-diameter, all tumors had discrete margin, 62% had the lobulated contours, 9% had the local invasions, 79% had heterogenous enhancement patterns and 65% of tumors had strong contrast enhancement. In this report, the tumor exceeding 10 cm in maximal diameter had lobulated contour with strong contrast enhancement.
Surgical resection is mandatory for the treatment of SFTs, but it is often difficult to complete resection due to the hypervascular nature of tumors and collateral vessels. One patient with large SFT in the pelvis died of severe and uncontrolled hemorrhage during surgery in the tertiary care center. In one case of recent reports on SFT in the pelvis, resection was failed in the first operation due to the injury of iliac artery and vein. Postoperative CT revealed that the marked contrast enhancement tumor was having blood supply from internal iliac arteries and terminal branches of inferior mesenteric artery. After the pathologic diagnosis of SFT was accomplished, the tumor was treated by radiation therapy [9]. According to the case series of SFTs, postoperative radiotherapy was given due to the high-grade malignancy, narrow excision margins, large size and rapid growing. Also, patients underwent palliative chemotherapy in the cases of distant metastasis [8]. The patient in this case refused any adjuvant treatment in transferred hospital and was followed up in about a year. Recently, she visited our department for following up and there was no disease recurrence.
Several conclusions could be drawn from this series of patients. The extrapleural SFTs are usually benign entities. SFTs with malignant histologic features may have more chance to have aggressive clinical course than that with benign histologic features. Histologic consultation by expert pathologist is necessary for the accurate diagnosis, and long-term follow up is crucial in order to detect recurrent disease because of the unpredictable clinical course. When gynecologists encounter mass in the pelvis which is lobulated, and has the discrete margin and strong contrast enhancement pattern on imaging study, the SFTs should be suspected. In addition, they should consider that vascular injury resulting in uncontrolled hemorrhage and inadequate resection can be occurred during surgery. The SFTs should be treated by expert surgeons in the tertiary center where vascular surgeons are available.
References
1. Klemperer P, Coleman BR. Primary neoplasms of the pleura: a report of five cases. Am J Ind Med 1992;22:1-31. PMID: 1415270.


2. Takizawa I, Saito T, Kitamura Y, Arai K, Kawaguchi M, Takahashi K, et al. Primary solitary fibrous tumor (SFT) in the retroperitoneum. Urol Oncol 2008;26:254-259. PMID: 18452815.


3. Saint-Blancard P, Jancovici R. Solitary fibrous tumor of the retroperitoneum. Rev Med Interne 2009;30:181-185. PMID: 18538897.


4. Enzinger FM, Weiss SW. Solitary fibrous tumor. In: Enzinger FM, Weiss SW, editors. Soft tissue tumors. St. Louis: Mosby; 1995. p. 1021-1031.
5. England DM, Hochholzer L, McCarthy MJ. Localized benign and malignant fibrous tumors of the pleura: a clinicopathologic review of 223 cases. Am J Surg Pathol 1989;13:640-658. PMID: 2665534.


6. Hasegawa T, Matsuno Y, Shimoda T, Hasegawa F, Sano T, Hirohashi S. Extrathoracic solitary fibrous tumors: their histological variability and potentially aggressive behavior. Hum Pathol 1999;30:1464-1473. PMID: 10667425.


7. Cranshaw IM, Gikas PD, Fisher C, Thway K, Thomas JM, Hayes AJ. Clinical outcomes of extra-thoracic solitary fibrous tumours. Eur J Surg Oncol 2009;35:994-998. PMID: 19345055.


8. Wignall OJ, Moskovic EC, Thway K, Thomas JM. Solitary fibrous tumors of the soft tissues: review of the imaging and clinical features with histopathologic correlation. AJR Am J Roentgenol 2010;195:W55-W62. PMID: 20566782.


9. Wat SY, Sur M, Dhamanaskar K. Solitary fibrous tumor (SFT) of the pelvis. Clin Imaging 2008;32:152-156. PMID: 18313582.


Fig. 1
(A) Contrast enhanced computed tomography; lobulated well enhancing mass in the upper-pelvic cavity is very close to left iliac vessels. (B) Same mass in the mid-pelvic cavity is located around uterus and left ovarian cyst.

Fig. 2
Laparoscopy shows that bluish-colored huge mass is located along the sacrum in the pelvic retroperitoneum.

Fig. 3
(A) The tumor was a circumscribed mass and had many variable sized vessels (H&E, ×100). (B) The tumor was composed of high cellular spindle cells having irregular patterns and moderate cytologic atypia. Mitosis was occasionally seen (H&E, ×400). (C) The tumor cells were reactive for CD34 (×200).
-
METRICS

-
- 14 Crossref
- 2,966 View
- 29 Download
- Related articles in Obstet Gynecol Sci
-
A Case of Vaginal Tuberculosis presenting as Vaginal Cyst.2005 December;48(12)
A case of spontaneous rupture of liver melanoma diagnosed during pregnancy.2006 September;49(9)



















