|
 |
- Search
| Obstet Gynecol Sci > Volume 59(4); 2016 > Article |
Abstract
Objective
Endometriosis is a common gynecological disorder caused by ectopic implantation of endometrial glandular and stromal cells outside the uterine cavity. Among several types of endometriosis, endometrioma is the only subtype that could be determined preoperatively using pelvic ultrasonography, and guidelines recommend pathologic confirmation of endometrioma greater than 3 cm in diameter. However, although surgery is performed in cases of endometrioma, endometrioma has a high cumulative rate of recurrence. Therefore, because determining the possibility of recurrence before performance of initial surgery is important, we examined preoperative factors associated with recurrent endometrioma.
Methods
This was a retrospective, comparative study including 236 patients who visited the outpatient clinic between January 2009 and December 2011. Patients who were pathologically diagnosed with endometrioma were included in this study. They were followed up postoperatively and were divided into two groups according to presence of recurrent endometrioma.
Results
We examined associations between baseline factors and recurrent endometrioma. In multivariate analysis, dysmenorrhea and cyst septation were statistically significant after adjusting with age, parity, surgical staging and postoperative management. We examined cumulative recurrence free survival within cases of recurrent endometriosis, based on the presence of inner cyst septation. The cumulative recurrence free survival was lower in cases with septation.
Conclusion
Our study found that recurrent endometrioma is more likely in patients with inner cyst septation and the recurrence occurred within a shorter duration of time than in patients without inner cyst septation on preoperative ultrasonography. Therefore intensive caution and postoperative long term medical therapy would be appropriate in patients with inner cyst septation on preoperative ultrasonography before undergoing primary surgery for endometrioma.
Endometriosis is a common gynecological disorder caused by ectopic implantation of endometrial glandular and stromal cells outside the uterine cavity [1,2,3]. It is classified according to three pathological categories; peritoneal lesions, deep infiltrative lesions, and ovarian endometriotic lesions [4]. Among these, ovarian endometrioma is the only subtype which can be suspected preoperatively using pelvic ultrasonography. European Society of Human Reproduction and Embryology guidelines recommend pathologic confirmation of endometrioma greater than 3 cm in diameter to exclude malignancies [3].
Although pathological and final diagnosis could only be made after surgery, suspected diagnosis could be made based on clinical symptoms along with ultrasonographic findings, based on typical sonographic findings and improvements in ultrasonographic technologies. Endometrioma can be easily detected, and the recurrence rate is also considerably high. The cumulative rate of endometrioma recurrence is 12% to 30% after 2 to 5 years of postoperative follow up [5,6,7]. Therefore, it is important to determine the possibility of recurrence before performance of the initial surgery.
Many studies have reported on risk factors associated with recurrence of endometrioma after laparoscopic excisions. Associations of age at surgery [8,9], the revised American Society for Reproductive Medicine (r-ASRM) score [5,8,9,10], previous medical treatment [6,9], size of the largest cyst [6], previous operative history due to endometriosis [5], and the r-ASRM adnexal adhesion scores, particularly ovarian adhesion score [11] with high recurrence of the disease have been reported. However, few studies on prognostic factors associated with recurrence of endometrioma on preoperative detailed findings have been reported.
Factors related to operative field and postoperative management have been reported. However discovery of more preoperative factors would be helpful in counseling patients on their future prognosis. Therefore, in this retrospective study, we examined preoperatvie factors associated with recurrent endometrioma.
This was a retrospective, comparative study, including 236 patients who visited the outpatient clinic in Gil Hospital, Gachon Medical School between January 2009 and December 2011. Patients initially suspected of endometrioma using ultrasonography and pathologically diagnosed with endometrioma were included. After the operation, patients were followed up serially and divided into two groups according to presence of recurrent endometrioma (group 1, n=37) or not (group 2, n=199). Patients suspected of endometrioma on peoperative ultrasonography but not diagnosed with pathologically, and who only had endometriotic spots in the pelvic cavity without endometrioma were excluded. Patients who previously underwent surgery due to endometrioma in other hospitals were also excluded because initial information regarding before and during the primary operation was incomplete.
The study was conducted in accordance with the ethical standards of the Helsinki Declaration, and was approved by the Gachon Medical School, Gil Hospital, institutional review board (GCIRB 2015-293).
Data on age, height and weight were collected at the time of the primary operation due to endometrioma. Body mass index was calculated by weight (kg) divided by square meters of height (m2). Serum blood test was performed for measurement of CA 125, and ultrasonography was done to examine uterus and both adnexa. Two experienced sonographers performed sonography of all the enrolled patients using Accuvix-XQ (Samsung Medison, Seoul, Korea), and Voluson E8 (GE Healthcare Korea, Seoul, Korea). Diameter and symmetricity of anterior and posterior uterine walls were measured and the shape was described. A patient was suspected to have adenomyosis when uterine enlargement with multiple, fine, linear areas of attenuation throughout the lesion and poor definition of the endo-myometrial junction were noted. The maximum diameter of endometrioma was measured in centimeters by measuring the largest diameter of the ovarian cyst with diffuse, homogeneous, low-level internal echogenecity. Not only size, but also laterality and features of endometrioma were examined, and described according to the presence of septation and nodularity.
Laparoscopic excision of ovarian endometrioma was performed as follows. Upon entering the pelvic cavity, uterus and both adnexa were examined. If pelvic adhesion was observed, dissection and adhesiolysis were performed initially using a sharp monopolar. The endometriotic ovary was then freed from adjacent adhesion bands and a sharp incision was made superficially on the ovarian cortex so that the cyst wall could be identified. Once the ovarian cyst wall was exposed, the wall was held with tooth forceps and contralateral force was applied in order to strip off the cystic lesion only. To prevent massive active bleeding during ovarian cystectomy, bipolar forceps were used to cause focal coagulation of actively bleeding lesions. Because the incision made on the ovarian cortex was not large, the ovary was not sutured, but it was put together with hemostatic glue (Greenplast kit, Green Cross, Yongin, Korea). Fulguration was performed if endometriotic spots were found in the pelvic cavity.
Operation type was divided according to six categories; right ovarian cystectomy, left ovarian cystectomy, bilateral ovarian cystectomies, right salpingo-oophorectomy, left salpingo-oophorectomy, and unilateral ovarian cystectomy with unilateral salpingo-oophorectomy. Because this study was conducted in order to monitor occurrence of recurrent endometrioma, cases of bilateral salpingo-oophorectomy were excluded. The operative field was examined and data on pelvic adhesion, posterior cul de sac obliteration, laterality of involved ovary, and r-ASRM stage were reviewed. After the operation, serum CA 125 was measured once more 3 months later, and options for adjuvant treatment were classified according to three categories; none, gonadotropin-releasing hormone agonist only, and gonadotropin-releasing hormone agonist with hormone therapy.
Data on patients with recurrent endometrioma were also collected. Associated symptoms, duration of disease free survival, serum CA 125, laterality and maximum diameter of recurrent endometrioma, options and duration of treatment of recurred cases were reviewed retrospectively.
Endometrioma was suspected if a homogeneous hypoechogenic ovarian cyst with a thick wall was visible on ultrasonography. Variations including hyperechogenic intracystic nodules or septations were also examined and recorded. Recurrent endometrioma was defined as an ovarian endometrioma equal to or larger than 3 cm detected on ultrasonography. The last follow up date was considered the last date of visit to the outpatient clinic of the obstetrics and gynecologic department in our hospital, and follow-up duration was calculated in months, from the day of the first visit to the day of the last follow-up.
Continuous data were expressed as mean┬▒standard deviation, and categorical data were expressed as numbers of cases (percentages). Because the number of enrolled patients was small, the Mann-Whitney U-test was performed in univariate analysis to compare differences between non-recurrent group and recurrent group. One-sample t-test was used for analysis of data only on recurrent endometrioma. Univariate analysis was performed to determine possible risk factors for recurrence and factors with P-value <0.05 were included in multivariate analysis using a step-wise variable selection method. In multivariate analysis, logistic regression analysis was performed for identification of significant variables which contribute to recurrent endometrioma. Kaplan-Meier analysis was performed to determine cumulative recurrence free survival depending on presence of septation or nodularity only among patients with recurrent endometrioma, and the log-rank test was performed for comparison of significant differences between the curves obtained in each graph. PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis, and a P-value less than 0.05 was considered statistically significant.
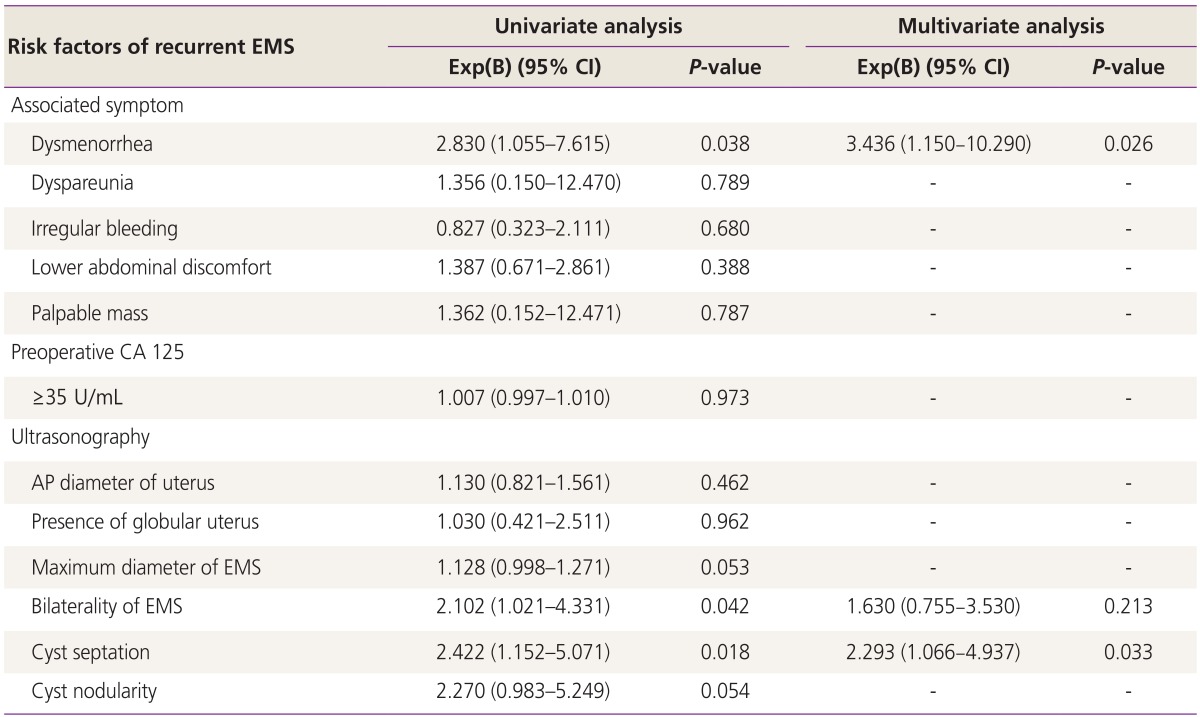
Preoperative baseline characteristics of patients with and without recurrent endometrioma are listed and analyzed (Table 1). Statistically significant difference in body mass index, presence of dysmenorrhea, maximum diameter, bilaterality and side of endometrioma, presence of cyst septation, and follow up duration was observed between the two groups. Patients with recurrent endometrioma were more obese (body mass index, 21.017┬▒3.563 vs. 22.181┬▒37.177 m/kg2; P=0.017), and had dysmenorrhea (69.3% vs. 86.5%, P=0.033). They also had greater maximum diameter of endometrioma (5.693┬▒2.569 vs. 6.611┬▒2.830 cm, P=0.041), higher proportions of bilaterality (27.1% vs. 42.9%, P=0.042) and cyst septation (41.2% vs. 62.9%, P=0.018) as well as longer follow-up period (25.090┬▒15.653 vs. 60.270┬▒32.778 months, P<0.001) than those without recurrent endometrioma.
Intraoperative findings and postoperative management were analyzed according to presence of recurrent endometrioma (Table 2). In sub-classification analysis of operation type, laterality of involved ovary, r-ASRM stage, and adjuvant treatment, no differences were observed between the two groups. However, regarding pelvic adhesion along with posterior cul de sac obliteration, patients with recurrent endometrioma showed higher prevalence than those without recurrent endometrioma (pelvic adhesion, 76.9% vs. 91.9%, P=0.039; posterior cul de sac obliteration, 76.4% vs. 97.1%, P=0.004).
In evaluation of baseline data on patients with recurrent endometrioma, 35.1% of cases with recurrent endometrioma showed no associated clinical symptoms, while the most common symptom was dysmenorrhea (45.9%) (Table 3). The mean duration since the first operation to the point of recurrence was 32.001┬▒3.623 (range, 3 to 84) months and the mean value of serum CA 125 was 51.389┬▒9.344 (range, 8.80 to 226.0) U/mL, including values Ōēź35 U/mL in 37.8% of recurred cases. 83.7% of the cases had unilaterally recurred endometrioma, and the maximum diameter of recurred endometrioma was 6.047┬▒0.393 (range, 3.00 to 8.00) cm in size. When recurrent endometrioma was detected, 45.9% of cases underwent medical treatment, 40.5% underwent both surgical and medical treatment, whereas the rest (13.5%) underwent no treatment at all.
Associations between baseline factors and recurrent endometrioma were examined (Table 4). Multivariate analysis was performed using dysmenorrhea, bilaterality of endometrioma, and cyst septation, which were statistically significant in univariate analysis. Among these three factors, dysmenorrhea (odds ratio, 3.436; 95% confidence interval, 1.150 to 10.290; P=0.026), and cyst septation (odds ratio, 2.293; 95% confidence interval, 1.066 to 4.937; P=0.033) were statistically significant after adjusting with age, parity, surgical staging, postoperative management, and follow-up duration.
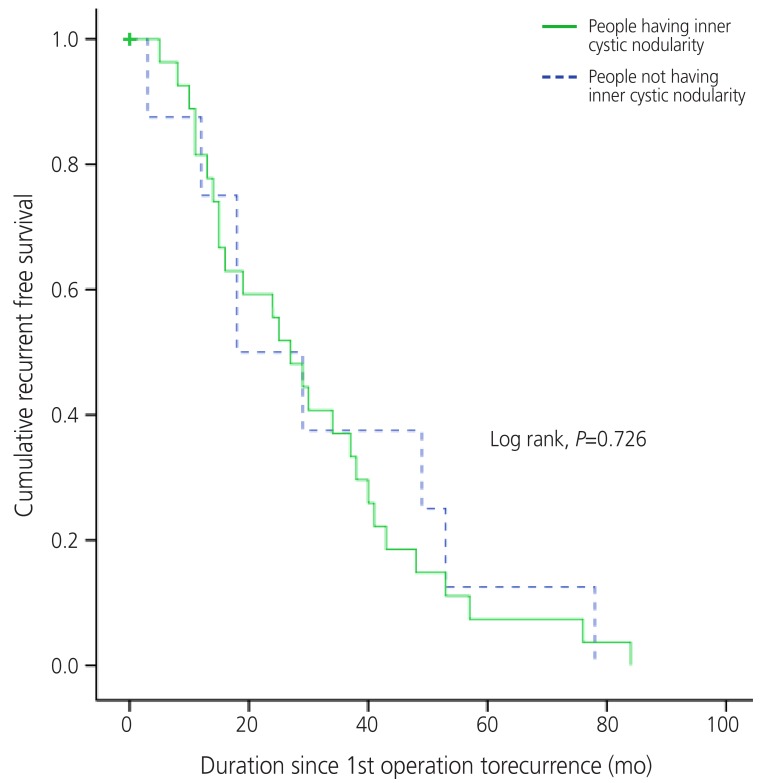
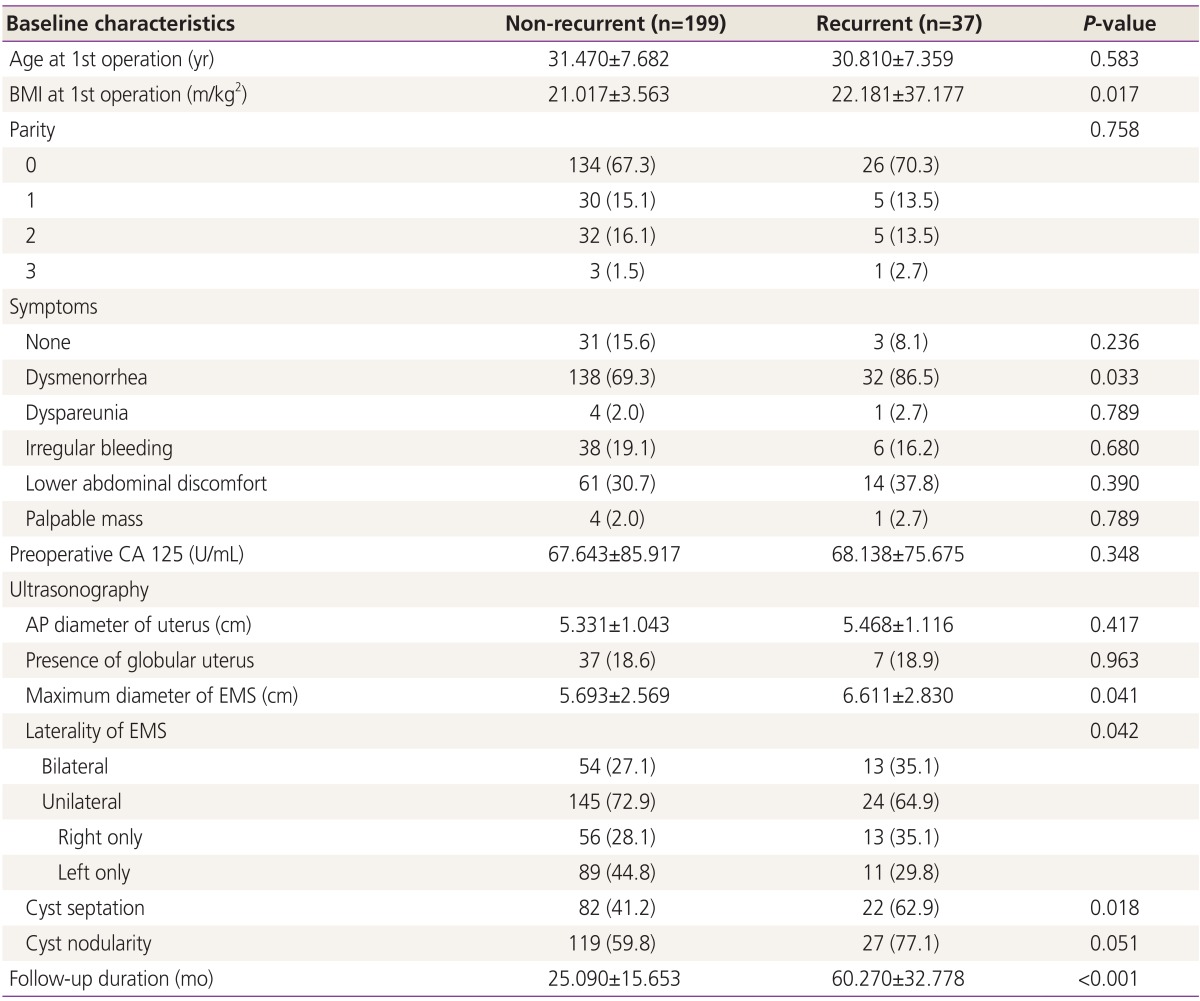
Cyst septation and nodularity were the two ultrasonographically detailed descriptive factors in recurrent ovarian endometrioma in this study. Cumulative recurrence free survivals within recurrent endometriotic cases were examined based on the presence of these two factors each (Figs. 1, 2). The cumulative recurrence free survival was lower in cases with septation (log rank, P=0.003), but it was similar in cases with and without nodularity (log rank, P=0.726).
Our study concluded that the presence of dysmenorrhea and cyst septation on preoperative ultrasonography may be associated with recurrent endometrioma. Among patients with recurrent endometrioma, cumulative recurrence free survivals were significantly different between groups with and without septation. Patients with inner cyst septation showed shorter cumulative recurrence free survival than those in the other group while no statistically significant difference in cumulative recurrence free survival was observed between groups, divided according to presence of nodularities.
Pelvic pain and dyspareunia are the main symptoms related to endometrioma. Pathogenesis of pain related to these symptoms is not generally categorized according to these individualized symptoms, but according to degrees of infiltrated endometriosis; ovarian endometrioma, superficial peritoneal endometriosis and deep infiltrating endometriosis [12]. Deep infiltrating endometriosis, the most severe form may be explained by the significantly decreased apoptosis and increased proliferation activity [12]. However, in cases of recurrent endometriosis, associations between types of endometriosis and various symptoms related to pain have not been elucidated.
Our study showed association of the presence of dysmenorrhea before initial surgery with recurrent endometrioma. Diverse symptoms related to endometrioma are difficult to individualize because they are mostly from homogenous background. Mechanisms of dysmenorrhea have not been uniformly determined, however direct and indirect effects of focal bleeding from endometriotic implants, actions of inflammatory cytokines in the peritoneal cavity, and irritation or direct infiltration of nerves in the pelvic floor are causes [13]. In other words, presence of dysmenorrhea would mean that the disease itself has progressed based on the mechanisms mentioned above. In addition, operating on an endometriotic lesion would only decrease the severity of symptoms and remove visualized cystic lesions, whereas it would not clear basic mechanisms that have occurred and are occurring in the pelvic cavity. This would naturally lead to recurrence of endometriosis in various forms after a certain period of time.
Prevalence of primary endometrioma is known to be higher in the left ovary in patients with unilateral endometrioma [14,15,16,17,18]. Difference in occurrence of laterality due to variations in anatomy and peritoneal fluid flow in a pelvic cavity has been reported [19]. However, results regarding laterality of recurrent endometrioma have been inconclusive. Our study concluded that recurrent endometrioma does not depend on laterality of primary endometriotic lesions, but patients who initially had bilateral endometrioma would have higher recurrence rates. Like our study, one retrospective study reported that frequency and laterality of unilateral recurrent endometriomas were not different between the two sides [20]. On the other hand, a cross-sectional study suggested that recurrence of endometriosis is more likely when advanced stage of endometriosis is located in the left hemi-pelvis. They concluded that this could be due to anatomico-physiological conditions of the genital tract and pelvis, and surgery for primary endometrioma would only treat acute disease, not underlying predisposing factors [19].
To the best of my knowledge, the impact of inner cystic septation in primary endometrioma on endometrioma recurrence has not been a major concern and no study on this issue has been reported to date. In this paper, we found a high correlation between inner cystic septation of primary endometrioma with recurrent endometrioma. From this result, we came up with three possible mechanisms. The first one is that we cannot be certain that we have removed all the inner cystic septations during the operation, especially when the endometriotic cyst has been ruptured and is spontaneously collapsed intraoperatively. The chance of removing inner cystic septations would be higher when the operation is performed with an intact endometriotic cyst. The mechanisms of inner cystic septation are not clearly known, but the second possibility is related to the idea that inner cystic septation would occur due to a combination of two distinct cysts which eventually grew closer and joined together. If inner cyst septation has been made in the above mentioned mechanism, levels of cytokines and inflammatory mediators would be increased in environments having more than one endometriotic cyst. This will eventually cause deterioration of the inner cystic condition, potentiating higher prevalence of recurrence. Last, people having more than one endometriotic cysts would have higher possibilities of having extrauterine implantation of endometrium. Therefore, despite undergoing surgery, the tendency of regurgitating endometrial tissues along with innate immune mechanisms would eventually cause recurrence of endometriotic lesions.
Like this, inner cystic septation may cause a high prevalence of recurrent endometrioma. In addition, we wanted to know whether duration since the first operation to recurrence would be statistically different between the two groups, which were divided according to presence of septation. Based on the value for cumulative recurrence free survival according to presence of septation within recurrent endometrioma cases, cases involving inner cystic septation had a relatively shorter duration since the first operation for detection of recurrent endometrioma than cases without inner cystic septation. This might also be explained based on the mechanisms of recurrence mentioned above. Inner cystic septation may not only cause recurrence in endometriotic lesions, but might also cause acceleration of recurrence.
This study has several limitations. First, it is based on data from a single institution, which might cause selection and measurement bias. Second, in surveying associated symptoms, they were not measured objectively. It would have been better if the symptoms were expressed based on more objective systems such as numeric rating system. Third, in logistic regression analysis, we adjusted with age, parity, surgical staging of endometriosis and postoperative management, which could be factors for recurrent endometrioma. However, for more accurate validity, it would have been better if more factors such as age at menarche, menstrual cycle, smoking, and exercise had been added to the adjusted variables.
Despite the limitations of this study, our finding has clinical importance in counseling patients. Our study found that patients with inner cyst septation have higher possibilities of having recurrent endometrioma, and the recurrence is occurred in a shorter duration of time than in patients without inner cyst septation on preoperative ultrasonography. Therefore, intensive caution and postoperative long term medical therapy would be appropriate in patients with inner cyst septation on preoperative ultrasonography before undergoing primary surgery for endometrioma.
References
3. Kennedy S, Bergqvist A, Chapron C, D'Hooghe T, Dunselman G, Greb R, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod 2005;20:2698-2704. PMID: 15980014.


4. Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil Steril 1997;68:585-596. PMID: 9341595.


5. Busacca M, Marana R, Caruana P, Candiani M, Muzii L, Calia C, et al. Recurrence of ovarian endometrioma after laparoscopic excision. Am J Obstet Gynecol 1999;180(3 Pt 1):519-23. PMID: 10076121.


6. Koga K, Takemura Y, Osuga Y, Yoshino O, Hirota Y, Hirata T, et al. Recurrence of ovarian endometrioma after laparoscopic excision. Hum Reprod 2006;21:2171-2174. PMID: 16644912.


7. Jones KD, Sutton CJ. Recurrence of chocolate cysts after laparoscopic ablation. J Am Assoc Gynecol Laparosc 2002;9:315-320. PMID: 12101328.


8. Kikuchi I, Takeuchi H, Kitade M, Shimanuki H, Kumakiri J, Kinoshita K. Recurrence rate of endometriomas following a laparoscopic cystectomy. Acta Obstet Gynecol Scand 2006;85:1120-1124. PMID: 16929419.


9. Liu X, Yuan L, Shen F, Zhu Z, Jiang H, Guo SW. Patterns of and risk factors for recurrence in women with ovarian endometriomas. Obstet Gynecol 2007;109:1411-1420. PMID: 17540815.


10. Hayasaka S, Ugajin T, Fujii O, Nabeshima H, Utsunomiya H, Yokomizo R, et al. Risk factors for recurrence and rerecurrence of ovarian endometriomas after laparoscopic excision. J Obstet Gynaecol Res 2011;37:581-585. PMID: 21159045.


11. Yun BH, Jeon YE, Chon SJ, Park JH, Seo SK, Cho S, et al. The prognostic value of individual adhesion scores from the revised American Fertility Society classification system for recurrent endometriosis. Yonsei Med J 2015;56:1079-1086. PMID: 26069133.



12. Tosti C, Pinzauti S, Santulli P, Chapron C, Petraglia F. Pathogenetic mechanisms of deep infiltrating endometriosis. Reprod Sci 2015;22:1053-1059. PMID: 26169038.


13. Lee DY, Kim HJ, Yoon BK, Choi D. Factors associated with the laterality of recurrent endometriomas after conservative surgery. Gynecol Endocrinol 2013;29:978-981. PMID: 24004294.


14. Vercellini P, Aimi G, De Giorgi O, Maddalena S, Carinelli S, Crosignani PG. Is cystic ovarian endometriosis an asymmetric disease? Br J Obstet Gynaecol 1998;105:1018-1021. PMID: 9763055.


15. Parazzini F. Left:right side ratio of endometriotic implants in the pelvis. Eur J Obstet Gynecol Reprod Biol 2003;111:65-67. PMID: 14557014.


16. Al-Fozan H, Tulandi T. Left lateral predisposition of endometriosis and endometrioma. Obstet Gynecol 2003;101:164-166. PMID: 12517662.


17. Matalliotakis IM, Cakmak H, Koumantakis EE, Margariti A, Neonaki M, Goumenou AG. Arguments for a left lateral predisposition of endometrioma. Fertil Steril 2009;91:975-978. PMID: 18353324.


18. Bricou A, Batt RE, Chapron C. Peritoneal fluid flow influences anatomical distribution of endometriotic lesions: why Sampson seems to be right. Eur J Obstet Gynecol Reprod Biol 2008;138:127-134. PMID: 18336988.


19. Vercellini P, Busacca M, Aimi G, Bianchi S, Frontino G, Crosignani PG. Lateral distribution of recurrent ovarian endometriotic cysts. Fertil Steril 2002;77:848-849. PMID: 11937148.


20. Ghezzi F, Beretta P, Franchi M, Parissis M, Bolis P. Recurrence of ovarian endometriosis and anatomical location of the primary lesion. Fertil Steril 2001;75:136-140. PMID: 11163828.


Fig.┬Ā1
Cumulative recurrent free survival according to presence of septation within endometrioma in cases with recurrent endometrioma. People having inner cystic septation was associated with recurrence within shorter period of time (log rank, P=0.003) than people without septation.
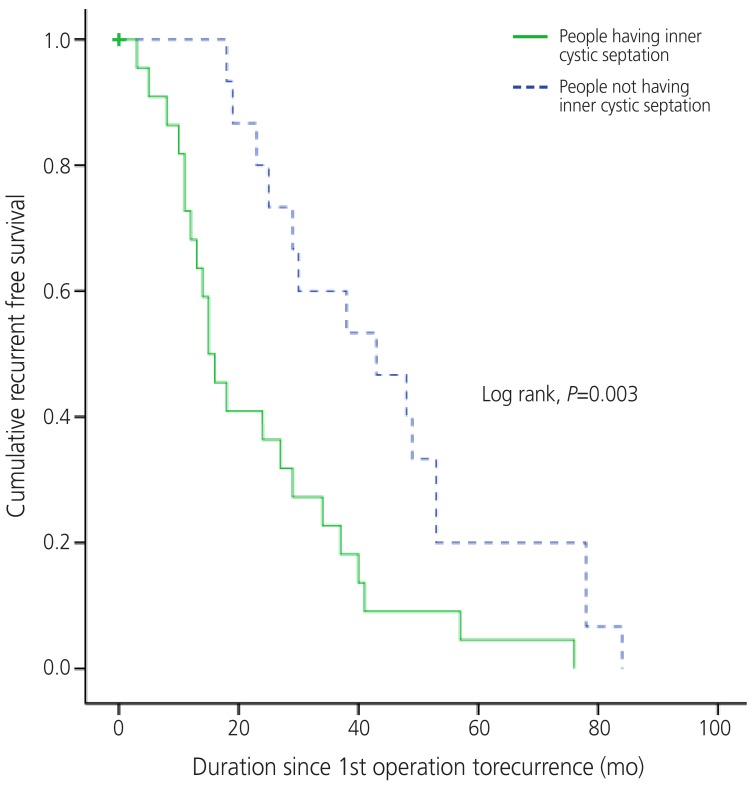
Fig.┬Ā2
Cumulative recurrent free survival according to presence of nodularity within endometrioma in cases with recurrent endometrioma. People with and without inner cystic nodularity had no difference in duration of recurrence since 1st operation (log rank, P=0.726).
Table┬Ā1
Baseline characteristics of patients according to presence of recurrent endometrioma before primary operation
Table┬Ā2
Intraoperative findings in primary operation according to presence of recurrent endometrioma
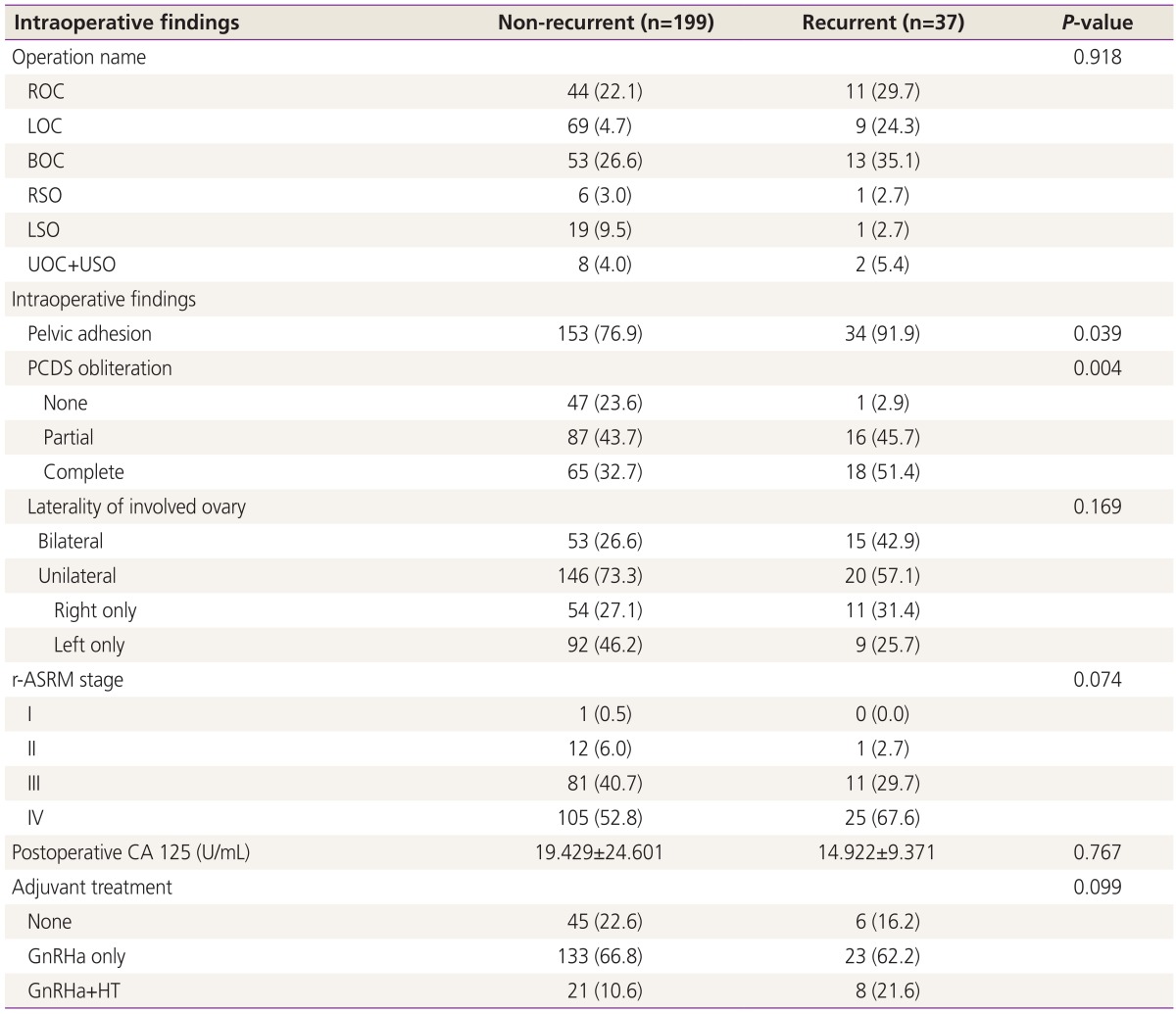
ROC, right ovarian cystectomy; LOC, left ovarian cystectomy; BOC, bilateral ovarian cystectomy; RSO, right salpingo-oophorectomy; LSO, left salpingo-oophorectomy; UOC, unilateral ovarian cystectomy; USO, unilateral salpingo-oophorectomy; PCDS, posterior cul de sac; r-ASRM, revised-American Society of Reproductive Medicine; GnRHa, gonadotropin releasing hormone agonist; HT, hormone therapy.
-
METRICS

-
- 7 Crossref
- 3,233 View
- 28 Download
- Related articles in Obstet Gynecol Sci
-
Prognostic factors in recurrent cervical cancer patients with pulmonary metastasis.2007 June;50(6)