Right ventricular metastatic tumor from a primary carcinoma of uterine cervix: A cause of pulmonary embolism
Article information
Abstract
The presence of intracavitary cardiac metastasis from squamous cell carcinoma of the uterine cervix is extremely rare. The diagnosis is made almost exclusively postmortem. Apart from causing intracardiac obstruction, it can present as pulmonary emboli and the prognosis is extremely poor. It is important to suspect this diagnosis in patient with recurrent pulmonary emboli. Due to the rarity of this condition it is very difficult to standardize care for these patients. However, it is possible that aggressive therapy may lengthen patients' survival and quality of life. We present a case of isolated intracavitary cardiac metastasis arising from a squamous cell carcinoma of the cervix, 44-year-old woman, diagnosed as stage complaint of fatigue and dyspnea on mild exertion. The echocardiogram showed a mass in the right ventricle and suspicious pulmonary embolism. We took an aggressive therapeutic approach. The pathological examination of the resected tissue revealed metastatic squamous cell carcinoma.
Introduction
Cervical cancer frequently spreads to vaginal mucosa and myometrium of the lower uterine segment but the common extrapelvic sites of spread include lungs, bone and supraclavicular lymph nodes [12]. However, cervical carcinoma with cardiac metastasis is very uncommon.
The lung, breast, esophagus, malignant lymphoma, leukemia, and malignant melanoma are the most common tumors spreading to the heart. Cardiac metastases by the cancers occurring around infradiaphragmatic organs are less frequent [3]. The incidence reported in literatures for the metastatic cardiac cancer is about 1.23% [4]. The cardiac metastasis is low because of continuous movement of myocardium, striated cardiac muscle, rapid circulation of blood and lymphatic flow away from the heart.
As already known, there are four pathways for cardiac metastasis. First, retrograde spread by lymph node, second, directly from adjacent viscera, blood circulation and through the vena cava [5]. Even when present, it is difficult to diagnose and represents rapidly fatal condition such as pulmonary embolism. Considering its fatality, the life expectancy after diagnosis is approximately 4 months [2]. Hence it is often difficult to diagnose ante mortem. However, it is important to suspect this diagnosis in patient with recurrent pulmonary embolism. Due to the rarity of this condition, it is very difficult to standardize management. It is possible that aggressive therapy lengthens patients' survival and quality of life. Here, we present a case of cervical carcinoma with metastasis to right ventricle for which she underwent surgical resection but ultimately expired sue to pulmonary embolism.
Case report
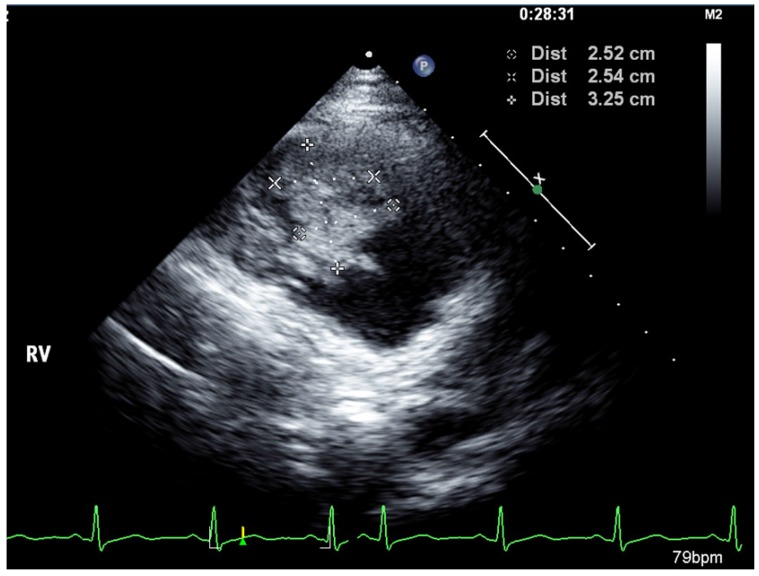
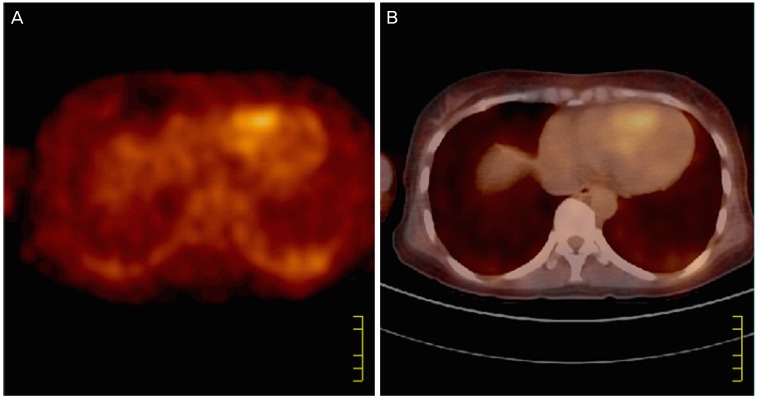
A 44-year-old female presented with vaginal bleeding along with exertional chest discomfort. Vitals signs at the time of presentation were insignificant except for pulse 101 beats per minute with the normal electrocardiogram. However, she had no any past history of cardiovascular disease. Gynecological evaluations revealed cervical cancer (squamous cell carcinoma, stage IVB) which instigated further investigations and evaluations. Whole body positron-emitting tomography computed tomography (PET-CT) (Fig. 1) revealed right ventricular mass possibly malignancy or tumor thrombus with enlarged lymph node in left inguinal area and retroperitoneum without other distant metastasis. For further evaluation of tachycardia and dyspnea occurred a week before visiting the hospital, transthoracic echocardiography (Fig. 2) and pro B-type natriuretic peptide measurement were performed. Pro B-type natriuretic peptide was within the normal range but transthoracic echocardiography revealed right ventricular mass doubtful of malignant mass or tumor thrombus. Hence, she was referred to Department of cardio-thoracic surgery for further evaluation and management. She underwent total bypass surgery and removal of the mass. Histopathology revealed the mass to be a metastatic lesion from the cervical squamous carcinoma. Postoperatively, the patient received 175 mg/m2 paclitaxel (Genexol, Samyang, Seoul, Korea) and 50 mg/m2 of cisplatin for 12 cycles with 3 weeks apart. Until 9th cycle of chemotherapy, there was no relapse of disease which was confirmed by abdomen CT. She then underwent additional 3 cycles of chemotherapy as laboratory test and serum squamous cell carcinoma antigen level (5.2 ng/mL, normal <12.5 ng/mL) reported normal. A contrast enhanced CT was done after additional 3 cycles which unfortunately showed suspicious of newly metastatic lesion in the bladder. She tolerated the chemotherapy well till the 7th cycle only when she started complaining dyspnea on mild exertion. However, echocardiography was normal. Two months after completing 12th cycle, she started to suffer from the dyspnea again. CT scan of chest was performed, which confirmed the increased extent of focal filling defect (thromboembolism) in right pulmonary artery. Echocardiography showed newly developed severe pulmonary hypertension with right ventricular dysfunction. She was then treated with the intravenous heparin because of which she developed severe per vaginal bleeding. Unfortunately, she died of pulmonary embolism fourteen months and 4 weeks from the diagnosis of cardiac metastasis.
Positron-emitting computed tomography of heart taken on August 11, 2008. (A) It shows higher fluorodeoxyglucose uptake of right ventricle comparing the left. (B) The hyper-metabolic lesion due to right ventricular mass.
Discussion
The heart is an uncommon site of metastasis due to relatively less vascularity of endocardium, repeated kneading movement of myocardium, rapid blood circulation and the lack of lymphatic communication of between the surrounding tissues. When, the metastatic cancer is observed from the heart, the most common site is right side like our case. Metastatic lesions are often located in the pericardium when the primary cardiac cancer more commonly found from the endocardium. The spreading route of these cervical carcinomas is hematogeneous through the cervical plexus, inferior vena cava into right atrium finally right ventricle [6].
Due to short survival rate of less than 6 months, diagnosis before death is unusual in compare to benign cardiac tumor. The secondary cardiac tumors progress rapidly resulting systemic symptoms of acute heart failure, which has no standard treatment so far. PubMed and Embase search resulted 19 reported cases. Among them 13 cases were diagnosed ante mortem. The mean age of initial diagnosis of cervical cancer is 48 years old but varies widely from 28 to 78 years. The stage at which the patient is diagnosed also varies widely, ranging from stage I to IV. The mean duration until cardiac metastasis occurs was 4.38 months. For two cases including current case, patients were diagnosed cardiac metastasis synchronously. Therefore, it indicates that during the first year of treatment, the patients should be carefully monitored and followed up. For the patient diagnosed in advanced stage, cardiac evaluation should be done.
When metastasis is observed in intracardiac cavity, common clinical symptoms are dyspnea, arrhythmias, and tachycardia. In our case, the patient suffered from dyspnea a week before visiting hospital. In the early stage of disease, cardiac metastasis was asymptomatic because of their small size. However, when the patient later visited hospital for the symptoms, we were able to detect as a result of increased cardiac uptake of fluorodeoxyglucose. When the patient was further evaluated, the radiologists were not able to confirm the cardiac mass. It is reported that even in an individual, the cardiac uptake of fluorodeoxyglucose by left ventricle differs from that of the right ventricle; this masking causes difficulty in detection of any cardiac mass or lesion [7]. Right ventricle mass was then confirmed through echocardiography. This only emphasizes that for early detection of cardiac lesion, for preventing mortality and morbidity careful confirmation of fluorine-fluorode-oxyglucose uptake and implementation of multiple diagnostic tools are necessary.
The cardiac treatment is limited to conservative management [3]. Concomitance of pulmonary embolism and systemic disease usually results decrease in overall survival period of such patients [8]. The reviews of published papers yielded wide spread presence of argument regarding aggressive treatment but several reports recommend that aggressive treatment lengthens the patients' survival time. In this case, the patient survived for 1.5 years which is longer than the expected survival duration of cervical cancer with cardiac metastasis [910]. Byun et al. [5] reported a case of 32-year-old woman diagnosed with cervical cancer (squamous cell carcinoma) stage IIA2 with exertional dyspnea which was a result of metastatic cardiac mass. The patient was treated with surgical excision followed by chemotherapy with paclitaxel and carboplatin. She survived for 13 months after the diagnosis of cardiac metastasis. In contrast, Tsuchida et al. [10] reported a case of 78 years old women with cervical cancer (squamous cell carcinoma) stage IIIb but they were not able to treat this patient aggressively due to unstable hemodynamic condition and disseminated intravascular coagulation. In our case, when the patient was first diagnosed of cervical cancer with cardiac metastasis, her condition could tolerate both the surgery and chemotherapy. However, later the course of treatment was complicated as anticoagulation therapy caused vaginal bleeding of approximately 900 mL per day. Therefore, the choice of treatment modality for the cardiac metastasis from cervical cancer should be determined on case by case basis [10].
In conclusion, the current studies and literature review, emphasizes that the cardiac metastasis in case of cervical cancer should be considered and evaluated carefully when the patient complains of dyspnea, chest pain, headache and has other nonspecific symptoms. Echocardiography is convenient tool but, combined with PET-CT during initial staging or restaging can increase the possibilities of finding cardiac metastasis in early stages. Moreover, when diagnosed, without systemic disease, aggressive treatment such as surgical resection may help to prolong the overall survival. However, the patient's condition should be considered first when choosing any treatment modality.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.