Comparison of sexual function between sacrocolpopexy and sacrocervicopexy
Article information
Abstract
Objective
To compare sexual function before and 12 months after between sacrocolpopexy and sacrocervicopexy.
Methods
This retrospective study examined a cohort of 55 sexually active women who underwent either supracervical hysterectomy with sacrocervicopexy (n=28) or total abdominal hysterectomy with sacrocolpopexy (n=27) for stage II to IV pelvic organ prolapse. Pelvic floor support was measured with Pelvic Organ Prolapse-Quantification examination. Pelvic floor function was measured with the Pelvic Floor Distress Inventory-Short Form 20 and sexual function was measured with Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire-Short Form 12 (PISQ-12).
Results
Baseline pelvic floor symptoms, demographics and PISQ-12 questionnaire scores were similar between the two groups. Overall improvements in sexual function were seen based on PISQ-12 scores in both groups, but were not statistically significant. No differences were seen in PISQ-12 scores regardless of sparing the cervix or surgical route. Responses to the PISQ-12 question of avoiding sexual intercourse because of vaginal bulging showed significant improvement in both group. No recurrences of prolapse occurred.
Conclusion
In women with pelvic organ prolapse, sexual function after either sacrocolpopexy or sacrocervicopexy was not different. Sexual dysfunction in terms of avoidance of sexual activity because of vaginal bulging was greatly improved in both groups with statistical significance.
Introduction
Pelvic floor disorders (PFDs) affect a large number of women; more than 11% undergo at least one surgery to treat these conditions in their lifetime [1]. Women with PFDs tend to be at high risk for sexual dysfunction. Relatively little information is available about sexual function in women with PFDs or the effects of treatment for PFDs on sexual function. Some studies show poorer sexual function in women with symptomatic PFDs, whereas others show similar rates of sexual function and activity in women with and without PFDs [23]. Also, studies of surgery for PFDs show conflicting results about their impact on sexual function, ranging from improvement to no change to deterioration [45678]. Women's sexuality and sexual function are complex issues that are affected by psychological, physical, social and environmental factors. Anatomical restoration of prolapse and correction of urinary incontinence can contribute women's sexual function. Hysterectomy is the most common procedure for treatment of uterine prolapse. Deterioration in sexual function is reported by 13% to 37% of women after simple and radical hysterectomy [910]. The route of surgical approach and posterior repair can also impact sexual function. In general, an abdominal approach helps preserve vaginal length compared to a vaginal approach. The caliber and length of the vagina is likely to affect sexual function, although the cutoff for these measurements has not been determined. Factors causing dyspareunia after prolapse surgery such as mesh material and posterior repair negatively affect sexual function.
The aims of this study were to compare sexual function and determine changes in anatomical and functional outcomes before and 12 months after between sacrocolpopexy with hysterectomy and sacrocervicopexy with subtotal hysterectomy.
Materials and methods
This is a retrospective study of a cohort of women who underwent prolapse surgery between March 2005 and March 2013 at the Kyung Hee University Hospital at Gangdong. Medical chart review of patients who underwent either supracervical hysterectomy with sacrocervicopexy or total hysterectomy with sacrocolpopexy was performed. This study was exempt from Institutional Review Board approval due to its retrospective nature.
Baseline demographic information was obtained including age, parity, body mass index, medical morbidities and previous history of surgery for PFDs. Pelvic floor support was measured using the Pelvic Organ Prolapse-Quantification (POP-Q) examination: point C refers to the vaginal cuff or cervix support. Point Ba refers to the support of the most distal anterior vaginal wall. Point Bp refers to the support of the most distal posterior vaginal wall. Pelvic floor function was measured with validated, condition-specific quality of life questionnaires: the Korean version of the Pelvic Floor Distress Inventory-Short Form 20 (PFDI-20) and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire-Short Form 12 (PISQ-12) [1112]. PFDI-20 has three subscales that assess symptoms of prolapse, colorectal, and urinary dysfunction, with 100 as the highest possible score on any of the three subscales and 300 as the highest possible total score. Higher PFDI-20 scores indicate more pelvic floor dysfunction or bothersome symptoms. The PISQ-12 assesses the effect of prolapse or incontinence symptoms on sexual function. It comprises three scales assessing the behavioral/emotional domain, physical domain and partner-related domain. Higher PISQ-12 scores indicate a higher level of sexual function with 48 as the highest possible score. Questionnaires were completed preoperatively and at least 12 months after surgery. All patients underwent uroflowmetry, post-void residual urine volume and multichannel urodynamic study; anti-incontinence surgery was added if needed.
Data were analyzed with SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Demographics were assessed with descriptive statistics. Analysis employed the Mann-Whitney U-test, Pearson chi-square test, and Wilcoxon signed-rank test.
Results
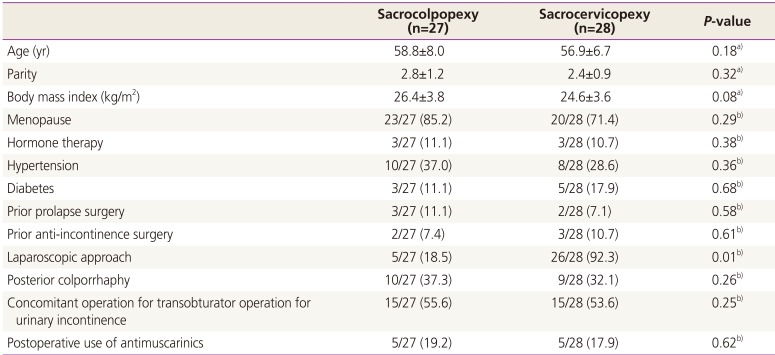
Of 96 women with prolapse over stage II who underwent sacrocolpopexy, 55 sexually active women completed at least one year of follow-up. Of these, 31 (56.4%) had surgery performed laparoscopically. In the study cohort, 27 women underwent total hysterectomy with sacrocolpopexy and 28 underwent supracervical hysterectomy with sacrocervicopexy. Demographic details are shown in Table 1. No differences were seen in age, body mass index, menopausal status, medical morbidities or hormonal use. Also, no differences were seen with regard to previous prolapse, anti-incontinence surgery or concomitant operation for rectocele or urinary incontinence. However, sacrocervicopexy was performed more often with the laparoscopic approach (P=0.01).
The analysis of anatomic outcomes by type of surgery (sacrocolpopexy or sacrocervicopexy) revealed similar results. None of the patients had prolapse recurrence, and both groups showed good postoperative pelvic support at one-year follow-up (P=0.01). And no significant differences were seen when comparing the two groups by POP-Q examination (Table 2). Postoperative vaginal length was significantly increased to 7.4±4.5 and 7.8±4.1 cm in each group, with no difference between the groups. Total pelvic floor symptom questionnaires revealed significantly improved postoperative scores except for bowel symptoms. No difference was observed between the two groups in PFDI-20 scores except for pelvic organ prolapse distress inventory scores. Prolapse distress symptoms were significantly improved in the sacrocervicopexy group (14.1±14.8 vs. 5.1±6.8, P=0.03). We did not identify differences in postoperative PISQ-12 scores within each group or between groups (29.6±5.9 vs. 34.1±5.9, P=0.23).
Analysis of scores for individual items of the PISQ-12 questionnaire, behavioral/emotive domain and partner-related domains did not demonstrate significant differences. Dyspareunia (item 5) scores did not significantly differ between before surgery and one year after within each group and postoperative dyspareunia scores showed no differences (2.5±1.1 vs. 2.6±1.7, P=0.18). Only the score of avoidance of sexual activity due to vaginal bulging was significantly improved one year after surgery in each group and between the two groups (Table 3).
Discussion
In the present study, the score of sexual function was improved a year after either sacrocolpopexy or sacrocervicopexy, based on the validated PISQ-12 questionnaire, but this improvement did not reach statistical significance even though all participants showed improvements in pelvic floor symptoms and none of them had experienced anatomical recurrence. Only the sexual dysfunction due to vaginal bulging was significantly improved and the rate of dyspareunia was not increased at a year after surgery. In attempting to infer from various studies of sexual function after prolapse surgery, the obstacles are reports of a variety of approach to prolapse in different compartment and the use of non-validated questionnaires to assess sexual function. PISQ-12, a short form of PISQ, is a validated questionnaire to assess sexual function in women with PFDs which contains three domains: behavioralemotive, physical, and partner-related [13]. The behavioralemotive domain measures the frequency of sexual activity, orgasm rate and satisfaction with one's sexual relationship. The physical domain examines episodes of pain, incontinence, sensation of prolapse, fear of fecal and/or urinary incontinence during sexual activity. The partner-related domain includes any difficulty with erectile dysfunction or premature ejaculation. The PISQ-12 scores have been known to be well correlated with scores of a general sexual function questionnaire and have a maximal score of 48. The mean PISQ-12 score in the population of sexually active women without bothersome PFDs was 40 [14]. The PISQ-12 questionnaire used in this study is translated into Korean and linguistically validated [12]. The average overall preoperative scores of PISQ-12 in the published articles were better than the scores of in the present study (32 to 34 published articles vs. 29 present study). The sexual function of population in the present study seemed to be more affected by the PFDs. The effect of PFDs on sexuality is still debated. Some studies show poorer sexual function, whereas others show similar rates of sexual function and activity with and without PFDs [31516]. Following the surgery for PFDs, cure of prolapse or incontinence and anatomical restoration can make sexual function to be improved. However, the behavioral/emotive domain which evaluate sexual desire, arousal and orgasmic capabilities and partner-relate domain seem to be not affected by the surgery for PFDs. Also, new physical symptoms such as fecal urgency, swelling and discomfort of abdomen or vagina region and pain can affect sex life after surgery. PISQ-12 did not come up to deal with these aspects of sexual function. It seems that a better tool might be needed in assessment of sexual function after surgery for PFDs.
The role of hysterectomy affecting sexual function has been debated to affect sexual function through lack of uterine contractions, altered perception of orgasm, vagina shortening, damage to nerve endings and loss of symbol of femininity [1718]. Uterine preservation may be another option for selected woman who want keep body image and sexual function. Also, posterior repair can bring improvement of sexual function and no increase in dyspareunia [19]. In the present study, the sexual function of the women who underwent between sacrocolpopexy and sacrocervicopexy was not different. Sparing the cervix and laparoscopic approach did not affect sexual function.
A limitation of the study is low response rate. Only 57.3% of the woman who responded to a questionnaire was analysed in this study. We could not perform power study analysis because the decision of surgical approach was made on the preference of surgeon and study was performed through the retrospective chart review in small cases. Despite these drawbacks, this study showed that sexual function was improved in terms of avoidance of intercourse due to vaginal bulging after sacrocolpopexy and sacrocervicopexy and this improvement was not affected by sparing the cervix, route of surgery. The use of validated condition-specific questionnaire, PISQ-12 helped to bring this study on. In the large case series, more significant findings could be obtained. These informations about sexual function after sacrocolpopexy and sacrocervicopexy can be given in the preoperative counseling and should be included in post-operative outcome evaluation.
In conclusion, sexual function after either sacrocolpopexy or sacrocervicopexy was not different. Sexual dysfunction in terms of avoidance of sexual activity because of vaginal bulging was greatly improved in both groups with statistical significance. The sexual function should be taken into consideration in planning surgery for PFDs and post-operative follow-up. A questionnaire which can reflect complex factors of female sexual function and postoperative new issues affecting sexual function may be needed.
Notes
This is presented with oral presentation in the session of free communication at the 17th annual meeting of Korean Urogynecologic Society, 2014.
Conflict of interest: No potential conflict of interest relevant to this article was reported.