Port site infiltration of local anesthetic after laparoendoscopic single site surgery for benign adnexal disease
Article information
Abstract
Objective
To determine whether local bupivacaine injection into the incision site after gynecologic laparoendoscopic single site surgery (LESS) improves postoperative pain.
Methods
This prospective cohort study included consecutive 158 patients who had LESS for benign adnexal disease from March 2013 to December 2015. Chronologically, 82 patients (March 2013 to August 2014) received no bupivacaine (group 1) and 76 (August 2014 to December 2015) received a bupivacaine block (group 2). For group 2, 10 mL 0.25% bupivacaine was injected into the 20 mm-incision site through all preperitoneal layers after LESS completion. Primary outcome is postoperative pain score using the visual analog scale (VAS).
Results
There was no difference in clinicopathological characteristics between the groups. Operating time (expressed as median [range], 92 [55–222] vs. 100 [50–185] minutes, P=0.137) and estimated blood loss (50 [30–1,500] vs. 125 [30–1,000] mL, P=0.482) were similar between the groups. Post-surgical VAS pain scores after 3 hours (3.5 [2–6] vs. 3.5 [2–5], P=0.478), 6 to 8 hours (3.5 [2–6] vs. 3 [1–8], P=0.478), and 16 to 24 hours (3 [2–4] vs. 3 [1–7], P=0.664) did not differ between groups.
Conclusion
Bupivacaine injection into the trocar site did not improve postoperative pain after LESS. Randomized trials are needed to evaluate the benefits of local bupivacaine anesthetic for postoperative pain reduction.
Introduction
Laparoscopy has several benefits compared to laparotomy in gynecologic surgery including reductions in operative morbidity, recovery time, and hospital stay [1]. There have been continuous efforts to develop less invasive procedures with reduced number and size of incisions. Laparoendoscopic single site surgery (LESS) is a technique in which 3 or 4 laparoscopic instruments are placed through a single umbilical incision [2345]. LESS is widely applicable, safe, and effective for surgical management of benign conditions involving the uterus and adnexa, as well as malignancies [6789101112].
Several randomized trials have reported similar perioperative outcomes following conventional laparoscopy and LESS. However, wound aesthetics was better in the LESS group since the surgical scar is concealed within the umbilicus [1314]. Interestingly, LESS caused similar or worse pain scores compared to conventional laparoscopy [131415]. Hence, optimization of postoperative pain management should be considered in LESS. Several studies investigated various techniques to improve postoperative pain relief after laparoscopic gynecologic surgery, including the injection of local anesthetic agents into the incision sites [1617].
Past studies have shown the effects of local bupivacaine injection on postoperative pain relief of conventional laparoscopic surgery with 3 or 4 laparoscopic ports or after laparotomy [1618192021]. The impact of local bupivacaine injection on postoperative pain after LESS has not been evaluated. Therefore, we evaluated whether injection of local bupivacaine into the umbilical incision site improves postoperative pain after LESS for benign adnexal disease.
Materials and methods
1. Patients
For this prospective cohort study, 158 consecutive patients with benign adnexal diseases who were treated with LESS from March 2013 to December 2015 at our institution were enrolled into a prospective registry designed to assess perioperative outcomes. The registry study was approved by the Institutional Review Board (KUH1040039). Data was accessed anonymously. Inclusion criteria are planned LESS for benign lesions, age ≥18 years, and American Society of Anesthesiologists (ASA) score 1 or 2. Patients were divided into 2 groups, chronologically. From March 2013 to August 2014, 82 patients who underwent LESS did not receive local bupivacaine injection into the incision site and were assigned to group 1. Thereafter to December 2015, an additional 76 consecutive patients who underwent LESS received bupivacaine injection. We evaluated demographic, clinicopathological, and follow-up data of all patients. Each patient underwent preoperative laboratory evaluation including serum cancer antigen-125, physical examination, and pelvic ultrasound or computed tomography.
2. Surgical procedure
All surgeries were performed by a single surgeon (SH Shim). After general anesthesia, the patient was placed in the dorsal lithotomy position. A Cohen cannula was used for uterine manipulation and was handled by the second assistant. An approximately 2 cm intraumbilical skin incision was made, and a single port device (Glove port; Nelis, Bucheon, Korea) was installed transumbilically. Rounded distention of the abdomen after initial pneumoperitoneum was made adequately. The adnexal surgeries were performed with the monopolar or bipolar forceps, atraumatic forceps, scissors, toothed grasper, and a suction-irrigator. The tissue was placed in a 10 mm endobag and removed from the pelvic cavity via the 20 mm incision site. The inserted single port device was removed from the abdominal wall. Group 1 did not receive local injection and group 2 received 10 mL of 0.25% bupivacaine (100 mg) into the 20 mm trocar incision site at the end of LESS. Injecting the local anesthetic through all preperitoneal layers provided a full-thickness local injection. Bupivacaine (0.25%) was injected with a 22G needle. The fascia of the 20 mm puncture site was closed layer by layer with a 2-0 polyglactin suture (Vicryl, Ethicon Inc., Somerville, NJ, USA). The skin was closed by interrupted sutures with 3-0 resorbable monofilament suture (Monosyn, B. Braun, Melsungen, Germany).
3. Postoperative protocol and follow-up
Postoperative pain therapy was composed of either intravenous narcotics via patient-controlled analgesia and/or nonsteroidal anti-inflammatory oral pain medication per the standard postoperative pain medication protocol used at our center. Whenever a patient requested additional analgesics, meticulously registered parenteral analgesics (tramadol hydrochloride, 50 mg intravenously) were given. A 5-day discharge course of thrice-daily oral nonsteroidal anti-inflammatory drugs was dispensed. The postoperative instructions included the specific recommendation to avoid sexual intercourse for 2 weeks after the procedure. The first ambulatory visit was at 1 month after discharge and included an assessment primarily on the surgical wound state and a general physical examination. The patient was asked about food tolerance, the presence of fever, dyspareunia, and evolution of postoperative pain. Subsequent follow-up visits were scheduled at 6 months and 1 year after the surgery and included a physical examination and transvaginal ultrasonography.
4. Outcome measures
The primary outcome was postoperative pain assessed using the visual analog scale (VAS). The secondary outcomes were operating time (initial incision to skin closure), estimated blood loss, transfusion, change in hemoglobin (from before the surgery to the first postoperative day), additional analgesic requirements, and perioperative complications. To evaluate postoperative pain, the patients were asked to rate the intensity of pain using a VAS ranging from 1 (absence of pain) to 10 (worst pain possible) immediately after the surgery in the recovery unit and at 3, 8, 16, and 24 hours after surgery [14]. A registered nurse queried patients about their pain on a regular schedule. To measure blood loss, the aspirator and blood-absorbent gauze were collected and weighed, and the weight of the lost blood was estimated by subtracting the weight of the intact gauze from the total measured weight. Perioperative complications were defined as any adverse event requiring additional medical or surgical therapeutic interventions during surgery and within 30 days after surgery.
5. Statistical analysis
The sample size was calculated before study initiation. This hypothesis was defined by comparing the mean VAS pain scores between the 2 groups. A mean difference between the 2 groups of 2 VAS pain scores was deemed clinically relevant, and the standard deviation was expected to be 3.5, based on the previous published report [17]. Given these assumptions, a sample size of 65 subjects per group provided 90% statistical power to detect a mean difference of 2 VAS pain scores points between the groups at any given time point using a 2-sided test having a significance level of 0.05. Taking into account for potential loss of patients to follow-up, a total of 158 patients were recruited.
Normally distributed continuous variables were presented as means (standard deviations). Non-normally distributed variables were presented as medians (ranges or interquartile ranges). Mean values between the groups were compared using Student's t-test for normally distributed data or the Mann-Whitney U-test for non-normally distributed data. Frequency distributions were compared using a χ2 test or Fisher's exact test. A P-value <0.05 according to 2-sided tests indicated a significant difference. All analyses were performed using SPSS, version 19.0 (SPSS Inc., Chicago, IL, USA).
Results
During the study period, a total of 158 patients who underwent LESS for benign adnexal disease met inclusion criteria (76 received bupivacaine block, and 82 did not). Table 1 summarizes the clinical characteristics of patients in both groups. The median age was 29 vs. 33 years in groups 1 and 2. The median body mass index was 21.1 and 21.3 kg/m2 in groups 1 and 2, respectively. There was no difference in preoperative size of adnexal mass and bilaterality between the 2 groups. The most common pathology was a mature cystic teratoma followed by endometriotic cyst in both groups.
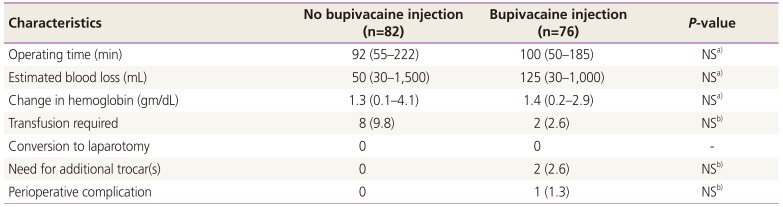
No cases required conversion to laparotomy in both groups. An additional trocar was required for 2 patients in group 2. Operating times (expressed as median [range], 92 [55–222] vs. 100 [50–185] minutes, P=0.137) and estimated blood losses (50 [30–1,500] vs. 125 [30–1,000] mL, P=0.482) were similar between the groups. Perioperative complications occurred only in one patient in group 2 (Table 2). The patient had postoperative ileus that was conservatively managed.
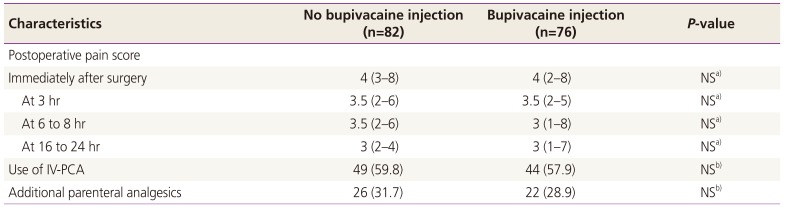
Post-surgical VAS pain scores after 3 hours (expressed as median [range], 3.5 [2–6] vs. 3.5 [2–5], P=0.478), 6 to 8 hours (3.5 [2–6] vs. 3 [1–8], P=0.478), and 16 to 24 hours (3 [2–4] vs. 3 [1–7], P=0.664) did not differ between the groups (Table 3). Moreover, additional analgesics required was similar between the groups (26/82 [31.7%] vs. 22/76 [28.9%], P=0.790).
Discussion
Pain is expected after all surgical procedures; nonetheless, it is undesirable [22]. Effective management of postsurgical pain is related to shortened hospital stay, earlier mobilization, reduced costs, and patient satisfaction. Therefore, the management of postoperative pain should be considered as one of the priorities in routine surgical practice.
In the present study, the injection of bupivacaine in the incision site did not improve postoperative pain after LESS for benign adnexal disease. No significant difference was found in secondary outcomes including operating time and estimated blood loss. Although postsurgical local anesthetic injection is commonly practiced during laparoscopic surgery, this study indicates that local anesthesia might not provide a significant reduction in postoperative pain compared with no anesthetic injection.
To the best of our knowledge, the present study is the first prospective cohort study that evaluates the effect of local bupivacaine injection on pain after gynecologic LESS. Gynecologic studies evaluating the effect of local anesthesia injection on pain after conventional laparoscopic procedures have yielded varying results [1623242526]. Theoretical backgrounds for the use of local anesthetic are blocking the input of noxious stimuli that trigger neuronal excitability and inhibiting the nervous system sensitization [24]. Several studies have shown the benefit of bupivacaine in reducing postoperative pain after conventional laparoscopic gynecologic surgery or mini-laparotomy when intraperitoneal administration is used [1721]. Meanwhile, the incisional sites injection alone did not demonstrate significant benefit [1627]. These outcomes correlate with our results.
One reason for not finding statistically significant pain relief was that the use of local anesthetics injection into the port site had a limited focus of action at the port site. While this may be important, the factors which induce postoperative pain after laparoscopic surgery are variable. Peripheral and central sensitization, intra-abdominal trauma, residual pneumoperitoneum, and phrenic nerve irritation by residual carbon dioxide can also result in pain, in addition to incisional trauma at port sites [2829]. Infiltration of trocar sites with a local analgesic probably does not reduce the severity of alternative sources of pain. This could confound the results of the study.
Other pain-relieving laparoscopic techniques studied so far included intraperitoneal aerosolization of bupivacaine and heated humidified insufflation gas [3031]. Of these, a recent meta-analysis reported that intraperitoneal analgesia in laparoscopic gastric procedures and cholecystectomy minimizes overall pain and opioid use [32]. Like these procedures, visceral pain after gynecologic surgery may gain analogous benefit from intraperitoneal analgesia. Laparoscopic gynecologic surgeries are often performed to treat endometriosis and/or pelvic pain, which are reflected in pelvic nerve density and distribution, hence they are different from the common visceral pain of general surgery [33]. According to a recent randomized trial, multimodal analgesia with combined ropivacaine administration (port-site injection plus intraperitoneal nebulization) may be effective for postoperative pain relief in conventional laparoscopic adnexal surgery but not in uterine surgery [34].
This study has several limitations worth noting. This study was performed in a single institution and all surgeries were performed by a single surgeon, which may limit the generalizability of the present findings. However, this could also be viewed a strength since this protocol avoided inappreciable variations such as differences in surgical techniques between different institutions or surgeons, and also provided reliability of outcomes with consistency. As pain is a subjective finding, patient self-reporting is the best indicator of pain. Thus, this study deliberately used individual patients' pain assessment to act as their own control, which also served to control confounding variables like a history of chronic pelvic pain. Another limitation of the study is its non-randomized study design feature. Although all the consecutive patients undergoing LESS are included in the analysis and the clinicopathological variables are well-balanced between the 2 groups, we could not control confounding factors inherent in observational studies. The outcomes of the present study should be interpreted with caution and be confirmed in future randomized trials.
In conclusion, the use of local bupivacaine anesthesia does not significantly improve postoperative pain relief in gynecologic LESS. Future randomized controlled trials are needed to further elucidate the effects of local bupivacaine anesthetic in terms of postoperative pain. Further studies using a wide range of gynecologic surgeons may add generalizability to the study procedure.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.