Conceptualized framework for levels of obstetric care
Article information
Abstract
It has been demonstrated that risk-appropriate perinatal and obstetric care can improve perinatal morbidity and mortality. Recently, various studies focus on the importance of evaluation for maternal conditions and allocation of high risk pregnant women to highly qualified facilities. Therefore, it is necessary to develop the conceptualized framework for levels of obstetric care and establish the guidelines for the situations that should be cared in each level of facility. In this review article, we reviewed several classifications of obstetric care in eastern and western countries, and conditions in which transfer should be recommended depending on the risk and capacity of centers.
Introduction
It is obvious that to initiate timely appropriate management can improve maternal and fetal outcomes in obstetric care. The role of health care providers is critically important for the better prognosis in obstetric care. Medical doctors, especially obstetricians must make decision clearly and promptly whether to manage at their institution or to transfer to high level facilities in each obstetric patient. If they decide that their institution is not appropriate for managing pregnancy woman or fetus in any reason because of facility system, lack of delivery system, operation room or blood bank, unavailability of medical and/or surgical anesthesia consultation or intensive care unit (ICU), then they should transfer the patient without any delay.
It has been demonstrated that timely appropriate transfer can improve the neonatal outcomes [1]. The survival of preterm birth infants were higher when they were delivered in higher level of hospitals than that in lower level of hospitals and the differential outcome persisted even after neonatal period, suggesting the importance of maternal transport [23]. These evidences support the necessity for classification system of maternal care, which is complementary but different from that in neonatal care.
In this review, we will compare classification systems of obstetric care facilities in eastern and western countries and the evaluation system of maternal/obstetric severity to determine the necessities of transfer in both inpatient and outpatient obstetric services.
Classification systems of obstetric care facilities
The range of medical care may vary depending on each level of health care center's capacity to manage pregnant woman and fetus. Therefore, it is essential to evaluate an institution's management capacity based on its facility, device, and medical personnel.
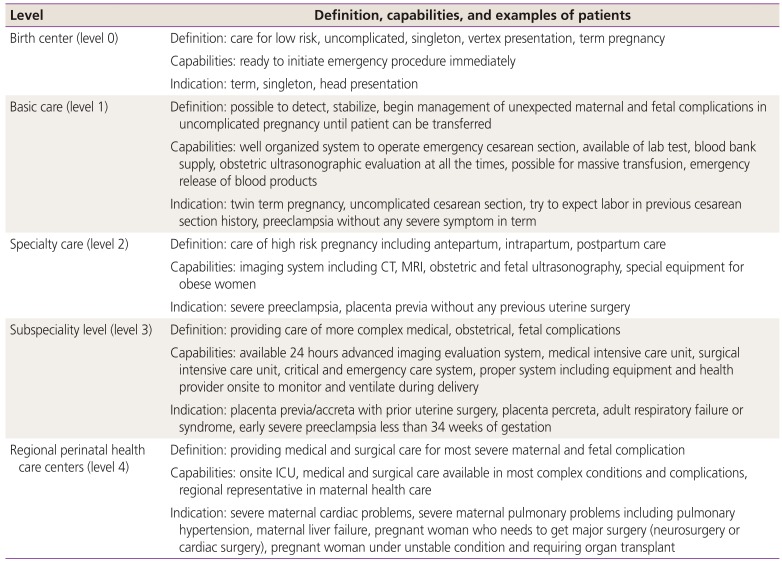
In USA, most states have developed regional systems on perinatal care, but they are using inconsistent systems of classification and definitions [456]. To develop standardized care, American College of Obstetricians and Gynecologists (ACOG) and Society for Maternal-Fetal Medicine suggested uniform classification system for levels of maternal care [7]. This system includes birth centers, basic care, specialty care, subspecialty care, and regional perinatal health care centers. The definition and requirements for each center are summarized in Table 1.
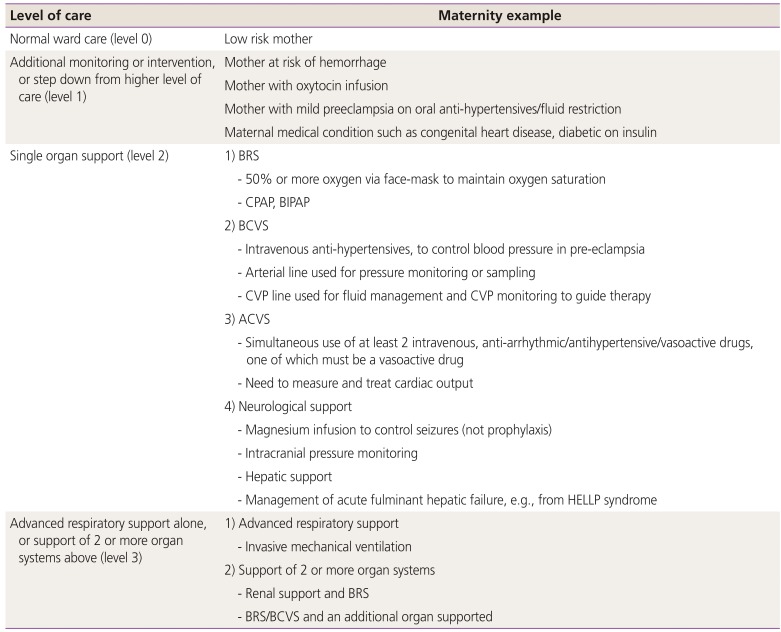
In UK, multidisciplinary working group developed models of maternal care in 2011. Several committee including Royal College of Obstetricians and Gynaecologists, British Maternal and Fetal Medicine Society, Royal College of Midwives, Obstetric Anaesthetists Association, Royal College of Anaesthetists, Intensive Care Society, Department of Health participated in developing maternal health care system and the results are shown in Table 2 [89].
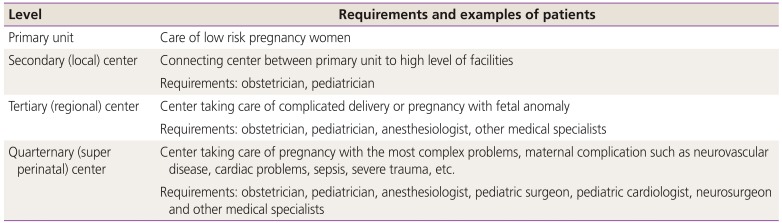
Japan has established proper transfer system between integrated centers for high-risk pregnancy. In Japan, there are 4 levels of facilities in prenatal care system; primary unit, secondary (local) center, tertiary (regional) center, quarternary (super perinatal) center. The requirement for each center is shown in Table 3 [101112].

Maternal-fetal triage index (modified from American College of Obstetricians and Gynecologists 2016)
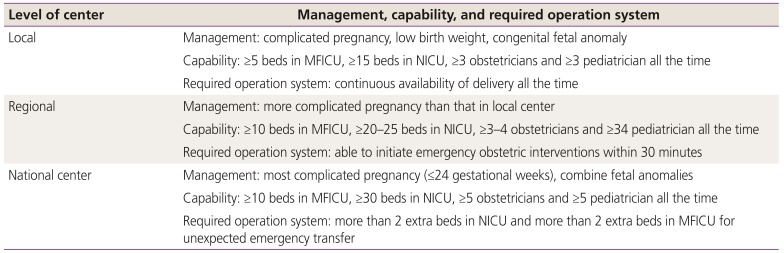
In Korea, maternal-neonatal integrated center system was also suggested by Park [12] and Lee [13] in 2015. In this report, the importance of nationwide transfer system for integrated approach was emphasized for high-risk pregnancy woman and infant care. This report proposed the necessity of classification in perinatal care depending on capabilities of obstetric and pediatric department. Three levels of maternal care system suggested are shown in Table 4 [1213].
Evaluation of pregnant women in inpatient services
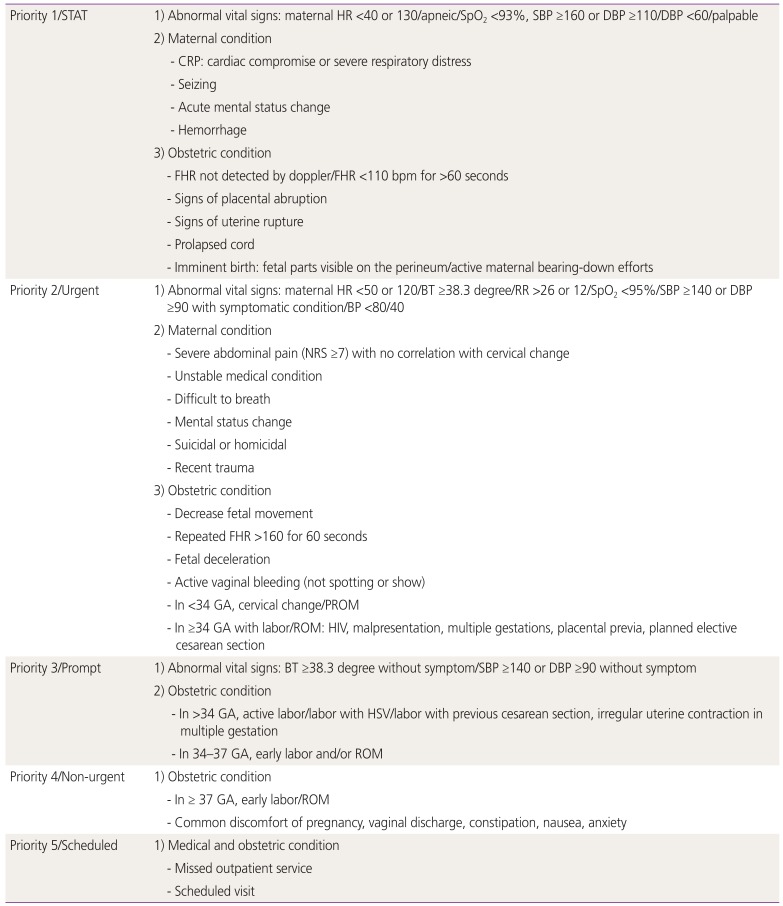
Pregnant women can visit any levels of facilities, and health care providers in maternal care should be qualified for determination of pregnant women. In evaluation of pregnant women who visit emergency department or labor/delivery unit, ACOG addressed the necessity for the development of hospital-based triage of pregnant patients [14]. In the suggested maternal-fetal triage index, patients are classified into 5 levels, according to their condition (Table 3).
According to this triage, obstetrician should decide the appropriate location and timing of treatment, based on the urgency of obstetric problem and the risk and benefit of transfer; whether the patient is unstable and needs prompt treatment, or the patient is stable but need transfer for management in high level of maternal care, or she is stable and can be treated in their unit [1516]. For example, patients with placental abruption at 37 weeks of gestation may need emergent cesarean delivery at the initial hospital, whereas patients with premature preterm rupture of membranes at 32 weeks of gestation without active labor pain can be transferred to high level facilities for neonatal ICU care.
Before making a decision, obstetricians should stabilize the patient or transfer the patient to higher level of facilities immediately. Every patient must be transferred only when the benefits outweigh the risks [1718]. Two other factors should be considered in order to make a proper decision regarding transfer. First, all of the process was initiated after informed consent. Second, when transfer to high level facilities is decided, the patient is under the care by qualified personnel with proper transportation equipment.
Evaluation of pregnant women in outpatient services
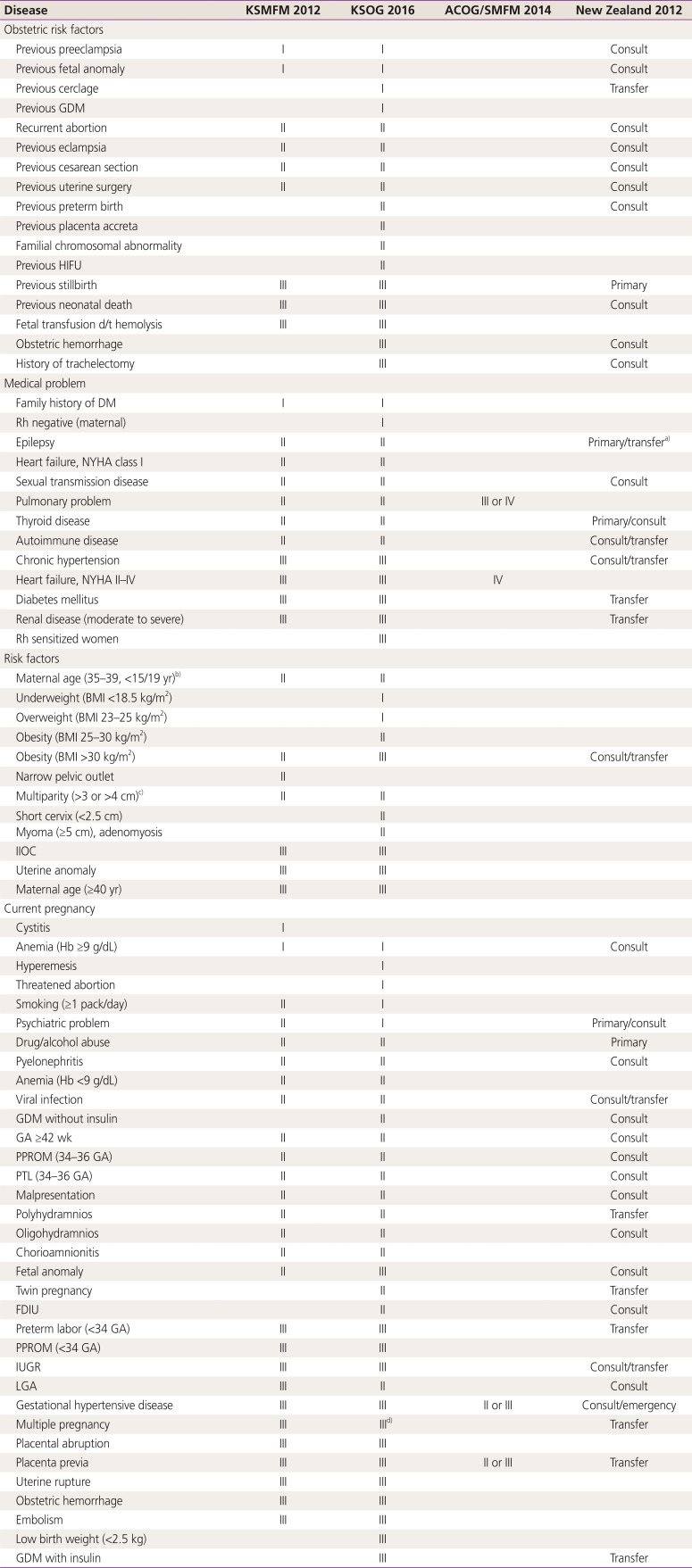
The definition of high-risk pregnancy has not been specified and may be variable according to the health care system of each country. In 2012, the Korean Society of Maternal Fetal Medicine suggested 3 grades of high-risk pregnancy for several obstetric conditions depending on several experts' opinions, and these criteria have been revised in 2016 by Korean Society of Obstetrics and Gynecology [1920]. The conditions considered as mild problems are classified into grade 1, whereas moderate states are regarded as grade 2, severe diseases are defined as grade 3. The primary physician in local clinics may decide to transfer the patient or not and choose the level of obstetric care facilities to transfer according to this grading system of high risk pregnancies (Table 5).
In 2015, ACOG showed the example of patients according to the level of obstetric care facilities. In this suggestion, birth center can take care of term, singleton, vertex presentation, whereas term twin gestation may be appropriate for level 1 (basic care) facilities. The examples of patients who should be managed in level IV (regional perinatal health care centers) facilities are severe maternal cardiac conditions, severe pulmonary hypertension or liver failure, pregnant women requiring neurosurgery or cardiac surgery, or patients in unstable condition and in need of an organ transplant [7].
In 2012, New Zealand Ministry of Health also proposed specific guidelines for consultation or transfer. There are 4 categories: primary, consult, transfer, and emergency condition. In this process maps, primary, consultation, transfer, emergent conditions are defined as follows. First, primary means the condition that the Lead Maternity Center (LMC) may consider as referral to another primary physician. Second, consult is the condition that requires consultation with another specialist. Third, transfer is a situation in which LMC should transfer to another specialist in order to allocate clinical responsibility to specialist. Fourth, emergency is criteria that needs prompt transfer of medical responsibilities to the most proper practitioners. In this system, medical or obstetric high risk conditions are classified as conditions that need referral to another primary physician, consultation with a specialist, transfer of responsibility to specialists, or emergent condition [21].
In Table 6, we compared these evaluation systems of pregnant women in outpatient services from Korea, USA, and New Zealand.
Conclusion
The evaluation of maternal condition and selection of the high-risk pregnancy that requires high level of cares are essential in order to reduce perinatal morbidity and mortality. Furthermore, unified classification of obstetric care depending on the capabilities of facilities is essential for the better outcomes in perinatal care. The guidelines and examples of the conditions that can be managed in each level can be helpful to make a proper decision in providing maternal health care. The goal of conceptualized framework for maternal care and effort to establish the high risk maternal conditions is for high risk pregnant women to receive appropriate care in institutions that are ready to provide specialized care, thereby improving perinatal mortality and morbidity.
In addition, many problems related to high-risk pregnancy are originated from not only transfer system but also low insurance and lack of manpower [222324]. Many obstetricians experience malpractice burden and decide to discontinue obstetric care due to financial problem. In USA, the government had assigned Critical Access Hospital (CAH) as a part of supporting obstetricians and hospitals in rural area through financial support and educational program. One of the policies converting rural hospital into CAH is Medicare Rural Hospital Flexibility Grant Program, which finally makes it possible to improve quality of medical service. There are several more projects such as National Rural Health Resource Center, Health Care Services Outreach Grant Program, Delta Rural Hospital Performance Improvement Project in order to support obstetricians to supplement manpower and resource in obstetric care in USA [25]. Therefore, we should focus on developing both transfer system and support program in obstetric care.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.