Supernumerary ovary on recto-sigmoid colon with associated endometriosis
Article information
Abstract
A supernumerary ovary is a rare gynecological anomaly, and is usually excised due to its malignant transformation potential. We report a case of a supernumerary ovary and endometriosis situated on the anterior rectosigmoid colon. When laparoscopy was conducted, a firm, 5-cm mass was discovered on the anterior rectosigmoid colon along with normal ovaries. In this case, the discovery of a supernumerary ovary implied the presence of endometriosis. It is unusual for endometriosis and a supernumerary ovary to exist simultaneously.
Introduction
A supernumerary ovary is found in 1/29,000 autopsy cases and is defined as a third ovary that develops in a location with no connection to the utero-ovarian ligament, broad ligament, or infundibulopelvic ligament [1].
This is an extremely rare gynecologic anomaly, while an accessory ovary, indicating the presence of more than 2 ovaries that are directly connected to these ligaments, is simply an uncommon congenital anomaly.
Winckel [2] first reported a case of supernumerary ovary in 1890. Wharton [1] stated that the exact incidence is unknown. One case of accessory ovary among 93,000 gynecological patients and one case of supernumerary ovary among 29,000 autopsies (occurrence 1/29,000 autopsies) have been reported.
A supernumerary ovary is usually found in the pelvis, consisting of the uterus, bladder, pelvic wall, retroperitoneum, omentum, mesentery, and inguinal region [3]. Accessory and supernumerary ovaries are mostly small and are usually not found before surgery for a specific reason.
In most cases, patients are asymptomatic, but may occasionally have chronic abdominal and pelvic pain, as in the present case report. Cystic or neoplastic transformation may cause the pain.
Case report
A 42-year-old woman, gravida 2 para 2, with a history of repeat cesarean section, had chronic abdominal and pelvic pain. She visited the hospital as an outpatient due to recent worsening. Physical examination was unrevealing. The abdomen was soft, with no palpable mass. Laboratory tests showed elevation of cancer antigen (CA) 125, but CA 19-9 was normal (CA 125: 85.4 U/mL, CA 19-9: <0.8 U/mL); other test results were within normal limits.
The sonogram showed multiple uterine myomas, and a homogeneous cystic mass on the left (Fig. 1A). Magnetic resonance imaging (MRI) showed normal ovaries, but a pelvic mass measuring 5.8×4.8 cm was discovered. This suggested ectopic ovarian endometriosis (Fig. 1B). Laparoscopic surgery under general anesthesia was planned for the diagnosis of endometriosis. At surgery, both ovaries were normal, but an ovarian cyst measuring approximately 6 cm was discovered on the anterior rectosigmoid colon (Fig. 1C). The ovarian cyst was not connected to the 2 normal ovaries. Chocolate-colored fluid was aspirated under laparoscopy, and the entire cystic mass was removed. In cross section, the external surface was grayish-white and smooth. The cut section surface was coated with dark brown hemorrhagic material. A pathologist at Eulji University Hospital described a unilocular cyst with wall thickness up to 0.2 cm (Fig. 1D). Microscopically, the cyst consisted of old hemorrhage. Focal spindle cells suggesting ovarian stroma were found (Fig. 1E). The cells exhibited cytoplasmic immunoreactivity to CD 10 (Fig. 1F). Thus, a supernumerary ovary with an endometrioma was diagnosed, based upon pathologic findings.
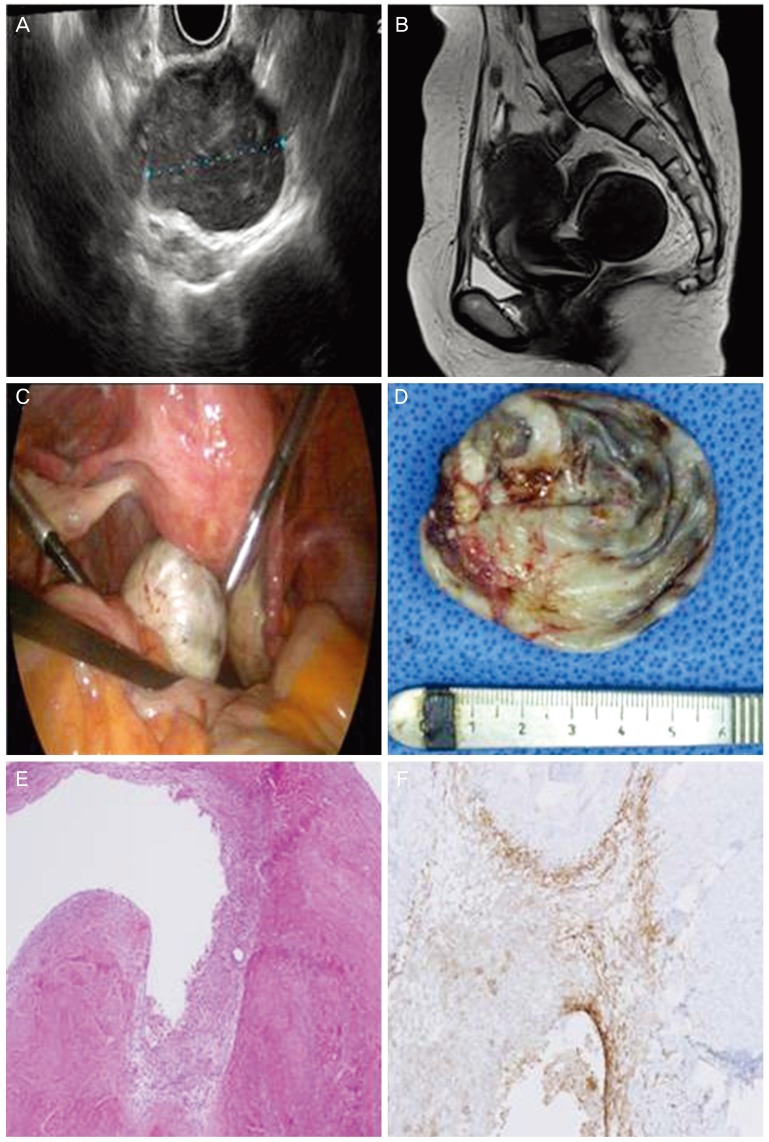
(A) Sonographic findings. (B) magnetic resonance imaging findings. Both ovaries were normal and a pelvic mass measuring 5.8×4.8 cm was discovered. (C) Laparoscopic findings. Both ovaries were visible, but a third ovarian cyst was discovered. (D) Gross findings. The ovarian cystic mass measured 5.0×4.0×1.5 cm and weighed 16.9 g. The external surface was grayish-white and smooth. On section, the cyst was unilocular and the inner surface was coated with dark brown hemorrhagic material. The wall thickness measured up to 0.2 cm. (E, F) Histopathologic findings. (E) Hematoxylin and eosin stain. Cystic wall of the supernumerary ovary showing spindle cell layer around endometrial tissue. The spindle cells suggested ovarian stroma (HE, ×100). (F) Benign cystic lesion lined by CD 10-positive cells in endometrial stroma, in association with endometrial glands. Aggregates of hemosiderin-laden macrophages were observed.
After surgery, the patient rapidly recovered, and was discharged on the third postoperative day. She has been followed at the outpatient clinic and did not receive hormonal medication to prevent recurrence. At 1 year, she is doing well without recurrence.
Discussion
Supernumerary and accessory ovaries are similarly used terms. Supernumerary ovaries have ovarian tissue. A supernumerary ovary has no direct connection with a normal ovary, whereas an accessory ovary is located near a eutopic ovary, and is directly connected to the normal ovary [1].
The term “ectopic ovary” was used by Lachman to replace the terms supernumerary and accessory ovary [4]. An ectopic ovary has an embryological or acquired origin. Embryonic origin refers to the case in which a cell is implanted at an abnormal location, with subsequent ovarian development. An acquired ectopic ovary can arise from implantation of ovarian tissue during surgery or as a result of postinflammatory implantation.
Normal ovarian development begins as gonadocytes migrate from the yolk sac endoderm to the germinal ridge via the dorsal mesentery. The development of supernumerary ovaries has been proposed to result from aberrant migration of part of the gonadal ridge following germ cell incorporation, or from migratory arrest of germ cells at an ectopic site, leading to induction of ovarian stroma during development [5].
In another hypothesis, ovarian tissue that is accidentally disrupted during surgery may be implanted in a location other than that of the original ovary to produce an ectopic ovary. When the ovary adheres to surrounding tissue as a result of chronic inflammation, an ectopic ovary may develop.
About 20% of supernumerary ovary cases also have endometriosis in the pelvic cavity [6].
It is known that spread of microscopic endometriosis can occur in the peritoneum, by invading the supernumerary ovary and inducing an endometrioma. The other possibility is lymphatic spread, which explains the occurrence of distant endometriosis [7].
However, there was no evidence for an association between a supernumerary ovary and endometriosis and/or endometrioma in our case.
The usual location of a supernumerary ovary is the pelvis, which consists of the uterus, bladder, pelvic wall, retroperitoneum, omentum, mesentery, and inguinal region [3].
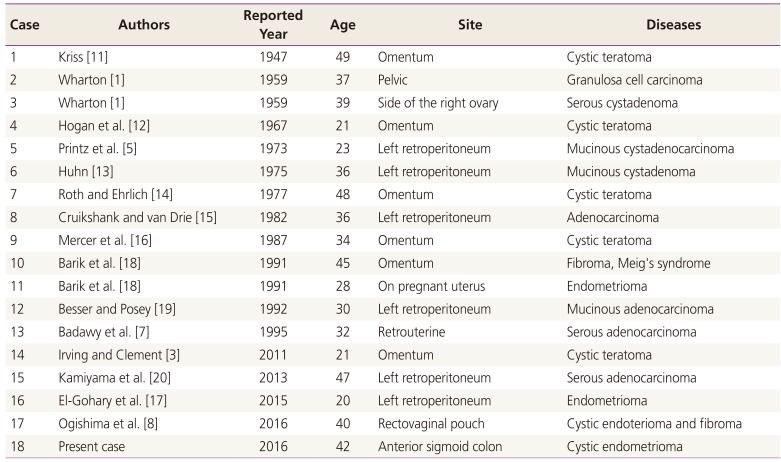
The site and disease in 18 cases (17 previously reported and the present case) with a tumor and/or endometriosis originating in a supernumerary ovary are presented in Table 1. Among the 17 previously reported cases, malignant tumor occurred in 6 cases, benign tumor in 8, and endometrioma in 3 [8].
Congenital anomalies are associated with accessory ovaries and supernumerary ovaries in up to 23% of cases. These anomalies include bicornuate and unicornuate uteri, bifid Fallopian tubes, accessory tubal ostia, agenesis of the kidney or ureter, duplicated ureter, bladder diverticulum, accessory adrenal glands, and a lobulated liver [9]. However, our patient did not have any congenital anomalies.
Most supernumerary ovaries are asymptomatic and considered nonfunctional. Supernumerary ovaries are seldom diagnosed before surgery for some unrelated reason or autopsy. Enlargement or torsion of a supernumerary ovary, however, can lead to symptoms such as abdominal pain.
A supernumerary ovary can be diagnosed using computed tomography (CT), MRI, ultrasonography, and color Doppler. If the margin is defined or a thick-walled cystic lesion can be seen on CT or MRI, a supernumerary can be suspected. Furthermore, if a vascular connection is not visible during color Doppler examination (as supernumerary ovaries do not have blood vessels connected to normal ovaries or pelvic muscles), a supernumerary ovary can be suspected [10]. However, there is a limit to the accuracy of diagnosing a supernumerary ovary with these imaging modalities.
Complete excision of the cyst is recommended for accurate pathologic diagnosis of this rare gynecological anomaly and to eliminate risk of malignant transformation.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.