Vaginal vault drainage as an effective and feasible alternative in laparoscopic hysterectomy
Article information
Abstract
Objective
Infected pelvic hematoma is a serious complication of hysterectomies. Pelvic drainage can help reduce complications. In this study, we evaluated the efficacy and safety of vaginal vault drainage in patients who underwent laparoscopic hysterectomy for benign gynecological diseases.
Methods
Patients who underwent laparoscopic hysterectomy and pelvic drain insertion for benign gynecological diseases between January 2008 and December 2015 were enrolled retrospectively in the study. They were grouped according to drain insertion sites, that is, through the abdomen (group 1) and vaginal vault (group 2). The postoperative outcomes were compared between the two groups.
Results
A total of 504 women were included. No significant differences were observed in the prevalence of postoperative fever, readmission, and reoperation between the two groups.
Conclusion
Given the discomfort associated with holding and removing the abdominal drain, inserting a closed pelvic gravity drain through the vaginal vault appears to be a feasible alternative to an abdominal drain.
Introduction
Hysterectomy is a common gynecological operation performed either through the vaginal, abdominal, or laparoscopic approach. Except for patients with pelvic organ prolapse, laparoscopic hysterectomy is the preferred procedure by both patients and surgeons because it offers several advantages, including a smaller wound, shorter operation time, fewer complications, faster recovery, and shorter hospital stay, compared to those of other procedures [1,2].
Pelvic hematoma is a common perioperative complication associated with hysterectomy, and its incidence has been reported to range from 25% to 98% [3,4]. Once it gets infected, it causes fever, abdominal pain and decreases serum hemoglobin (Hb) levels, leading to more blood transfusions, prolonged hospitalization, and an increased risk of readmission [5]. Previous studies have compared the postoperative outcomes of vaginal hysterectomy with those of abdominal or laparoscopic hysterectomy. Vaginal hysterectomy appears to be more significantly associated with the incidence of vault hematomas than that of abdominal hysterectomy [6–8].
Following hysterectomy, based on the surgeon’s decision and experience, pelvic drainage is usually performed to reduce the risk of pelvic hematoma formation, which is done by inserting a drain through the abdominal wall, laparoscopic trocar site, or vaginal vault. Regardless of the type of hysterectomy, the vaginal vault is incised during operation. Therefore, the insertion of drainage through the vaginal vault could be a feasible option. However, research surrounding the feasibility of vaginal vault drainage is limited, especially following laparoscopic hysterectomy.
In this study, we evaluated the feasibility and efficacy of closed gravity drainage through the vaginal vault in patients who underwent laparoscopic hysterectomy for benign gynecological diseases by comparing the postoperative outcomes of a vaginal vault drainage to those of a transabdominal drainage.
Materials and methods
1. Study population
This retrospective, comparative study was conducted at a single institution, Gachon University Gil Hospital. Female patients who underwent laparoscopic hysterectomy for benign gynecological diseases with a closed pelvic gravity drain insertion between January 2008 and December 2015 were included in this study. The patients were divided into the two following groups: patients with drains inserted through abdominal trocar sites (group 1) and the vault (group 2) (Figs. 1, 2). The study was conducted in accordance with the ethical standards of the Helsinki Declaration and was approved by the Institutional Review Board of Gachon Medical School, Gil Hospital (GBIRB 2015–49).
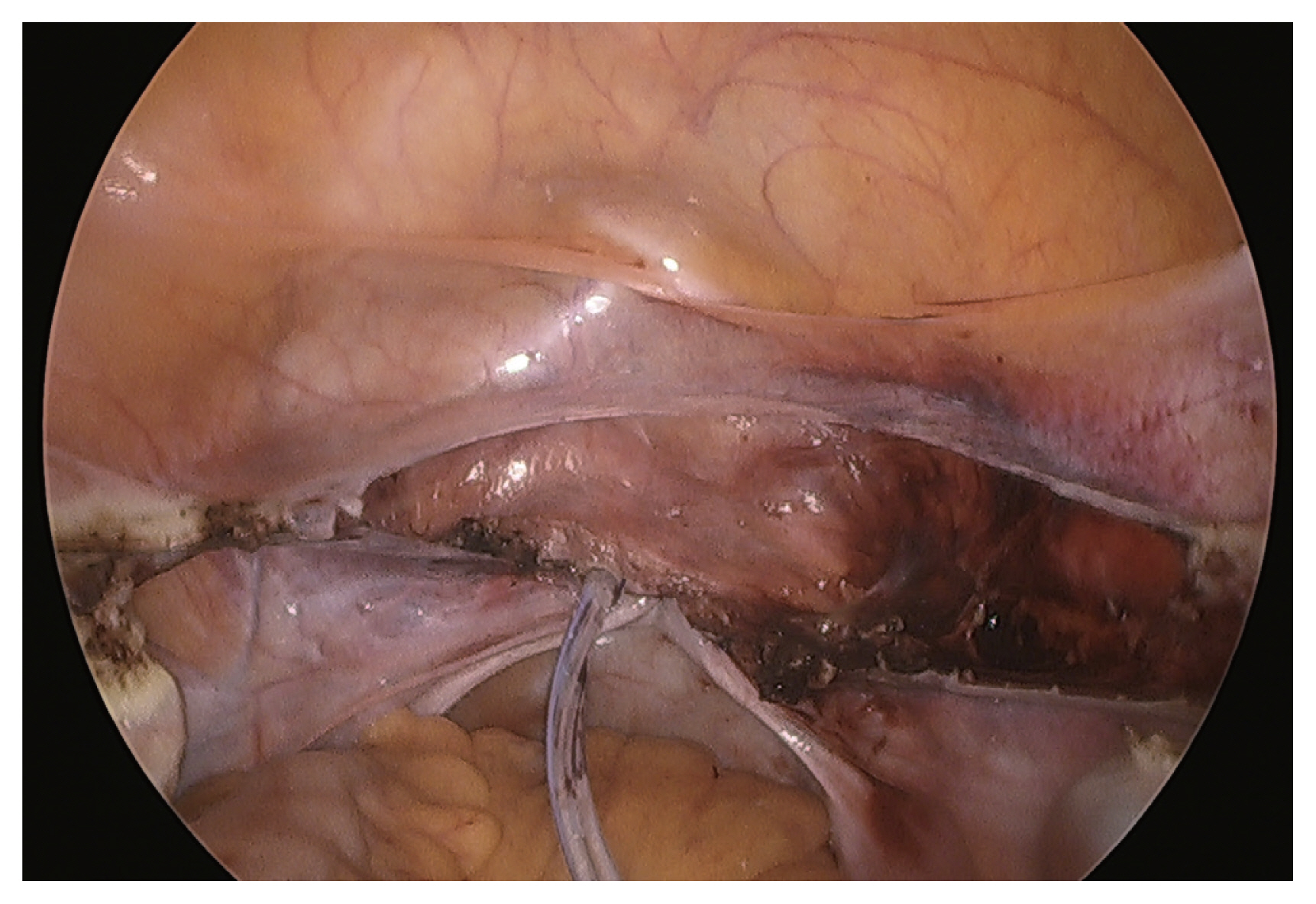
Insertion of a drain in the pelvic cavity through the vaginal vault. View from the abdominal cavity.
We retrieved patient’s demographic and clinical data, such as age, parity, height, weight, body mass index (BMI), surgical history, and pathological results, from their medical records.
2. Surgical procedures
Laparoscopic hysterectomy was performed by inserting a 12-mm trocar at the umbilicus and 5-mm trocars at both the paraumbilical and suprapubic areas. A single-port laparoscopic approach with a vertical 3-cm incision at the umbilicus was also performed in selective cases. The vaginal vault was sutured laparoscopically with absorbable materials in a continuous manner. If a pelvic drain (EZ-VAC® 200; GEMSKOREA, Seoul, Korea) was inserted before the closure of the vaginal vault, it was inserted either abdominally or vaginally. A silastic drain with a diameter of 5-mm was inserted through one of the 5-mm trocar sites or vaginal vault and connected to a bile bag. The abdominal drainage tube was anchored between the stitches using air knots. Therefore, before removing the abdominal drainage, we stiched off the anchored sutures. A vaginal vault drain was anchored between the stitches without air knots, and two pieces of gauze were inserted into the vagina to secure the drain. To remove it, we pulled the gauze and drain out with a small amount of force and did not suture or use any staples. The surgeon would decide to remove the pelvic drain on the first or second day after the operation based on the amount and nature of the drained fluids.
3. Surgical outcomes
Surgical outcomes were reviewed, including the operation time, estimated blood loss (EBL), perioperative Hb changes, and incidences of transfusion, readmission, and reoperation. Operation time was defined as the duration from the skin incision on the umbilicus to the closure of the abdominal incision. The preoperative Hb level was assessed within a month of the operation, and the postoperative level was estimated the morning after the operation. Transfusion rates were estimated during and after surgery. Postoperative fever was defined as a body temperature higher than 37.8°C, except for cases with atelectasis confirmed by chest radiography.
4. Statistical analysis
Continuous data was expressed as mean±standard deviation, and categorical data was expressed as number of cases (i.e., percentages). The mean values were compared using Student’s t-test, and the categorized values were compared using a chi-square test. Statistical analyses were performed using SPSS version 21 (IBM Corp., Armonk, NY, USA). If the P-value was less than 0.05, the null hypothesis that states that there is no difference between the means were rejected.
Results
A total of 504 patients were included in this study; 126 and 378 patients were assigned groups 1 and 2, respectively. Table 1 shows the baseline characteristics of the patients. There were no significant differences in age, parity, BMI, and surgical history between the two groups. The operation time and EBL were significantly lower in group 1 than those in group 2, leading to more blood transfusions in group 2 compared to that of group 1. However, no differences were found for the prevalence of postoperative fever, readmission, and reoperation between the two different drainage site (Table 2).
Four patients underwent reoperation, with two patients from each group. One of the patients in group 2 underwent reoperation because the vaginal drain got stuck between the vaginal vault sutures and had to be cut into two pieces during removal. The remnant drain in the pelvic cavity was located using abdominal radiography and removed using a long Kelly through the vaginal vault on the third postoperative day under general anesthesia. No additional sutures were performed, and the patient recovered without further complications. Of the remaining cases, one of the patients in group 1 experienced bleeding in the vaginal vault while two had vaginal vault dehiscence and underwent vaginal vault primary repair under general anesthesia and were discharged without complications.
Discussion
In this retrospective comparative study, we evaluated the feasibility of a closed vaginal vault gravity drain compared to an abdominal drain after laparoscopic hysterectomy for benign gynecological diseases. We inserted a vaginal drain without anchoring sutures; thus, the removal of the stitches at the drain insertion site was not required. In addition, it is more plausible to insert a vaginal drain because colpotomy is generally performed during surgery. Consequently, a vaginal drain is considered safer and more comfortable than an abdominal drain, with similar postoperative complication rates.
One observational study reported that vaginal or abdominal hysterectomy resulted in approximately 10–200 mL of postoperative pelvic fluid collections [5]. Even though pelvic hematoma is a common postoperative finding following hysterectomy, it can lead to higher morbidity rate when infected. Therefore, it is important to drain the pelvic fluid collection and avoid infection if there is a risk of pelvic hematoma formation. Previous studies on vaginal vault drainage have shown conflicting results regarding the incidence of complications. One randomized controlled trial found that, after vaginal hysterectomy, the incidence of postoperative complications was similar, irrespective of whether a vaginal vault drain was inserted. The risk of febrile morbidity, prolonged hospital stays, decreased in Hb level, and the need for blood transfusion were similar between the groups. Therefore, the routine insertion of a vaginal vault drain was not recommended [9]. Another retrospective study evaluated the efficacy and safety of vaginal vault drainage after a complicated single-port access laparoscopic-assisted vaginal hysterectomy. Although there was a tendency for patients with vaginal drainage to develop pelvic fluid collection and febrile morbidity occurred more frequently than that in patients without drainage, the differences were minimal regarding transfusion rates, intraoperative and perioperative complications, and febrile morbidity [10]. In contrast, a retrospective study found that leaving a patent tract in the vaginal vault instead of a complete closure significantly reduced the possibility of pelvic hematoma infection after a vaginal hysterectomy. They suggested that inserting a vault drain significantly reduced the incidence of infected pelvic hematomas compared to the complete closure of the vaginal vault [11].
The primary goal of our study was to determine whether the vaginal vault drain is as feasible and effective in reducing postoperative complications as the abdominal drain. To date, no study has compared the efficacy between vaginal vault and abdominal drains. Here, we estimated the incidences of postoperative fever, readmission, and reoperation as postoperative complications, and found that there were no significant differences between the two drain types. Notably, an increase in EBL correlated to an increase rate of postoperative complications in a retrospective cohort study including 18,003 hysterectomy cases [12]. Therefore, despite a greater amount of blood loss in patients with vaginal vault drains, one can assume that the risk of surgical morbidity was effectively decreased when vaginal vault drains were inserted.
When we reviewed the reoperation cases, we identified a case in which a vaginal drain was cut into two pieces because it got stuck between the sutures. The patient was reoperated under general anesthesia to locate the remnant tip of the drain. This was a single incident, but it is important to highlight that any forceful manipulation during drain removal through either the abdominal wall or vaginal vault should be avoided. A similar complication was a transabdominal drain slipping down into the pelvic cavity through the drainage tract [13]. This usually occurs when the drain is incompletely secured or a secured thread is loosened or cut accidently. Other reports have also described retrieving the abdominal drain and slipping it into the pelvic or abdominal cavity by relaparotomy or transvaginal endoscopic guidance [14–17].
This study had several limitations. As this was a single-center retrospective study, our results do not represent the general population. In addition, we did not analyze subjective factors, including pain or discomfort, as defined by a numeric rating scale (NRS). If the NRS in patients with vaginal drains was lower than that in patients with abdominal drains, our results would have been more promising. Randomized controlled trials evaluating subjective factors should be conducted to validate the feasibility and efficacy of closed vaginal vault gravity drains.
In conclusion, given the discomfort of carrying the drain and removing the anchoring suture from the drain insertion site via the abdomen, inserting a closed pelvic gravity drain through the vaginal vault appears to be a feasible and efficient method to reduce the risk of pelvic hematomas infection in patients who underwent laparoscopic hysterectomy.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Gachon Medical School, Gil Hospital (GBIRB 2015-49).
Patient consent
Informed consent was waived owing to the retrospective nature of the study.
Funding information
None.



