Sentinel lymph node biopsy in high-risk endometrial cancer: performance, outcomes, and future avenues
Article information
Abstract
Endometrial cancer is the second most common gynecological malignancy worldwide, with an overall favorable prognosis. However, a subgroup of patients has a high risk of recurrence and poor prognosis. This review summarizes recently published articles that examined sentinel lymph node (SLN) biopsy in patients with high-risk endometrial cancer. We focused on the performance and outcomes of SLN biopsy, and examined potential methods for improving the management of this high-risk subset. Few studies have examined the long-term outcomes of SLN in patients with high-risk endometrial cancer. Thus, we reviewed recently published retrospective studies that have adopted statistical techniques, such as inverse probability weighting or propensity score matching, to examine the outcome of SLN biopsy compared to conventional lymphadenectomy. Potential avenues for future research to fine-tune decision making for this patient subgroup were also discussed.
Introduction
The sentinel lymph node (SLN) mapping technique was developed based on the assumption that lymphatic drainage from the primary tumor spreads in a stepwise fashion from the proximal SLN to the distal lymph node [1]. It was first introduced in 1996 by Burke et al. [2] when examining endometrial cancer. Several large-scale prospective trials have supported the hypothesis that SLN mapping shows high detection accuracy compared to the conventional full lymphadenectomy (LND) [3,4], thereby offering adequate prognostic information, while preventing surgical morbidity, including the development of lymphocele and lymphedema [5,6]. International guidelines have changed accordingly, and according to the National Comprehensive Cancer Network (NCCN) guidelines published in 2014 [1], SLN mapping was assigned a category 2B recommendation only for institutions with expertise, and special caution was given to patients in the high-risk subgroup based on histology. The prevalence of endometrial cancer has steadily increased [7], and SLN mapping has started to garner interest worldwide, including in Korea, where it was first performed at the Yonsei University in 2014 [8]. Clinical evidence for SLN mapping continues to accumulate in patients with endometrial cancer with a wider risk spectrum, such as those with a high-risk histological subtype or poor prognostic uterine factors. In 2019, multiple international guidelines recommended that SLN mapping may be an acceptable alternative to systemic LND in intermediate-to high-risk endometrial cancer [9,10].
Despite recent updates in the guidelines, many clinicians still do not feel comfortable replacing conventional LND with SLN mapping in high-risk patients. Additionally, the risk of lymph node metastasis was much higher in this cohort, as high as 20–30%, compared to the 5% observed in patients with low-risk subtype [11–13]. Furthermore, alternative lymphatic drainage, resulting in isolated para-aortic lymph node involvement is concerning [14]. The reported incidence of para-aortic lymph node involvement ranges from approximately 10% in the general endometrial cancer population [15] to 17–20% in the cohort with high-risk subtypes [16–18]. Therefore, the limited accuracy of the cervical injection technique for para-aortic lymph node assessment may be a cause for concern, especially considering studies, such as the survival effect of para-aortic lymphadenectomy in endometrial cancer survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL) trial, which demonstrated that para-aortic LND is associated with a survival benefit in high-risk endometrial cancer [19]. To address this concern, various alternative SLN mapping techniques have been introduced, specifically for para-aortic SLN detection, such as peritumoral injection with a hysteroscope and fundal myometrial injection [8,20,21].
No consensus has been reached regarding the best management procedure for patients with high-risk endometrial cancer, and there is a paucity of prospective data on the long-term prognostic outcomes of high-risk patients subjected to SLN mapping. When interpreting the outcome of SLN mapping in high-risk endometrial cancer, the aforementioned factors, such as cohort demographics and details of the SLN techniques are important considerations. Moreover, other factors may affect survival outcomes, such as surveillance method and periodicity, which may vary with adjuvant strategies and between institutions for patients with node-negative tumors with high-risk features that have evolved over time. Interpretation of the outcome data necessitates caution in the absence of large prospective randomized trials.
Hence, the objective of this review article was to summarize recently published data on the performance and outcomes of SLN mapping in patients with endometrial cancer, with a focus on high-risk histological subtypes or deep myometrial invasion. With respect to the outcomes, we discussed studies that utilize different statistical methods to overcome selection bias as an inherent limitation of a retrospective study design. Lastly, potential avenues for future research to fine-tune decision making for this patient subgroup are also discussed.
Methods
PubMed, Cochrane Library, and the NCCN guidelines were used for different combinations of the following key terms: “endometrial cancer,” “sentinel lymph node,” “survival outcome,” and “high-grade.” Adjunctive terms for SLN, including “SLN biopsy” and “SLN mapping” were also included.
Studies were selected for review if they were published in a journal that included articles in English, were available for a complete review, and comprised a significant number of patients (≥30 patients). References were searched for relevant studies that could have been missed in the original systematic search. Seminal observational studies published in high-quality journals were also included in the meta-analysis. Similar studies were cross-compared to exclude repeated analyses of similar patient populations. With respect to the data, selected journals were reviewed for the inclusion of endometrial cancer patients with endometrial cancer with high-risk features. Many different risk stratification methods have been introduced for endometrial cancer [22], including findings based on post-surgical specimens, such as lymphovascular space invasion (LVSI). Based on the Mayo and ESMO criteria [23,24], the two factors that were preoperatively identifiable based on biopsy or imaging, namely histological subtype and presence of deep myometrial invasion were used to define high-risk endometrial cancer in this review. Studies involving patients with endometrial cancer with either (i) grade 1 (G1) or grade 2 (G2) histology with deep myometrial invasion or (ii) grade 3 (G3) or non-endometrioid histology, regardless of deep myometrial invasion were analyzed. Most studies were in line with this definition unless otherwise specified. Recent updates on the molecular risk-stratification method and Proactive Molecular Risk Classifiers for Endometrial Cancer (ProMisE) classification are only mentioned in the future direction section.
For specific SLN mapping techniques, cervical injection of indocyanine green (ICG) following the NCCN guidelines was considered the standard [10]. Studies utilizing other types of dyes, in addition to ICG, have been specified. Alternative SLN mapping techniques that utilize injection sites other than the cervix have also been specified. For publications on the detection accuracy of SLN mapping, the performance of SLN mapping was assessed in the setting of SLN mapping followed by LND, where LND was considered the standard. Failed SLN mapping refers to unilateral detection failure. Studies that focused on survival outcomes were assessed on the outcomes of SLN mapping. Overall, studies that exclusively examined patients with high-risk endometrial cancer or those with a majority of the patient population, consisting of those with high-risk characteristics were prioritized.
Results
1. Detection accuracy of SLN in high-risk patients
Several concerns are associated with the SLN detection rate in high-risk subpopulations. First, the overall risk of lymph node metastasis is high in this patient subset; thus, the cost of missed lymph node metastasis due to either technical failure or lack of surgeon proficiency will also be significant. Therefore, previous studies have emphasized that side-specific LND should be performed in cases of failed SLN mapping [25]. SLN mapping failure may be more common in high-risk patients with positive lymph node metastasis, owing to altered lymphatic drainage or tumor infiltration. Moreover, the SLN mapping rate differs, depending on the surgical proficiency. A previous study that assessed various factors associated with SLN mapping failure (age, body mass index, menopausal status, previous surgery history, and pathological factors) found that surgical proficiency was the most important factor [26]. Another study on the learning curve for SLN mapping showed that approximately 40 cases were required for plateauing of the learning curve for successful bilateral mapping [27]. Surgical competency assessment tools have also been developed for this purpose [28]. Thus, for SLN mapping in high-risk patients with endometrial cancer, adherence to the prespecified protocol in the context of high surgical proficiency is of paramount importance.
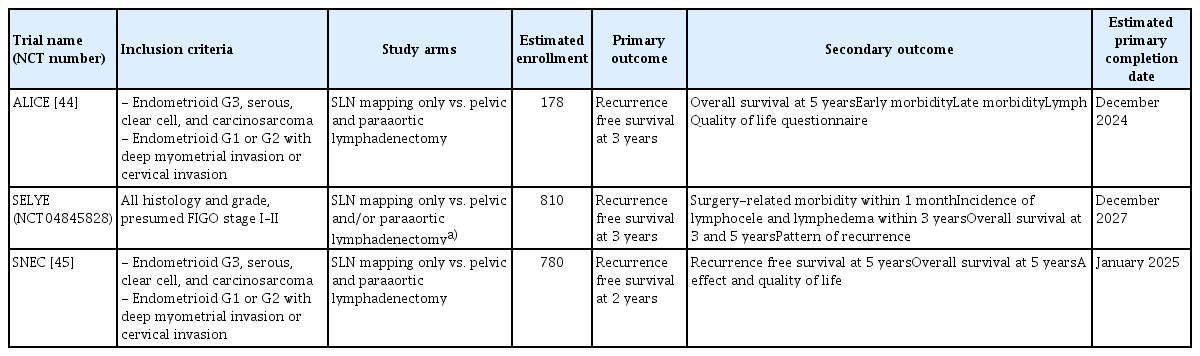
Several prospective studies have highlighted the role of SLN mapping in patients with high-risk endometrial cancer, and the specific details of these studies are summarized in Table 1 [18,29–31]. Studies examining the performance of SNL mapping in conjunction with cervical injection of ICG in patients with high-risk endometrial cancer showed an overall high performance of SLN mapping in such patients, with a sensitivity of 95–98% and a negative predictive value of 97–98%. Bilateral detection rates varied, ranging between 58–95%. Moreover, protocols that specified reinjection in cases of failed mapping showed a high bilateral detection rate, resulting in a low false-negative rate. Based on a recent meta-analysis of nine studies examining 429 patients with stage I endometrial cancer showing G3 endometrioid and non-endometrioid histology subtypes, the pooled sensitivity, negative predictive value, and false-negative rate were 92%, 97%, and 8%, respectively [32].
Summary of studies on the detection accuracy of SLN mapping in high-risk endometrial cancer patients
Among the studies examining the performance of SLN mapping in high-risk patients, the SENTOR study conducted by Cusimano et al. [31] is one of the largest prospective studies that excluded patients with the G1 histological subtype. In this study setting, where SLN was followed by pelvic and para-aortic LND, lymph node metastasis was found in 27 of 156 patients. Among the node-positive patients, 52% showed metastasis, which was identified in the SLN-only cohort, and 26% were outside the traditional LND boundaries or required immunohistochemistry for diagnosis, emphasizing the added value of SLN mapping over conventional LND.
Moreover, real-world incorporation of SLN biopsy appears to cover a wider population than expected. A population-based retrospective study by Matsuo et al. [33,34] showed that clinicians have begun to perform SLN biopsy in stage II and T3 diseases, which is beyond the current guideline recommendations. We speculated that clinicians have begun to universally adopt SLN biopsy in the absence of distant metastases. Another possibility is that patients believed to exhibit T1 stage disease preoperatively could demonstrate occult T3 disease, postoperatively. Prospective studies should evaluate the validity of SLN mapping in a wider population of high-risk stage I disease patients.
2. Survival outcomes associated with SLN in high-risk patients
Few studies have examined the long-term outcomes of SLN in patients with high-risk endometrial cancer. Despite the recent revision of international guidelines, certain clinicians still feel uncomfortable performing SLN mapping only in this patient population because previous studies have stated that LND may improve survival outcomes in such patients [19,35,36]. The SEPAL study, which retrospectively assessed 671 patients who underwent pelvic and para-aortic LND versus pelvic LND alone, revealed that the addition of paraaortic LND was associated with better survival outcomes in patients who were characterized as intermediate-to-high-risk cohorts [18]. Similarly, a meta-analysis showed that systematic para-aortic LND was associated with favorable overall survival (OS) outcomes in endometrial cancer patients with intermediate-or high-risk recurrence [37]. With respect to non-endometrioid histology, a national database study of 7,250 patients with non-endometrioid histology showed that pelvic LND, specifically the procedure involving the removal of >15 nodes, was associated with a reduction in mortality rate [35].
More recent studies comparing the survival outcomes associated with SLN alone compared to those of LND are small retrospective or prospective studies, examining the short-term outcomes of patients with specific histological subtypes. A recent retrospective study by Basaran et al. [38] compared a 2-year progression-free survival (PFS) and OS of 245 patients with serous histology who underwent either SLN alone or LND without SLN. In this study, the 2-year PFS rates were 58.8% and 64.9% (P=0.478), and 2-year OS rates were 89.1% and 83.9% (P=0.9) in the SLN and LND groups, respectively. Another retrospective study by Schiavone et al. [39] compared the 2-year PFS in 136 patients with carcinosarcoma and revealed that the median PFS was comparable between the SLN and LND groups (23 vs. 23.2 months, P=0.7). The adjuvant patterns were comparable in both groups in both studies.
An important caveat of these retrospective studies is that the SLN group invariably represented a temporary cohort. During the initial adoption phase of SLN mapping, clinicians in many institutions opted for safety by performing a validation LND in addition to the SLN mapping. Therefore, if patients who were subjected to SLN only were to be compared to those who were subjected to LND only, a significant time gap would likely exist between the two cohorts. One solution is to examine recurrence or mortality within a specific timeframe with either a 2-year or 3-year limit [38,39]. However, this approach does not solve the problem entirely. It is possible that, during this transition period, patients with favorable clinical characteristics were disproportionately selected for SLN mapping. Adjuvant therapy has evolved over time. Thus, to mitigate such bias, several recently published retrospective studies have adopted statistical techniques, such as inverse probability weighting (IPTW) or propensity score matching (PSM), to adjust for the differences in baseline characteristics of the patients.
In theory, IPTW utilizes a logistical regression model to create a pseudo-population in which patients with a high probability of receiving treatment are assigned smaller weights, and those with a low probability are assigned larger weights [40]. Compared with PSM, IPTW is advantageous because it utilizes all observation points and allows comparison of outcomes in multiple groups. In the context of SLN mapping, Schlappe et al. [41] used the IPTW method to compare a 3-year PFS and OS rates in 214 patients with serous or clear cell subtypes. IPTW-adjusted 3-year PFS and OS were not compromised by the SLN algorithm. However, an important disadvantage was that patients at one institution were subjected to SLN, those at a different institution were subjected to LND, and the surveillance methodology and adjuvant pattern were significantly different between the two institutions. Even after statistical adjustment using the IPTW method, the trends associated with PFS and OS were reversed despite the lack of statistical significance.
The PSM method is another frequently used statistical method, especially when the two groups have different sample sizes [40]. Based on logistic regression, the PSM selects a subset of patients from the larger group who are similar in terms of covariates to those from the smaller group. Although the overall sample size is usually small, the baseline characteristics are comparable after matching. In the context of SLN mapping, Bogani et al. [42] conducted a multi-institutional retrospective study, comparing SLN mapping and SLN with LND performed as a backup in high-risk patients. Using PSM with a 1:1 ratio, 50 patients were selected from 146 patients in the LND group for further comparison with 50 patients subjected to SLN alone, resulting in a reduced effective sample size between 192 to 100 patients. In this study, multivariable analysis showed that LVSI was the most important prognostic factor for predicting recurrence, but not survival. The outcomes between the two groups did not differ; however, the median follow-up period was only 17 months, and maturation of the outcome data appeared to be necessary. Another study conducted by Nasioudis et al. [43] utilized PSM matching for patients with high-risk endometrial cancer included in the National Cancer Database. As the SLN group included 70% of the patients undergoing validation LND in addition to SLN (i.e., patients during the transition phase), the authors performed an additional sensitivity analysis with the group of patients subjected to SLN alone. In this study, after controlling for lymph node status, depth of myometrial invasion, and administration of adjuvant therapy, no differences were observed in the 3-year OS between the two groups (hazard ratio, 1.39; 95% confidence interval, 0.77–2.52).
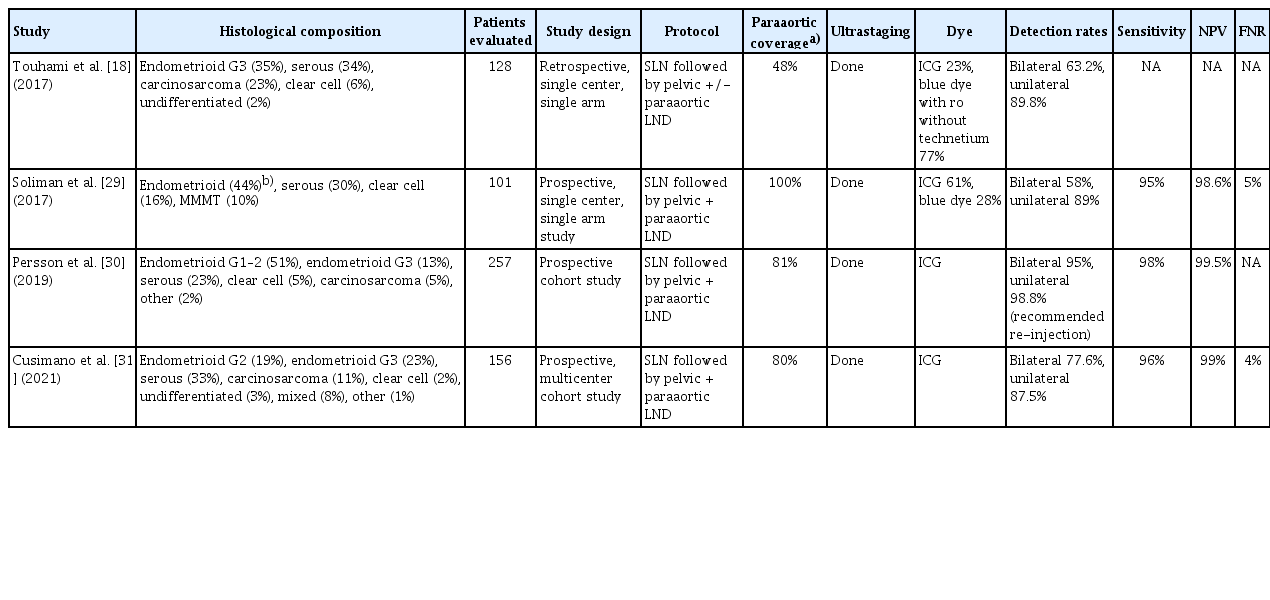
During the interpretation of studies on the survival outcomes of SLN mapping in high-risk patients, surgical and adjuvant factors should be carefully considered. If the SLN mapping was to be compared with full LND, not only was the proportion of patients undergoing full LND up to the para-aortic region, but also whether the anatomic location up to the renal vein level was covered and the number of para-aortic lymph nodes removed should be noted. If the survival outcome of SLN mapping is superior to that of complete LND, this may underscore the survival benefit of detection alone rather than resection. The recent shift in the focus on adjuvant therapy from radiotherapy to chemotherapy based on adjuvant chemotherapy versus radiotherapy alone in women with high-risk endometrial cancer (PORTEC-3) will likely bias support the survival advantage of detection, more so than resection [44]. Considering these complex factors, the best setting to study the survival outcome of SLN mapping in high-risk patients would be a randomized controlled study design. Notable ongoing randomized controlled trials, including ALICE [45], SELYE (clinical trial: NCT04845828), and SNEC trial [46], and the details including the inclusion criteria, primary outcome, and estimated completion date are shown in Table 2.
3. Methods of fine-tuning SLN mapping with respect to paraaortic assessment
Although the prevalence of isolated para-aortic lymph node metastasis in the general endometrial cancer cohort is 1–3%, assessment of the true rate is difficult because it can only be determined through studies performed with patients subjected to systematic LND, in which a large number of pelvic and para-aortic nodes are removed in the upper para-aortic region. Furthermore, with lymphatic dissemination as the denominator, the rate of isolated lymph node metastasis, ranging between 16–25% is not low [8,47,48]. Thus, adequate assessment of para-aortic SLN may be of remarkable value in patients with high-risk endometrial cancer because such patients demonstrate a higher rate of nodal and para-aortic lymph node metastases compared to the general endometrial cancer cohort.
With adequate development of the SLN technique for para-aortic lymph node detection, the detection rate may be improved from approximately 20% [3] to 50–80% [8,19,48] using alternative injection techniques. Previously, hysteroscope-guided peritumoral injection of ICG administered to >200 patients from a single center showed a para-aortic SLN detection rate of >50% [49]. However, a multicenter prospective randomized study of 165 patients who were administered hysteroscope-guided injection alone versus those administered cervical injection reported better pelvic SLN identification and a higher bilateral detection rate with the cervical injection method [50]. Another alternative is the fundal injection of ICG using a laparoscopic approach, which is usually performed sequentially with cervical ICG injection and pelvic SLN sampling. Previous studies from Korea utilized a two-step SLN mapping, which showed a high detection rate of para-aortic SLN and was 67% in the lower para-aortic region and 38% in the upper para-aortic region [8]. A more recent study by Ruiz et al. [48] that examined 278 patients who were administered dual injection for 5 years, reported a similar para-aortic SLN detection rate of 65%. Some authors have stated that isolated para-aortic metastasis is frequently accompanied by overlooked metastasis or micrometastasis in the pelvic lymph nodes. The assessment of para-aortic SLN is by-passed, especially with the frequent implementation of adjuvant chemotherapy in patients with high-risk endometrial cancer. Nevertheless, the decisions regarding the SLN technique of choice in this patient subgroup should be made by individual clinicians.
4. Weaving through the heterogeneity within the high-risk subgroup
The term high-risk comprises a heterogeneous subset. Therefore, patients with non-endometrioid histological subtypes (i.e., serous, clear cell, carcinosarcoma, or mixed) may present with different clinical phenotypes, genomic backgrounds, and varied prognostic and therapeutic implications. Hence, certain studies examining the outcome of SLN mapping in high-risk endometrial cancers have focused on one specific histological subtype [38,39]. For instance, targeted therapies based on HER2 expression, homologous recombination deficiency, and mismatch repair (MMR) status have been explored for serous carcinomas [51]. These therapeutic advances do not preclude continued research on SLN mapping in patients with serous carcinoma. However, some patients may benefit from SLN mapping for effective diagnosis of low-volume disease followed by personalized adjuvant therapy instead of extensive LND.
Similarly, in patients with low-risk endometrioid histology, those with deep myometrial invasion may be considered to be different from those with LVSI. For instance, patients with deep myometrial invasion, especially in the uterine fundus, may show an increased risk of lymphatic dissemination through the upper para-aortic pathway by-passing the pelvic route [14,52]. Patients with LVSI showing tumors in the lower cervical region may demonstrate an overall increased risk of pelvic lymph node involvement but not necessarily a disproportionate increase in para-aortic lymph node involvement. Likewise, to interpret the data of any studies on SLN mapping in high-risk endometrial cancer, attention should be paid to the definition of “high-risk” and details of patients.
5. Avenues for future research
One important research area is the best utilization of SLN mapping in the era of ProMisE classification [53]. The ProM-isE classification is currently validated in many clinical settings and has the potential to be used as a prognostic stratification modality, either alone or in combination with other clinical risk factors [54]. Assuming that the classification according to the ProMisE criteria is possible and based on pre-hysterectomy specimens, such as tissues derived from diagnostic curettage, it is likely that research on SLN mapping in patients with high-risk endometrial cancer will change significantly [9]. The ProMisE-based molecular classification has already been incorporated into the updated ESMO guidelines [55], and the current definition of “high-risk” features associated with stage I endometrial cancers with respect to SLN mapping may change in the future.
An important research question involves finding a subset of high-risk patients with favorable prognoses, as currently defined. Although studies, such as the PORTEC-3 stated that patients with stage III disease are most likely to benefit from adjuvant chemotherapy compared to radiotherapy [44], no consensus has been reached regarding the best adjuvant therapy of choice for stage III patients [56]. Longitudinal studies on patient-reported outcomes of adjuvant chemotherapy revealed that in patients with endometrial cancer, adjuvant chemotherapy is independently associated with increased fatigue, lymphedema, and neuropathy even after 2 years of treatment [57]. Therefore, efforts are required to minimize unnecessary adjuvant chemotherapy. The presence of POLE mutations in high-risk patients is an excellent example of this [58]. These patients may not need adjuvant chemotherapy even if SLN mapping identifies macroscopic lymph node metastasis; they may not require SLN mapping at all. Another interesting patient subgroup included patients with MMR deficiencies. Previous studies have suggested that patients with endometrial cancer accompanied by MMR deficiency frequently have tumors in the lower uterine segment [59]. If dissemination through the para-aortic lymphatic channel is less common with this tumor localization [14,52], pelvic lymph node mapping with cervical injection of ICG may be sufficient for this patient subgroup, especially considering that patients with MMR deficiency respond exceptionally well to immunotherapy [60].
Conclusion
In recent decades, extensive research on SLN biopsy has led to changes in the international guidelines for the management of high-risk endometrial cancer. The simplicity of cervical ICG injection and its high detection accuracy have led to studies examining the long-term outcomes of SLN mapping in patients with non-endometrioid histology and those showing endometrioid histology with high-risk uterine features. Many studies have incorporated various statistical analyses to allow for group-wise comparisons; however, these methods have limitations. The results of prospective randomized studies have demonstrated an appropriate approach. As more research is being conducted on endometrial cancer based on molecular classifications, further research on SLN mapping and biopsy is required to examine the clinical relevance of SLN biopsy.
Notes
Conflict of interest
There is no conflict of interest in this research. Young Tae Kim has been an Editorial Board of Obstetrics & Gynecology Science; however, he was not involved in the peer reviewer selection, evaluation, or decision process of this article. Otherwise, no other potential conflicts of interest relevant to this article were reported.
Ethical approval
The study is not applicable to Institutional Review Board.
Patient consent
Patient consent was not necessary for this research.
Funding information
None.