Does transcutaneous electrical nerve stimulation reduce the laparoscopic related shoulder pain?
Article information
Abstract
Objective
Although laparoscopic surgery is a good substitute for laparotomy in reducing postsurgical pain, many patients complain of shoulder pain after laparoscopic surgery and require pain-relief. Post-operative pain management leads to increased patient satisfaction. Transcutaneous Electrical Nerve Stimulation (TENS) is a non-pharmacological, non-invasive modality that reduces pain by activating the descending inhibitory systems in the central nervous system. Given the importance of decreasing shoulder pain after gynecological laparoscopy, the current study aimed to investigate the management of shoulder pain in these patients using TENS.
Methods
This was a retrospective case-control study. A total of 112 women aged 18–45 years who experienced shoulder pain due to gynecologic laparoscopic surgery were included in the study. Patients were divided into TENS and control groups. In the TENS group, TENS was used twice for 20 minutes each, but in the control group, the patients received regular treatment. Patients were evaluated at intervals of 2, 4, 8, 24, 48, and 72 hours after laparoscopy for shoulder pain score.
Results
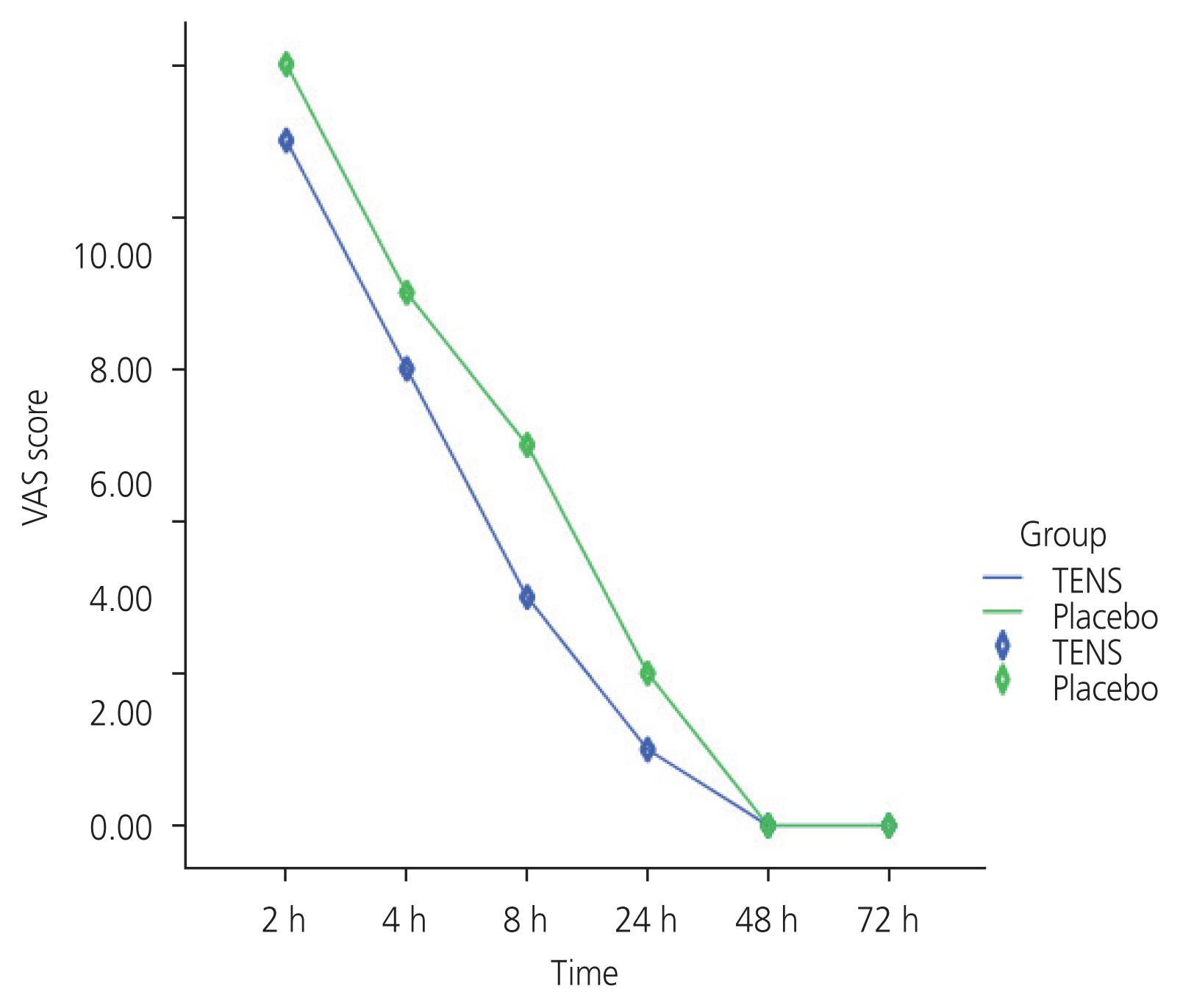
The results showed a significant decrease in visual analog scale scores at 2, 4, and 8-hour in the TENS group compared with the control group. At 24 hours evaluation, although the pain was reduced, the difference was not significant. At 48- and 72-hour assessment, all patients in each group reported zero score for severity of pain.
Conclusion
The findings suggest that TENS significantly reduces postoperative shoulder pain.
Introduction
Reducing human suffering related to untreated or poorly managed pain is a medical challenge and a moralist imperative [1]. Regardless of the type or method of surgery, pain management is crucial because it reduces the costs and length of hospital stay and increases patient convenience. Pain can be managed through multiple approaches [2,3], including a better conception of pain mechanisms, issuance of guidelines, establishment of acute pain services, and the availability of new medications and devices. Postoperative pain relief is a major problem worldwide [2].
Although minimally invasive, laparoscopy is a surgical technique used for the diagnosis and treatment of gynecological diseases. The advantages of laparoscopic surgery over laparotomy include smaller incision, less tissue disruption, milder and shorter duration of postsurgical pain, and a rapid healing course. Unfortunately, a high percentage of patients experience severe pain after laparoscopy and require pain relief [1]. Pain can be divided into shoulder pain (STP), incisional, and upper abdominal pain. Shoulder tip pain is specific to laparoscopic surgery, and induces pain around the shoulders. It has been emphasized that the most probable cause of this pain is carbon dioxide pooling in the abdominal cavity, toward the diaphragmatic region.
The cause of shoulder pain syndrome after laparoscopic surgery in women has not been fully determined, and is probably multifactorial and referred pain [4]. Three theories explain the cause of shoulder pain. The first theory is the conversion of carbon dioxide gas into carbonic acid, which reduces the peritoneal pH and stimulates the peritoneal and diaphragm nerves and causes shoulder pain [5,6]. The second theory states that residual gas cavities in the abdominal cavity cause shoulder pain in various ways [7]. The third theory of shoulder pain syndrome after laparoscopic surgery is tissue trauma, which is also called the neuropraxia theory. According to this theory, stretching and/or damage to the peritoneum and diaphragm by pneumoperitoneum leads to the rupture of blood vessels, stretching of nerves, and release of inflammatory mediators, which causes pain in the shoulder [6].
To date, many efforts have been made to decrease postlaparoscopic pain because people view laparoscopic surgery as a small-incision substitute for laparotomy; however, this pain seems less acceptable. The literature is contains a lot of modalities and medications to prevent or reduce STP, including all kinds of analgesics, sedatives [8,9], nerve blocking policies [10], trying to empty more air by different tips and tricks [11], and bioelectric therapy (transcutaneous electrical nerve stimulation [TENS]) [1].
TENS is a non-pharmacological intermediary that reduces pain by activating the descending inhibitory systems in the central nervous system. In this procedure, electrodes are placed on the skin near the painful area to decrease pain by stimulating peripheral sensory nerves. This device consists of three parts: a TENS unit, an interface wire, and an electrode. The TENS unit is an electric pulse generator that transmits these waves to the electrodes via an interface wire [12,13]. Electrodes are placed on the skin near the painful area to transmit electrical pulses and reduce pain by stimulating the peripheral sensory nerves [12,14]. TENS is clinically used at different frequencies, intensities, and durations. Depending on the excitation frequency, TENS is generally divided into two categories: high frequency TENS and low-frequency TENS. High-frequency TENS works through the gate theory and produces only short-term analgesia, whereas low-frequency TENS works through the release of endogenous opioids, which trigger a more systematic and long-term response. TENS is inexpensive and can be performed independently. Contraindications to the use of TENS include electronic implants such as cardiac pacemakers [13]. Systematic studies have shown that TENS, when used at sufficient severity, is effective for osteoarthritis, painful diabetic neuropathy, postoperative pain, and some acute pain; nevertheless, the evidence for the effectiveness of TENS is contradictory and requires further investigation [1]. As a few reviews have been published on the application of TENS to relieve shoulder pain after laparoscopic surgery, this study aimed to investigate the efficacy of TENS in reducing shoulder pain after gynecological laparoscopy.
Materials and methods
1. Study population
The present study retrospectively compared the TENS and non-TENS groups. It included 112 women aged 18–45 who underwent gynecological laparoscopic surgery and reported shoulder pain. The duration of surgery was less than 3 hours and the intra-abdominal pressure of the study patients during laparoscopy was less than 14. Patients with the following conditions were excluded from the study: epilepsy, malignancy, deep vein thrombosis, cardiac pacemaker, lung problems, addiction and depression, diaphragm lesions and electronic implant diseases, and fragile and damaged the skin in the areas of TENS use. The patients were divided into case (TENS) and control (regular treatment) groups.
2. Procedure
All patients were administered general anesthesia using the same protocol. After entering the operating room, a suitable venous route was taken for all patients, and standard monitoring was established (end-tidal carbon dioxide, oxygen saturation percentage, heart rate, and non-invasive blood pressure). As a prodrug, all patients were given 0.02 mg/ kg Midazolam and 2 mg/kg Fentanyl. Induction was started slowly with intravenous propofol (2 mg/kg) and completed with 0.5 mg/kg atracurium. To maintain anesthesia, Propofol 100 μg/kg/min and atracurium 0.15 μg/kg were administered after every 15 minutes. Laparoscopy was performed by entering a 10 mm umbilical trocar, creating a pneumoperitoneum and placing two 5 mm lateral trocar and one 10 mm supra-pubic trocar. We performed ovarian endometriosis cyst in our patients using ovarian cystectomy as the method of choice based on the 2018 ESHRE guidelines [15]. We performed either cautery or cutting according to the lesion size for other endometriotic lesions, such as peritoneal nodules. None of the patients experienced complications during cystectomy or hysterectomy. At the end of surgery, the patient’s abdomen was pressed to release CO2 gas. No analgesics were administered during recovery. After laparoscopy in the TENS group, two electrodes were placed vertically on the sides behind the shoulder, below the neck, and on the right and left sides at a downward angle. The distance between the pads should be at least one inch and increasing the distance between the pads reduces the success rate. In the TENS group, the conventional TENS method (high frequency: 100 HZ, low intensity, duration 120 μs) was used twice, each time for 20 minutes. The first time was used in the first hour of entering the ward and the second time after 6 hours. In both groups, non-steroidal anti-inflammatory drugs (NSAIDs) (indomethacin 50 mg with a maximum dose of 150 mg or apotel every 4 hours) were used to control pain, if necessary. In the ward, all patients underwent regular postoperative follow-ups, as previously reported. Accordingly, at intervals of 2, 4, 8, 24, 48, and 72 hours after laparoscopy in terms of shoulder pain score, and need for pain analgesics were evaluated by visual analogue scale (VAS).
3. Sample size
Each intervention group included 56 patients in a repeated-measures design with one between-subjects factor (treatment groups) and one within-subjects factor (assessment time). The sample size was calculated using VAS score as the primary outcome. The 56 participants per group were evaluated using a significance level of 0.05 and a power of 80.0%, according to difference of 0.1 in the VAS score between groups and a standard deviation of this outcome 1.9, which in equal in both groups.
4. Statistical analysis
Pain intensity was measured using the VAS. The primary outcome of this study was the VAS score measured at 2, 4, 8, 24, 48, and 72 hours. The score was calculated by measuring the distance (mm) between the “no pain” anchor and the patient’s mark on a 10-cm line, resulting in scores ranging from 0 to 100. Continuous variables, including age, body mass index (BMI) (kg/m2), and VAS scores, were summarized as mean±standard deviation. Categorical variables, such as the type of operation, were presented as proportions. The chi-square test and student’s t-test were used to compare the basic characteristics of patients among the groups. We analyzed changes in VAS scores over six assessments points using repeated-measures analysis. Statistical significance was set at P-value <0.05.
Results
A total of 112 patients were evaluated for eligibility, and two of them were excluded due to a shift from laparoscopic surgery to laparotomy. Among these patients, 57 were placed in the TENS group, while 53 were assigned to the control group. Demographic characteristics, terms, and surgical types were comparable between the two groups. No significant differences were observed between the two groups in terms of age, BMI, and length of surgery (P>0.05). However, the NSAIDs used in the TENS group differed significantly from those in the control group (P>0.05) (Table 1).
During the postoperative period, VAS scores were documented. The results showed that in the first assessment conducted 2 hours after surgery, the mean VAS score was significantly lower in the TENS group than in the control group (P=0.04). Additionally, at 4 and 8 hours, a significant decrease was found in the VAS score in all three TENS groups compared to the control group (P<0.001). While pain diminished by the 24-hour evaluation, the difference did not reach statistical significance. At 48-hour and 72-hour assessments, all patients in both groups reported a pain severity score of zero (Table 2, Fig. 1).
Discussion
This study aimed to investigate the effect of TENS on laparoscopy-related shoulder pain. Patients in both the TENS and control groups were assessed at intervals of 2, 4, 8, 24, 48, and 72 hours after surgery. The results revealed that TENS led to a reduction in shoulder pain at 2, 4, and 8 hours after laparoscopic surgery.
The etiology of laparoscopy-related shoulder pain is attributed to the stimulation of the phrenic nerve caused by excitation of the diaphragm or peritoneum. Diaphragmatic stimulation may result from direct injury, stretching, or CO2 gas exposure [1,2]. Non-pharmacological pain relief treatments are divided into two groups: counterirritants (e.g., acupuncture and TENS) and mind-body techniques (e.g., psychotherapy and relaxation). Acupuncture and TENS are deemed valuable owing to their minimal side effects. Depending on the stimulus used, the analgesic effects of TENS are mediated by two mechanisms: gate control and opiate-mediated pain control. Acupuncture-like TENS triggers pain relief by releasing endorphins and their precursors into the cerebrospinal fluid. However, in conventional TENS (C-TENS or gate-control TENS), pain is controlled via a gate control mechanism [3].
According to the gate control theory, non-painful input blocks nerve “gates”, preventing the transmission of pain to the central nervous system. After stimulation of the primary afferent fibers by a painful stimulus, the pain message reaches the brain via transmitting cells. Increased activity of transmitted cells leads to increased pain perception, while decreasing their activity alleviates pain. The gate, located in the dorsal horn of the spinal cord of the substantia gelatinosa, regulates the transfer of sensory information from primary afferent neurons to transmission cells. Closure of the “gate” blocks the entry of messages into the transmission cells, reducing pain sensation. Large (touch-, pressure-, and vibration-transmitting) and small (pain-transmitting) fibers control gate activity. Large fibers close the gate, whereas the small fiber opens it. Therefore, the increased activity of large-diameter fibers reduces pain [16,17]. TENS also activates large-diameter afferent fibers, thereby reducing pain [12].
Numerous studies have examined the efficiency of TENS in postoperative pain management. While some have yielded inconclusive results, others have shown positive results [12]. For instance, DeSantana et al. [18] found TENS effective in reducing the severity of pain after laparoscopic tubal ligation. Similarly, TENS exhibited pain-relieving effects after cholecystectomy [19] and in primary dysmenorrhea pain [20]. However, few studies have investigated the effect of TENS in reducing shoulder pain after gynecological laparoscopy. In a study conducted by Asgari et al. [2] in 2018, the effects of TENS and fentanyl on laparoscopy-related shoulder pain. In this study, pain intensity was measured using the VAS score and we did not find TENS to be more effective in reducing pain than fentanyl [2]; however, the results of our study revealed that despite the lower consumption of NSAIDS in the TENS group compared to the control group, the amount of pain in patients who used TENS to relieve pain was significantly reduced compared to the control group. Consistent with our findings, Platon et al. [21,22] demonstrated high-frequency TENS was effective in relieving pain after laparoscopic gynecological surgery and surgical abortions. Since a large number of women undergo gynecological laparoscopic surgery annually, shoulder pain is a common post-laparoscopic complication, and no single approach during and after surgery has been established to prevent or reduce pain severity. TENS can be of great help for these patients. In the current study, although TENS did not reduce the length of hospital stay, pain severity was significantly reduced, which increased patient satisfaction after surgery. The results of our study suggest that TENS at low intensity and high frequency significantly reduces postoperative shoulder pain. Therefore, this method is effective in reducing pain and increasing patient satisfaction.
Notes
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
The study approval was obtained from the Ethics Committee of Pars Advanced and Minimally Invasive Medical Manners Research Center (PAMIM) affiliated to Iran University of Medical Sciences (ID: 5022-G-1396).
Patient consent
Informed consent was obtained from all participants included in the study.
Funding information
The funding for this project was provided by the first author of this article (Abolfazl Mehdizadeh kashi).
Acknowledgments
The authors wish to thank Rasoul Akram Teaching Hospital Clinical Research Development Center (RCRDC), Iran University of Medical Sciences, for sample collection.