Intrapartum transperineal ultrasound: angle of progression to evaluate and predict the mode of delivery and labor progression
Article information
Abstract
Intrapartum ultrasonography serves as a valuable tool for the objective evaluation of labor progression and effectively identifies underlying factors, such as asynclitism, in cases of abnormal labor progression. Among the various ultrasound measurement techniques, the angle of progression (AOP) demonstrates favorable reproducibility and accuracy in assessing fetal head descent. In the context of abnormal labor, interventions differ across different stages of labor, emphasizing the importance of investigating the utility of AOP according to labor stages in this review article. Pre-labor assessment of AOP can be beneficial in terms of counseling for the timing of induction of labor, while a wider AOP value during the prolonged first stage of labor has demonstrated a positive correlation with successful vaginal delivery and shorter time to delivery. In the second stage of labor, the AOP has exhibited efficacy in predicting the mode of delivery and complicated operative deliveries. Furthermore, it has assisted in predicting the duration of labor, thereby highlighting its potential as a decision-making model for labor progression. However, further research is needed to investigate aspects, such as the determination of cutoff values, of AOP, considering the multifaceted characteristics of labor progression, which are influenced by complex interactions among maternal, fetal, and other contributing factors.
Introduction
Dystocia is prevalent among nulliparous women, accounting for more than 50% of all cesarean sections (CSs). This is often attributed to inadequate uterine contractions, abnormal fetal positioning, and cephalopelvic disproportion. Dystocia contributes to an elevated primary CS rate, and repeated CS is associated with the placental accreta spectrum, which is causally linked to increased rates of maternal morbidity and mortality; hence, the diagnosis, management, and prediction of dystocia are crucial in obstetrics [1,2].
Delayed labor is associated with an increased incidence of maternal and neonatal morbidity. Additionally, performing CS during the second stage of labor is associated with an increased risk of unintended uterine extension, bladder trauma, and prolonged operative time [3–6]. Furthermore, surgical intervention in women with arrested labor is associated with an increased risk of chorioamnionitis, endometritis, and postpartum hemorrhage [7]. Hence, early prediction and decision-making regarding the mode of delivery in cases of delayed or arrested first or second stages of labor and suspected abnormal fetal positioning can serve as strategies to mitigate the occurrence of maternal and fetal complications [8].
Classical digital vaginal examinations (DVEs) and ultrasound assessments are the primary methods that are used to predict labor progression. In general, the assessment of labor progression relies on measures such as cervical dilatation, fetal head descent (station), and fetal position evaluated using DVE. However, these methods are subject to interobserver variability based on the examiner’s experience. Moreover, they can cause discomfort in pregnant women and raise concerns regarding the potential risk of infection associated with an increased frequency of DVE [9–11].
Consequently, notable advancements have been made in the development of diverse intrapartum ultrasound methods to address the limitations that are associated with DVE [12,13]. Moreover, intrapartum transperineal ultrasound (ITU) allows mothers to actively participate in the labor process by visualizing the ultrasound screen, thereby alleviating maternal anxiety and enabling positive visual biofeedback, in addition to measurement [14]. The evaluation of fetal head descent incorporates various methods such as angle of progression (AOP), progression distance, head-symphysis distance, fetal head direction, head-perineum distance (HPD), and midline angle [8]. Among these, the AOP is a relatively user-friendly and highly reproducible approach. Hence, the objective of this review was to evaluate the utility of AOP in predicting the mode of delivery, delivery outcomes, and progression of labor.
Method of AOP (mid-sagittal vs. para-sagittal)
To measure the AOP, the pregnant woman is instructed to empty the bladder and assume a supine lithotomy position. After applying a sterile cover to the convex ultrasound probe, it is positioned vertically between the labia. The aim is to obtain a sagittal-view image from the position where the pubic bone and fetal head are most effectively visualized. The angle is measured by connecting the longest axis of the pubic bone with the bony part of the fetal head that is closest to the probe, indicating the greatest descent. This measurement is performed with and without uterine contractions to assess AOP under different conditions.
Two methods are used to obtain the AOP: the midsagittal and parasagittal methods. In the mid-sagittal method, the probe is positioned centrally, allowing for image acquisition. Conversely, in the parasagittal method, the probe is slightly tilted to either the left or right, enabling the acquisition of tilted images for analysis. The visual disparity between the two methods is as follows: in the midsagittal method, the angle measurement is based on the longest axis of the pubic symphysis, which appears less echogenic to the bony part of the fetal head that is closest to the cervix and encompasses the entire image in the midsagittal plane (Fig. 1A). Conversely, the parasagittal method involves measuring the angle between the longest axis of the pubic ramus, which exhibits higher echogenicity and is partially visualized in the parasymphyseal plane and bony part of the fetal head (Fig. 1B) [15]. In addition to the visual differences in ultrasound imaging, it has been observed that the parasagittal AOP (psAOP) tends to yield slightly larger angle measurements compared to the mid-sagittal AOP (msAOP) (101±16 vs. 98±16; P<0.001). Moreover, in the analysis to predict CS, msAOP exhibited marginally superior performance compared with psAOP. However, no statistically significant difference was observed between the two methods (area under the receiver operating characteristic curve [AUC], 0.732; 95% confidence interval [CI], 0.614–0.823 vs. 0.714; 95% CI, 0.622–0.805) [16]. In a comparative research analysis of the inter- and intra-observer reliability, manual psAOP demonstrated superiority over ms-AOP and the failure rate of obtaining images using automated psAOP, measured by ultrasound devices, was highest at 19% (single observer: AUC, 0.97; 95% CI, 0.95–0.98 vs. 0.93; 95% CI, 0.88–0.96 and two observers: AUC, 0.96; 95% CI, 0.93–0.98 vs. 0.74; 95% CI, 0.58–0.84) [17].
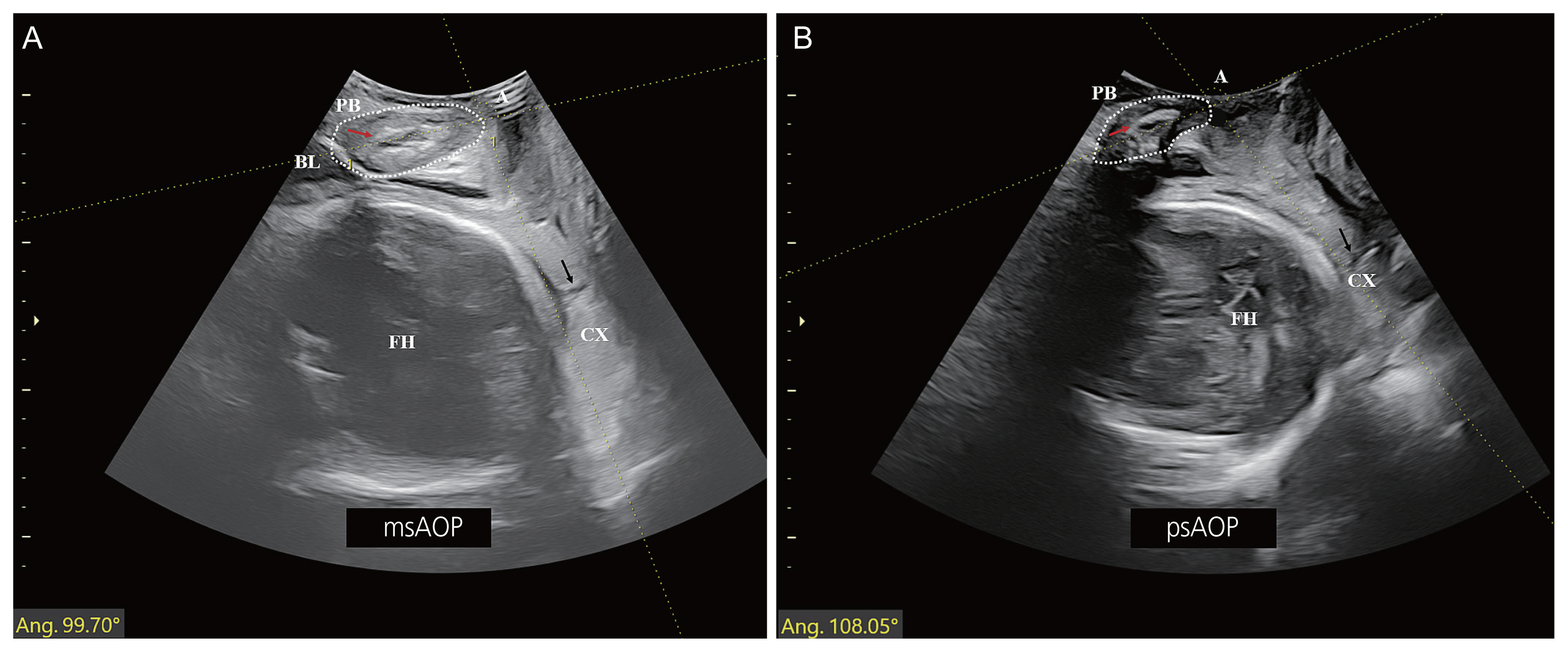
Characteristic features of the AOP on intrapartum transperineal ultrasound. (A) The angle measurement (white A) between the longest axis from the symphysis (red arrow) of the PB (white dot circle), which is ‘less echogenic’, to the bony part of the fetal head in the closest to the cervix, cervical canal (black arrow). (B) The angle (white A) using the longest axis from the ramus (red arrow) of the PB (white dot circle), which exhibits a higher echogenicity, to bony part of the fetal head, the cervical canal (black arrow). PB, pubic bone; A, angle; BL, bladder; FH, fetal head; CX, cervix; ms, mid-sagittal; AOP, angle of progression; ps, para-sagittal.
Consequently, in terms of obtaining images of the pubic bone, which serve as a reference for AOP measurement, ps-AOP, which displays more hyperechogenic images, may offer superiority in terms of reproducibility and accuracy. However, further research is warranted to compare its efficacy in accurately predicting delivery outcomes.
The usefulness of AOP according to labor stages
1. Before labor and First stage of labor
Rizzo et al. [18,19] conducted antepartum ultrasound measurements in singleton pregnant women at gestational ages between 36 weeks and 38 weeks. Nulliparous women who delivered after 40 weeks of gestation exhibited a significantly narrower AOP than those who delivered at before 40 weeks (93° vs. 95°; P=0.04). In multiparous women, a more substantial difference in AOP was observed (93° vs. 98°; P=0.029) [18,19]. In another study, involving nulliparous women at 38 weeks or beyond, it was observed that when the pre-labor measurement of AOP was less than 96°, the rate of CS deliveries reached 60% [20]. Hence, the prelabor assessment of AOP may contribute to the counseling of pregnant women before 40 weeks of gestation. However, Chan et al. [15] reported that pre-labor measurement of AOP is not a reliable predictor of the outcomes of induction of labor. Predicting delivery outcomes requires consideration of various factors related to labor, such as maternal and fetal factors and Bishop score. Thus, it is impractical to rely solely on AOP for outcome prediction.
Labor is composed of three stages: the first stage is defined as the period from the onset of labor to complete cervical dilatation (=10 cm) and is further delineated into the latent phase, occurring prior to reaching station 0, and the active phase, characterized by rapid cervical dilatation. Management of a prolonged latent phase of labor often involves options such as oxytocin administration or expectant management. However, decisions regarding the delivery method assume critical significance in the active phase. This is due to the fact that an abnormal labor pattern during the active phase ultimately contributes to a higher CS rate and an increased incidence of maternal and fetal complications related to delivery [21]. In this situation, AOP can be utilized as a tool for predicting delivery methods and time to delivery (TTD).
Successful vaginal delivery (VD) and TTD are closely related to cervical dilatation and fetal station. In a study comparing serial measurements of the AOP and DVE of cervical dilatation during the first stage of labor in singleton nulliparous women, a similar pattern was observed. Using a threshold of 119° for the AOP and 4 cm for the DVE as inflection points, it was observed that there was a significant average difference at 5.5 hours compared to 2.5 hours [22]. Moreover, the mean msAOP values of 124.3° corresponded to station 0, 145.6° to station +1, 149.4° to station +2, and 178.0° to station +3, during the active phase of the first stage of labor [23]. These studies suggest that AOP can serve as a reliable tool for assessing the progress of labor during the first stage.
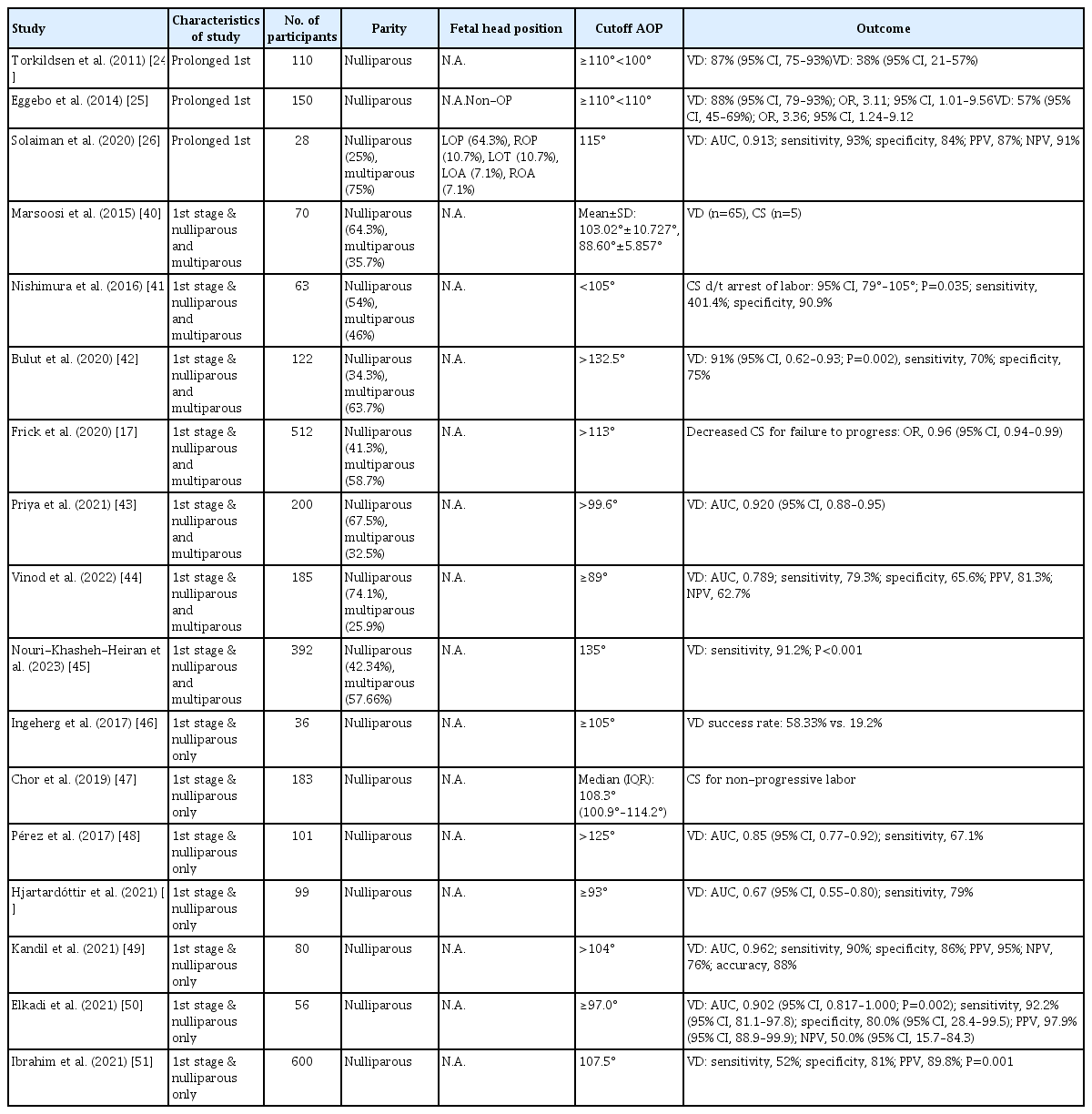
The clinical application of AOP as a predictive tool for labor can be categorized into two aspects: mode of delivery and TTD. Torkildsen et al. [24] conducted a study involving 110 and 150 nulliparous pregnant women. The investigation aimed to measure the AOP in cases of prolonged first stage of labor during the active phase, characterized by cervical dilatation ≥4 cm but with a cervical dilatation rate persisting <2 cm over a continuous 4-hour period. The findings revealed that in cases of AOP ≥110°, VD rates of 87% and 58% were observed. It can be inferred that there is a positive correlation between an increase in the AOP and a higher success rate of VD. Therefore, it was concluded that it is reasonable to proceed with labor and anticipate successful VD in pregnant women with an AOP exceeding this threshold, even in cases of prolonged first stage of labor. Notably, among pregnant women without occiput posterior positions, there was a significant increase in vaginal deliveries (odds ratio, 3.36; 95% CI, 1.24–9.12). This underscores the importance of fetal position as a significant determinant of successful VD [24,25]. In another study involving women with a prolonged first stage of labor, it was proposed that a cutoff value of 115° for AOP could serve as a predictive indicator for the success of VD (AUC, 0.913; sensitivity, 93%; specificity, 84%). Moreover, the measurement of AOP offers distinct advantages in cases of prolonged labor, as it enables the identification of notable features such as caput succedaneum and molding [26]. Several studies investigating the association between AOP and successful VD during the first stage of labor, particularly excluding prolonged labor, focused on nulliparous women and reported that AOP values ranging from 93° to 125° were correlated with VD. Conversely, studies conducted on parous women have proposed a cutoff value between 89° and 135° (Table 1).
As demonstrated by the aforementioned studies, the presence of various cutoff values for AOP indicates that the progression of labor is influenced by multiple factors. Frick et al. [17] reported that in a model combining maternal height, parity, gestational age, fetal weight, and AOP, the AUC was the highest at 0.8. Thus, to determine an appropriate cutoff value for AOP, further research is warranted to investigate more comprehensive models that incorporate multiple factors and their interactions.
In examining the association between AOP and TTD during the first stage of labor, a notable decrease in TTD was observed when utilizing a threshold of AOP ≥110°. In one study, for which pregnant women were stratified based on epidural anesthesia and oxytocin administration, it was found that among nulliparous women with epidural anesthesia, the mean TTD was 9 hours and 42 minutes, whereas those without epidural anesthesia had a mean TTD of 5 hours and 18 minutes. Among parous women, oxytocin administration resulted in a mean TTD of 3 hours and 18 minutes, whereas for those women to whom oxytocin was not administered, the mean TTD was 1 hour and 30 minutes. These observations were made using a reference AOP threshold of 125° [17,25]. With an AOP cutoff value of 93°, the TTD was observed as 12 hours and 12 minutes for nulliparous women and 8 hours and 26 mintues for multiparous women (Table 2) [22,27]. Therefore, there was a discernible negative correlation between AOP values and TTD.
2. Second stage of labor
Evaluating the progression of labor during the second stage can be challenging because of the occurrence of skull molding and caput succedaneum, which may result in decreased accuracies of DVEs [28]. Therefore, ITU, including that of AOP, allows for a more objective assessment of labor progression. Research studies focusing on AOP during the second stage of labor can be classified into three categories: determination of the delivery method, assessment of difficult instrumental delivery in prolonged labor, and evaluation of TTD.
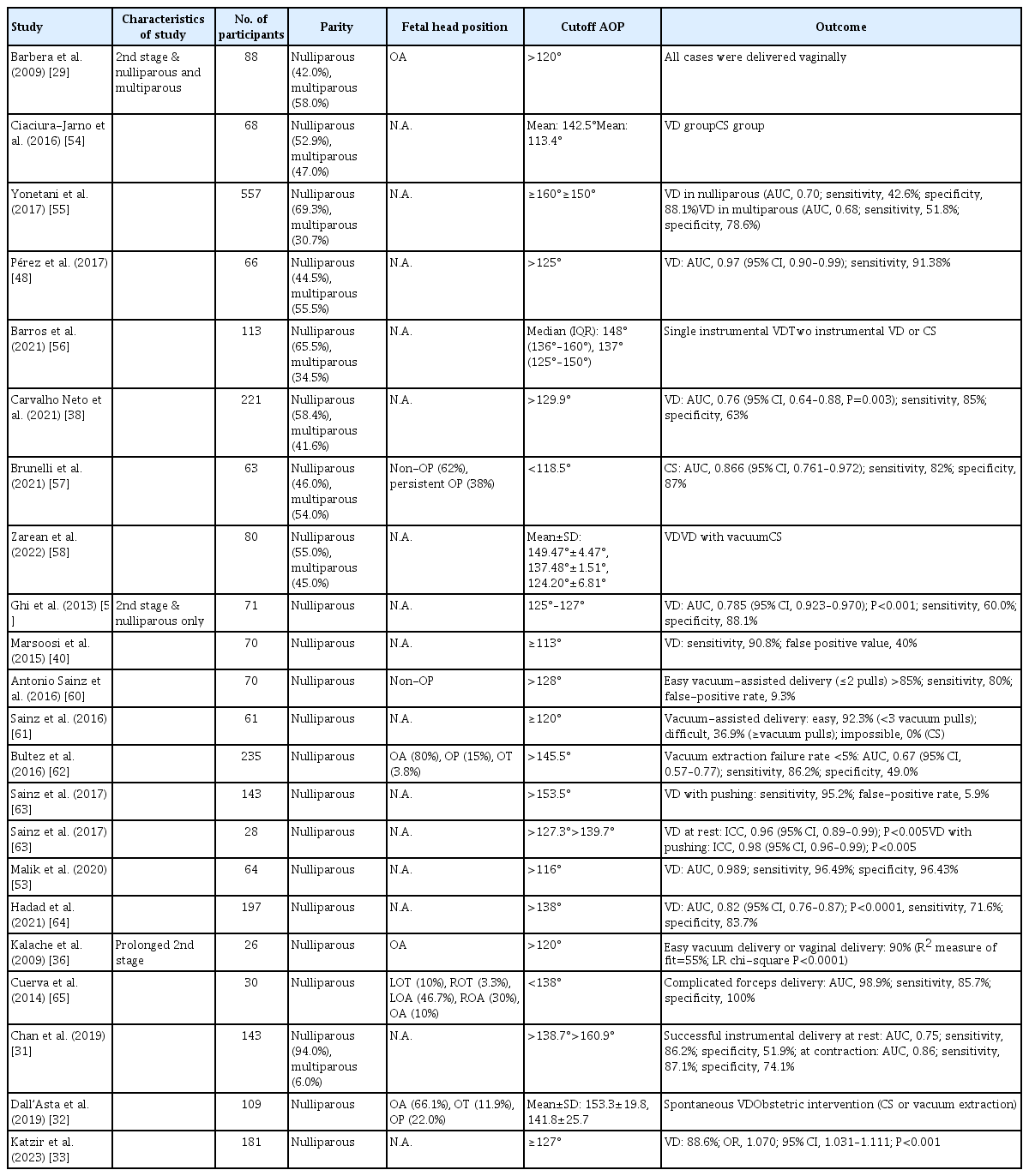
In a study involving 88 women, including both nulliparous and multiparous women, AOP was measured from the active phase of the first to the second stage of labor. Remarkably, successful VD was achieved in all cases in which the AOP exceeded 120° during the second stage of labor [29]. In a recent meta-analysis encompassing eight studies and 887 pregnant women, the diagnostic performance of AOP at the onset of the second stage of labor was analyzed. The results indicated a sensitivity of 80% (95% CI, 71–86%), a specificity of 81% (95% CI, 72–88%), and an AUC of 0.87, demonstrating the ability to predict spontaneous VD. Notably, the AOP range of 108°–119° exhibited the highest sensitivity of 94% (95% CI, 88–97%), whereas the range of 141°–153° demonstrated the highest specificity of 82% (95% CI, 66–92%). Moreover, when the AOP ranged from 141° to 158°, the probability of successful VD significantly increased from 22% to 87% [30]. In subsequent studies that focused on predicting the delivery method, the range of AOP values associated with successful VD was between 115° and 153.3° [26,31–33] (Table 3).
Prolonged second stage of labor is defined as the absence of delivery even after a duration of 3 hours in nulliparous women and 2 hours in multiparous women during the active phase when maternal “pushing” is attempted [34]. There is a higher risk of complications, such as third and fourth degree lacerations, postpartum hemorrhage, and maternal infection, owing to the increased duration of the second stage of labor. Hence, accurate decision-making is crucial in cases of prolonged second stage of labor [35]. In the case of nulliparous women experiencing a prolonged second stage of labor, it was found that when the measured AOP value surpassed 120°, the probability of achieving successful vacuum delivery or VD was consistently 90% or higher [36]. Subsequently, an AOP value of 138° or less could predict difficult forceps delivery with a sensitivity of 85.7% and a specificity of 100% (Table 4). It should be noted that, despite both studies focusing on nulliparous women, the variation in the AOP cutoff values between the previous research and Cuerva’s study can be attributed to the previous study exclusively targeting fetuses in the occiput anterior position.
Recently, the use of operative vaginal delivery (OVD) methods including forceps and vacuum extraction has decreased. However, by utilizing objective criteria based on the AOP, the appropriate application of OVD holds the potential to serve as an alternative approach for reducing the CS delivery rate. In a recent meta-analysis of seven studies and a total of 782 pregnant women, AOP was found to be capable of predicting uncomplicated OVD with a sensitivity of 80% (95% CI, 59–92%), specificity of 89% (95% CI, 76–95%), and a likelihood ratio positive (LR+) of 7.3 (95% CI, 3.1–15.8), indicating its predictive value for uncomplicated OVD during the resting state. During the pushing state, AOP demonstrated a sensitivity of 91% (95% CI, 85–94%) and specificity of 83% (95% CI, 69–92%), with a LR+ of 5.4 (95% CI, 2.7–10.6), indicating its predictive capacity. Significantly, in nulliparous pregnant women during the resting state, the AOP demonstrated notable performance indices, with a sensitivity of 87% (95% CI, 75–94%) and specificity of 90% (95% CI, 82–94%). Moreover, AOP >145.5° was associated with a post-test probability of successful VD of 98%, whereas AOP <120° was associated with a decrease in the post-test probability of uncomplicated OVD from 85% to 57%. Hence, AOP is a valuable tool for predicting successful and uncomplicated OVD. Its utility in clinical practice underscores its potential significance in guiding decision making and optimizing labor management [37].
In a recent study involving a cohort of 221 pregnant women, the relationship between AOP and duration of the second stage of labor was investigated. The findings revealed a statistically significant difference in duration based on AOP values. Specifically, when the AOP was <129.9°, the mean duration of the second stage of labor was measured as 103±88 minutes, whereas when the AOP was >129.9°, the mean duration decreased to 55±44 minutes (P=0.016) (Table 2). These results highlight the potential impact of AOP on the timing and progression of the second stage of labor. In this study, maternal height was a statistically significant factor (P<0.001) influencing the mode of delivery. However, it did not demonstrate a significant association with the duration of the second stage of labor. Conversely, the administration of labor analgesia emerged as a significant factor (P=0.005) affecting the duration of the second stage [38].
Influential factors in predicting labor progress with AOP
The delivery process is a multifaceted event that is influenced by a multitude of factors including maternal age, gestational age, maternal height, body mass index, parity, regional anesthesia, fetal weight, fetal position, and other relevant variables. In a recent study examining 261 pregnant women who underwent assessment of fetal head descent using ITU, several factors, including parity, methods of labor induction, epidural anesthesia, and obesity, were found to have a significant impact on labor progress. HPD, psAOP, and sonographic cervical dilatation were assessed in this study, and gestational age, parity, induction method (dinoprostone slow-release vaginal pessary vs. intracervical balloon), and obesity were found to have significant effects on HPD and cervical dilatation. However, no significant association was observed between an increase in psAOP and these variables. However, epidural anesthesia showed a significant correlation with slow fetal descent in both HPD and psAOP measurements. These findings indicate that the AOP, as a method for assessing fetal descent, may be less susceptible to the influence of other factors, suggesting its potential as a relatively unconfounded measure for evaluating fetal descent (P=0.04, P<0.01). These findings suggest that among the various methods for evaluating fetal descent, AOP is a superior approach that is less influenced by other factors [39].
Conclusion
ITU, particularly that examining the AOP, when used for evaluating labor progress allows effective biofeedback in pregnant women during labor. This is an easily implemented and highly reproducible method that is less influenced by other factors. Notably, a wider AOP has demonstrated a meaningful association with favorable outcomes, such as successful VD and reduced TTD. However, given the multifactorial nature of the labor process, a definitive and universally applicable cutoff value for AOP remains elusive. Therefore, further research is required to establish a comprehensive decision-making model that incorporates various factors.
Notes
Conflict of interest
No potential conflict of interests relevant to this article was reported.
Ethical approval
Due to the nature of the study as a literature review approval by an institutional review board was not required for this study.
Patient consent
Due to the nature of the study as a literature review the need for the patients’ informed consent was waived for this review article.
Funding information
None.