Fetal and maternal outcomes of segmental uterine resection in emergency and planned placenta percreta deliveries
Article information
Abstract
Objective
This study evaluated maternal and fetal outcomes of emergency uterine resection versus planned segmental uterine resection in patients with placenta percreta (PPC) and placenta previa (PP).
Methods
Patients with PP and PPC who underwent planned or emergency segmental uterine resection were included in this study. Demographic data, hemorrhagic morbidities, intra- and postoperative complications, length of hospital stay, surgical duration, and peri- and neonatal morbidities were compared.
Results
A total of 141 PPC and PP cases were included in this study. Twenty-five patients (17.73%) underwent emergency uterine resection, while 116 (82.27%) underwent planned segmental uterine resections. The postoperative hemoglobin changes, operation times, total blood transfusion, bladder injury, and length of hospital stay did not differ significantly between groups (P=0.7, P=0.6, P=0.9, P=0.9, and P=0.2, respectively). Fetal weights, 5-minute Apgar scores, and neonatal intensive care unit admission rates did not differ significantly between groups. The gestational age at delivery of patients presenting with bleeding was lower than that of patients who were admitted in active labor and underwent elective surgery (32 weeks [95% confidence interval [CI], 26–37] vs. 35 weeks [95% CI, 34–35]; P=0.037).
Conclusion
Using a multidisciplinary approach, this study performed at a tertiary center showed that maternal and fetal morbidity and mortality did not differ significantly between emergency versus planned segmental uterine resection.
Introduction
Placenta accreta spectrum (PAS) refers to placental attachment anomalies including placenta accreta, placenta increta, and placenta percreta (PPC). Approximately 0.4% of all pregnancies are affected by PAS [1]. The presence of placenta previa (PP) is associated with a 3.0% PAS risk in women with a previous single cesarean delivery, whereas the absence of PP is associated with a 0.03% PAS risk [2]. PAS is among the most important causes of postpartum hemorrhage and maternal mortality and considered a severe obstetric emergency [3]. Affected newborns experience prematurity, low Apgar scores, respiratory distress, neonatal intensive care unit (NICU) requirements, and a threefold increase in mortality [4,5]. The optimal delivery week becomes important when these factors are considered. However, consensus is lacking about this issue. The American College of Obstetricians and Gynecologists (ACOG) reported that delivery at 340–356/7 weeks is appropriate to preventing catastrophic maternal conditions in PAS cases. The procedure recommended by the ACOG for PAS is planned for post-cesarean hysterectomy [6]. Because an emergency labor risk scale is lacking for PAS, it is not possible to determine emergency delivery indications. However, conditions such as antenatal bleeding, active labor, or premature preterm rupture of the membranes (PPROM) may require emergency delivery in cases of PAS.
Recommendations for managing PAS-associated PP are diverse and primarily based on case series, reports, and specialists’ personal experience and clinical opinions. The desire of some patients to maintain their fertility has led to conservative treatment. Bakri balloon placement, segmental myometrial resection, placental bed suturing, uterus-sparing surgery [7], and long-term postpartum follow-up after leaving the placenta in place in cases of advanced invasion are among the current management options [8,9]. The success rate of uterus-sparing surgery is reportedly 78.4–80.0% in the literature [10–12].
Studies have examined the fetal and neonatal outcomes of emergency or planned cesarean hysterectomies in patients with PAS. However, the results of emergency or planned cesarean hysterectomies for PAS performed by multidisciplinary teams are conflicting [13,14]. This study aimed to evaluate the maternal and fetal outcomes of emergency and planned PPC cases in which uterine-sparing surgery was performed via segmental resection.
Materials and methods
Patients diagnosed with PPC or PP who underwent emergency or planned segmental uterine resection were included in this retrospective study. The study included patients who underwent surgery between January 1, 2013 and January 30, 2023, at the obstetric gynecology service of the Medical Faculty Hospital. The International Federation of Obstetrics and Gynecology guidelines (grades 4, 5, and 6) were used to diagnose PPC [15]. Patients’ past demographic and obstetric data were obtained from hospital records. Transvaginal ultrasonography was used to diagnose PP with the placenta close to the internal cervical os. As the diagnostic criteria for PAS, loss of the echolucent region between the uterus and placenta and thinning and interruption of the hyperechoic interface between the uterine serosa and bladder wall are used to show grayscale and color Doppler images. The observation of bridging vessels with increased vascularity in this region and monitoring of lacunae with turbulent flow in the placenta support this diagnosis.
Patients whose diagnoses were confirmed based on intraoperative findings were included. PPC cases with a fetal anomaly, twin pregnancy, and PAS diagnosis <24 weeks (viability limit in our clinic, 24th gestational week) and those who underwent hysterectomy were excluded. Patients with PAS but without a postpartum pathological diagnosis of PPC were excluded. The patients were divided into two groups: cesarean section on the planned day and emergency surgery. Emergency cases consisted of patients who had active bleeding or active labor and delivered on the day of admission. Most planned cases were followed up in our clinic (planned delivery week for PAS in our multidisciplinary clinic: 34–36 weeks). Patients that were difficult to reach because of their location, history of premature birth, or comorbidities were hospitalized 1 day or a few days before delivery. Although our planned delivery week was 34–36 weeks, patients with fetal or maternal comorbidities were hospitalized and underwent planned surgery earlier.
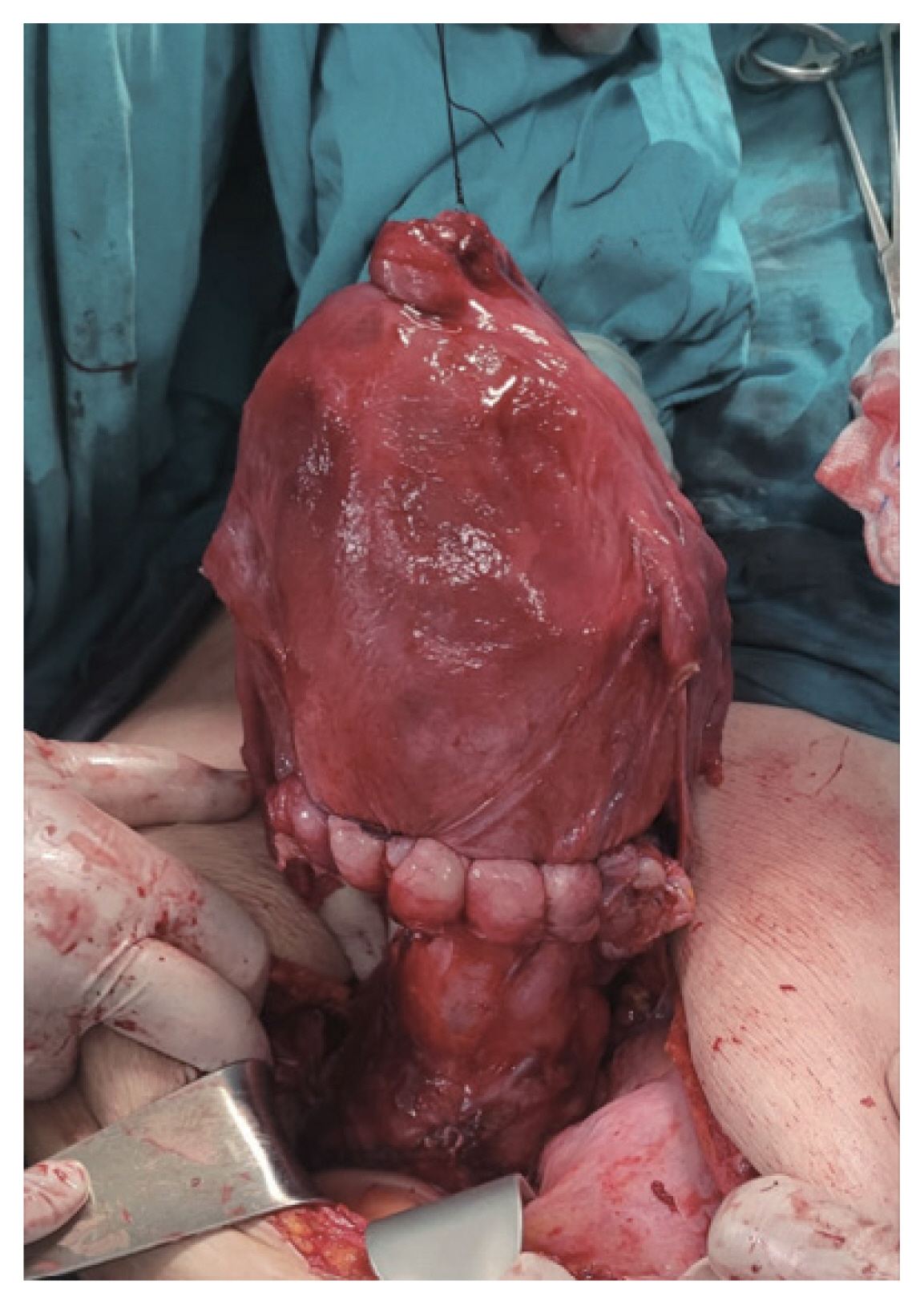
Uterine-sparing surgery is performed by a multidisciplinary team in our clinic, and cesarean hysterectomy is performed in cases in which bleeding cannot be controlled as previously described for PAS [16]. After a preoperative evaluation by the urology team, we inserted a cystoscope-guided bilateral ureteral catheter in cases of suspected bladder or parametrium invasion (this not possible in some very urgent cases). After receiving anesthesia, patients undergoing uterine-sparing surgery were positioned in the lithotomy position (anesthesia type decided individually for all patients by the anesthesiologists as spinal, general, or combined). The abdomen was opened via a midline incision below and above the umbilicus, and the uterine cavity was accessed via a vertical fundus incision. After fetal removal, the fundal cut was closed using sutures. The bladder flap was separated from the anterior surface of the uterus via a ligament beginning in the paracervical region. Once the uterine artery was reached, a clamp was placed on the cervical area of the uterus. Following the resection of the uterine segment containing the placental bed, placental bed sutures were placed, the uterine incision was primarily closed, and the procedure was completed (Figs. 1, 2). In cases involving bladder invasion, the bladder was opened under control, the placental tissue was removed, and the bladder underwent reconstruction following bleeding control. Methylene blue was used to assess urinary bladder leakage. The urethral catheter was left in place for 3–4 weeks.
All demographic data were compared between the emergency and planned cases. Admission complaints of patients who visited the emergency department were evaluated considering bleeding and active labor status. Hemorrhagic morbidities, intra- and postoperative complications, length of hospital stay, and surgical duration were evaluated in all patients. Perinatal and neonatal morbidity and mortality rates were compared.
1. Statistics analysis
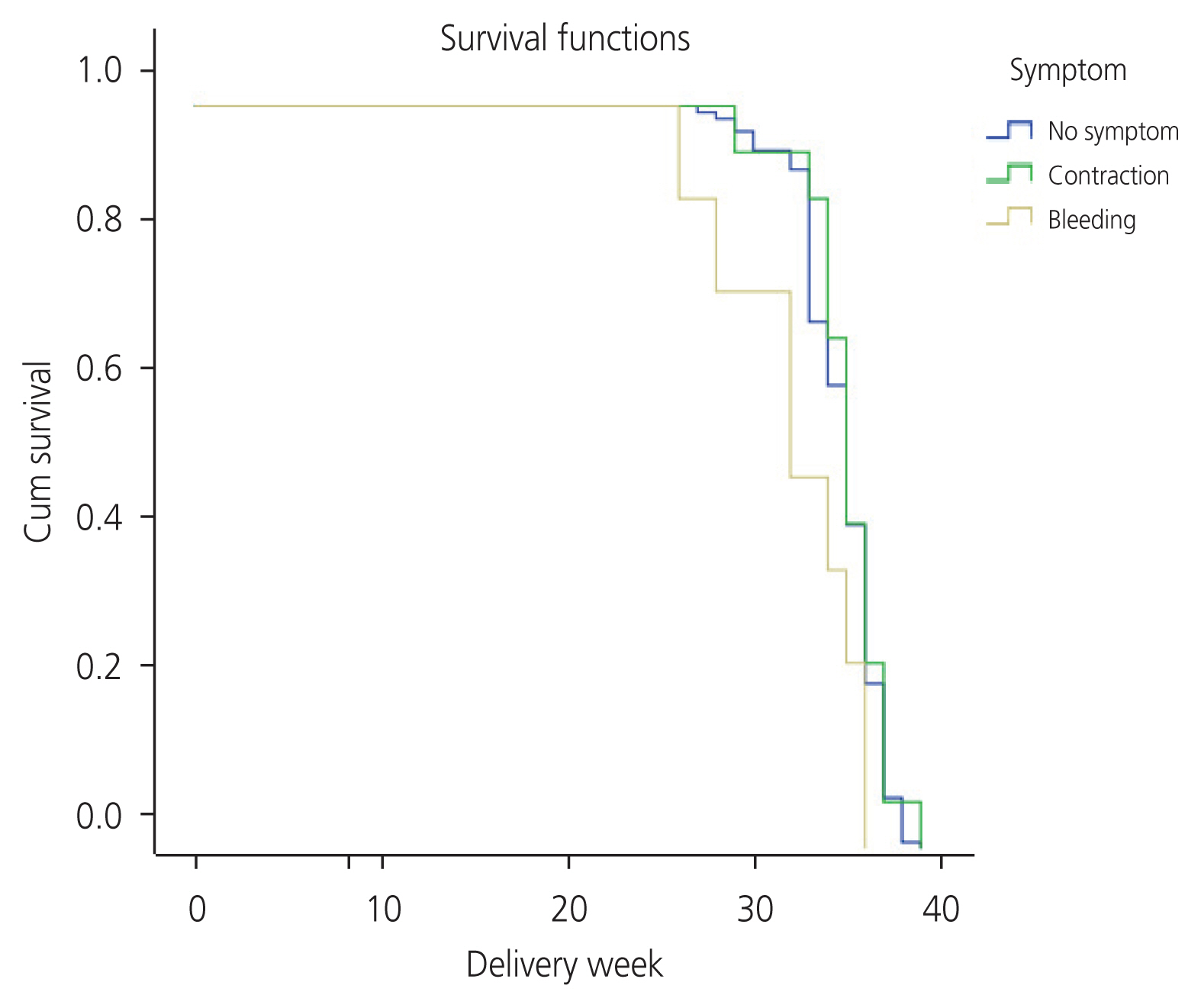
SPSS version 0 (SPSS, Chicago, IL, USA) was used for the statistical analysis. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used for the normality analysis. The Kolmogorov-Smirnov test was mostly used for comparing normally distributed data, whereas the Shapiro-Wilk test was mostly used for intragroup comparisons. Statistical significance was set at P<0.05, and the data were not normally distributed. Student’s t-test was performed to compare normally distributed data, which are shown as mean±standard deviation (SD). If the data were not parametric, the Mann-Whitney U-test was used, and the values are presented as median (minimum–maximum). The chi-squared and Fisher’s exact tests were used to determine whether the categorical variable distributions differed between groups. Kaplan-Meier statistics were used to analyze birth timing in the planned and emergency birth groups, and their importance was determined using the log-rank test. Values of P<0.05 were considered statistically significant.
Results
A total of 216 patients with PAS were included in this study. Based on the postoperative pathology results, 20 (9.2%) placenta accreta and 35 (16.2%) placenta increta cases were excluded from the study. One hundred and sixty-one (74.6%) PPC cases managed as emergency or planned cases were included in this study. Correct prenatal diagnoses were made for the entire study group. Postpartum pathology confirmed this diagnosis. Hysterectomies were performed in 20 patients (12.4%). When patients who underwent hysterectomy were excluded from both groups, 25 (17.73%) of 141 patients underwent emergency surgery and 116 patients (82.27%) underwent planned segmental uterine resection.
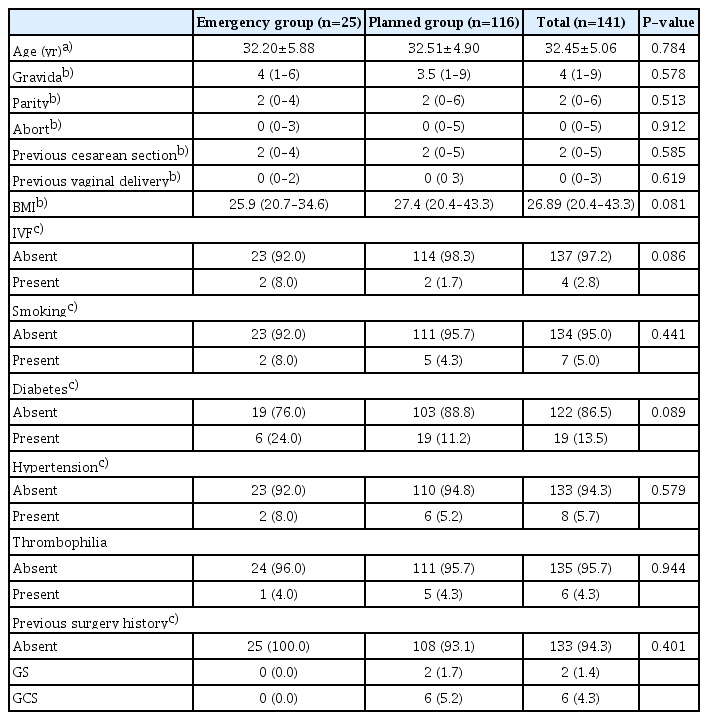
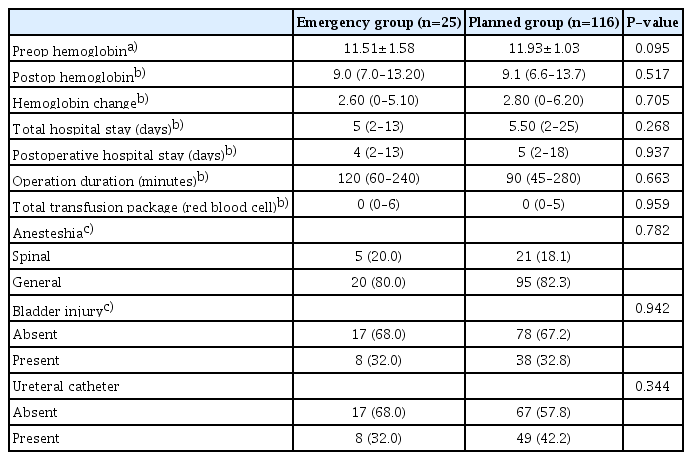
The demographic and obstetric histories of all the patients are shown in Table 1. Gravida, parity, and previous cesarean section numbers were similar in all cases. Of the emergency patients, 36% (n=9) presented with bleeding and 64% (n=16) presented with pain. Although preoperative hemoglobin values were low (mean±SD: 11.51±1.58 vs. 11.93±1.03 g/dL, P=0.095) in the emergency group, they did not differ significantly from those who underwent planned surgery. Postoperative hemoglobin changes of the emergency and planned groups were median (min–max) 2.60 g/dL (0–5.10) vs. 2.80 g/dL (0–6.20), respectively. The mean operation times were 120 minutes (range, 60–240) vs. 90 minutes (range, 45–280), while the mean total hospital stays were 5 days (2–13) vs. 5.50 days (2–25), respectively; the differences were not significantly different (P=0.268) (Table 2). Bladder damage rates were similar between groups. None of the patients required rehospitalization for postoperative complications.
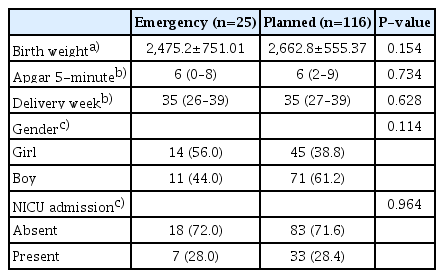
When neonatal outcomes were evaluated, the median fetal age at delivery was 35 weeks (26–39); that in the emergency group was 35 weeks (26–39), while that in the planned group was 35 weeks (27–39). The mean 5-minute Apgar scores did not differ between groups (P=0.628). Overall, 28.0% (n=7) of newborns in the emergency group versus 28.4% (n=33) of newborns in the planned group were admitted to the NICU; the difference was not significant. No neonatal deaths were observed (Table 3). Kaplan-Meier statistics were used to analyze birth timing in the planned and emergency birth groups, and their importance was determined using a log-rank test. The delivery week of patients presenting with bleeding was significantly lower than that of patients who were admitted in active labor and underwent elective surgery (32 weeks [95% confidence interval [CI], 26–37] vs. 35 weeks [95% CI, 34–35]; P=0.037) (Fig. 3).
Discussion
The optimal management of PAS remains controversial. In this study, we observed no differences in maternal and neonatal morbidity and mortality rates when planned versus emergency segmental uterine resection surgery was performed in planned in patients with PPC and PP.
Many studies in the literature compared the emergency or planned outcomes of cesarean hysterectomy cases; however, none have examined uterine-sparing segmental resection. Dawood et al. [17] stated that patients treated conservatively did not require intensive care, experienced less bladder damage, and had a shorter surgical duration. Studies by Kilicci et al. [18] and Karaman et al. [19] comparing segmental uterine surgery with cesarean hysterectomy support these findings. In cases in which PAS is suspected during cesarean section, the majority of Society for Maternal-Fetal Medicine members reported continuing with cesarean hysterectomy, while 15.0–32.0% prefer conservative treatment [20]. However, there are important differences between obstetricians and maternal-fetal subspecialists. Being in a high-or low-income country and having limited access to various treatments contribute to this difference. The safest and most feasible option for the majority of low-and middle-income nations is primary planned cesarean hysterectomy when diagnostic testing, follow-up care, and additional treatments are unavailable.
Studies have shown that delivery using a multidisciplinary approach leads to a shorter surgical time, less maternal hemorrhagic morbidity, and fewer intensive care admissions. In a large retrospective cohort study conducted between 1996 and 2008 in Utah, the maternal morbidity rate was lower among women with PAS who delivered in tertiary care centers using a multidisciplinary team approach than in those who delivered using standard obstetric care at other hospitals [21]. Additionally, in referral centers, clinical outcomes improve over time as multidisciplinary teams accumulate experience treating PAS cases. The regionalization of care for women diagnosed with PAS is strongly supported by these data [22].
In PAS surgery, cases can require urgent delivery owing to bleeding, active labor, PPROM, and unpredictable fetal or maternal conditions. Thang et al. [23] reported that there were 2.5 times more emergency deliveries among PAS cases with antenatal bleeding and 5.2 times more deliveries at <37 weeks. Similarly, Bowman et al. [24] and Wang et al. [25] reported that the risk of emergency delivery was high among patients with antenatal hemorrhage and PPROM. Flores-Mendoza et al. [26] reported that, among patients with PAS who underwent emergency (n=25) and planned (n=100) cesarean hysterectomy, 80.0% of the former versus 26.0% of the latter presented with antepartum hemorrhage. Our patients underwent surgery because of active labor rather than bleeding. Remarkably, the delivery week of the emergency patients presenting with bleeding was significantly lower.
The literature emphasized that maternal and fetal outcomes were better in the planned group of PP cases with or without PAS despite different treatment methods, while the need for hysterectomy and blood transfusion was higher in the PAS group treated with emergency surgery [5]. Other retrospective studies support this finding; when cases of emergency versus planned delivery without prenatal diagnosis and those of planned delivery were compared, less blood was needed in the planned group [27]. Flores-Mendoza et al. [26] observed that intra- and postoperative hemoglobin levels were lower, the rate of blood loss was higher, the need for general anesthesia was higher, bladder damage was more frequent, and the length of hospital stay was longer in the emergency group. The record of prenatal bleeding episodes could not be found. The authors attributed this finding to the fact that the diagnosis was missed in the unexpected group. As some cases were diagnosed intraoperatively, the bleeding was excessive during hysterectomy following hysterotomy performed to remove the fetus [28]. Wang et al. [25] reported that, although the blood loss rate was higher among emergency PAS cases with an early gestational age, blood loss did not differ significantly between the emergency and planned groups and that birth planning should be performed according to PAS severity. They attributed the similarity in maternal and fetal outcomes in emergency and planned delivery cases to the early recognition and termination of severe cases to avoid emergency delivery. The authors reported an emergency delivery rate of 30.0% in all cases [25].
The optimal delivery time for the coexistence of PAS and PP should be individualized according to the degree of placental invasion and patient’s condition. While some authors recommend delivery at 34–35 gestational weeks in PAS cases, others suggest that delivery be considered at 36 weeks in the absence of risk factors [29]. Morlando et al. [14]. evaluated neonatal outcomes and reported that NICU hospitalization duration was longer in the emergency group, while the mean 5-minute Apgar score and birth weight were lower in deliveries at 24–34 gestational weeks. Neonatal morbidity and mortality rates did not differ between emergency and planned deliveries in the 34–36 weeks group. In a study by Shamshir saz et al. [13], the neonatal composite morbidity rate was 78.9% in the emergency group and 45.8% in the planned group. The delivery week in the emergency group was 32 weeks, while that in the planned group was 34 weeks. NICU hospitalization rates and lengths of hospital stay were higher in the emergency group. No neonatal deaths were observed in the planned group [13]. In our study, the NICU admission rate was 28.0% in the emergency group and 28.4% in the planned group. The mean 5-minute Apgar scores did not differ between groups.
Our study had some limitations. First, it was a retrospective study. Prenatal bleeding episodes could not be reached in all cases, and our cesarean hysterectomy results could not be presented in emergency and planned cases because of the small number of cases; our rate was high because ours was the only referral center in our region and our study series consisted of total PP and PPC cases (PAS cases without PP could not be included).
This study showed that emergency versus planned delivery did not affect maternal and fetal morbidity and mortality except in cases of prematurity among patients who underwent segmental uterine resection using a multidisciplinary approach in a tertiary center and that the planned surgery week was also ideal for the delivery timing. Considering the catastrophic results of PAS surgery, we believe that experienced teams should intervene in such cases. Further studies are needed to confirm standard follow-up and treatment outcomes.
Notes
Conflict of interest
The authors state no conflict of interest.
Ethical approval
Permission for this study was obtained from the NEU Ethics Committee under decree No. 2022/3940 (10996).
Patient consent
Consent was obtained from all patients.
Funding information
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.