Incidentally detected ganglioneuroma during pregnancy: A case report
Article information
Abstract
Retroperitoneal ganglioneuroma is a rare benign tumor, which is included in the neuroblastomas group. It can occur anywhere along the peripheral autonomic ganglion sites, and the tumor is often incidentally detected in asymptomatic patients or may produce symptoms related to the slow growing tumor. Surgical excision is the treatment of choice and the prognosis is good. We report a case of retroperitoneal ganglioneuroma, which was incidentally detected in the first trimester of pregnancy in a 29-year-old woman. Surgical resection of the ganglioneuroma was done at the time of cesarean section at full term without complications.
Introduction
Ganglioneuromas are rare benign tumors of the peripheral nervous system. Ganglioneuromas are fully differentiated from neuroblastomas and ganglioneuroblastomas, and grow wherever sympathetic nervous tissue is found [1]. They most frequently occur in the abdomen in sites such as the adrenal gland and paraspinal retroperitoneum (sympathetic ganglia), and also occur in the posterior mediastinum, head and neck [2]. Retroperitoneal ganglioneuromas are often incidentally detected and are usually asymptomatic [3]. Normally ganglioneuromas are non-functioning, with up to 39% secreting catecholamines [3]. Surgical excision is the treatment of choice and their prognosis is good [1,4,5].
We report a case of incidentally detected ganglioneuroma in the first trimester of pregnancy. And a surgical resection of the ganglioneuroma was done at the time of the cesarean section at full term, without complications.
Case report
A 29-year-old pregnant woman visited the local hospital to confirm her pregnancy. On ultrasound the pregnancy was confirmed (6 weeks), and a pelvic mass was incidentally detected without any symptoms. The patient was transferred to our tertiary hospital for evaluation of the incidentally detected pelvic mass. Ultrasound revealed that there was an about 8 weeks sized embryo in the uterus and a 10 cm sized hypoechoic mass on the left, posterior to the uterus. But it was difficult to distinguish the mass from an adnexal mass, leiomyoma (intraligamentary), or other tumor by the ultrasonographic findings. We checked her serum tumor marker, and performed magnetic resonance imaging. Serum CA-125, CA-19-9, CA-72-4, and carcinoembryonic antigen were within normal range. A pelvic MRI without contrast media was checked at 11 weeks of pregnancy. Magnetic resonance imaging (MRI) revealed an about 10×10 cm sized mass in the retroperitoneum, and an anteriorly displaced uterus and rectum. This mass had high signal intensity on a T2-weighted image, and there was extension to the central spinal canal through the S3 left neural foramen. The MRI suggested a benign retroperitoneal neurogenic tumor (Fig. 1A). After we consulted with the urology and neurosurgery departments, we decided to remove the retroperitoneal mass after delivery or at the time of the cesarean section. The patient underwent routine antenatal care without complications or symptoms, and there was no growth of the retroperitoneal mass on ultrasonography. The patient delivered a male baby with body weight of 2,940 g by cesarean section at 38 weeks of gestation and the retroperitoneal mass was excised with assistance from the urology team. The intraoperative frozen biopsy suggested a ganglioneuroma. Grossly, the resected mass was multiply fragmented, measuring 10×7×6 cm in the largest piece, partly encapsulated, and showed a whitish yellow and gelatinous cut surface. The histology report confirmed the ganglioneuroma (Fig. 1B, C). We could not completely resect the deepest portion due to the possibility of injury to normal tissues (nerves and vessels). The patient was discharged on the 7th postoperative day in good condition. We planned regular follow-up without additional treatment. She will be checked with a computed tomography three months later.
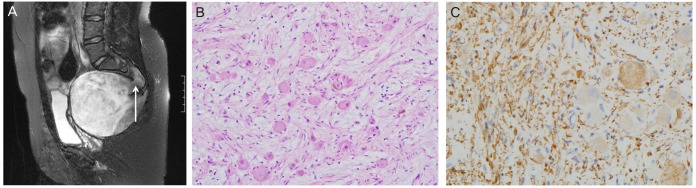
Pelvic magnetic resonance imaging (MRI) and histopathologic findings. (A) Sagittal T2-weighted MRI shows about 10×10 cm sized round retroperitoneal mass, it has high signal intensity and, extension to the central spinal canal through the S3 left neural foramen (arrow). (B) Microscopic findings of the tumor, showing ganglion cells (H&E, ×200). (C) Neurofilaments, stained positive for S-100 protein (immunoperoxidase staining, ×400).
Discussion
Ganglioneuroma is a tumor of the sympathetic nerve fibers arising from neural crest cells [1]. It may arise de novo and result from the maturation of a neuroblastoma or ganglioneuroblastoma [6]. The incidence of ganglioneuromas is unknown but they are rare. They are tumors of children and young adults, and rarely occur in adults [5,7]. Ganglioneuroma is fully differentiated and is a benign tumor [6]. It can be detected wherever sympathetic nervous tissue is found. It most frequently occurs in the posterior mediastinum, followed by the retroperioneum, adrenal medulla, head and neck. Most ganglioneuromas are non-functioning tumors, with up to 39% of them secreting catecholamines [1,3]. During surgery these catecholamines can cause hypertensive crisis [4]. In this case we did not check the serum catecholamines, but the patient had no vasoactive symptoms before surgery and no hypertensive crisis during surgery. Gnglioneuromas in nonpregnant patient are usually asymptomatic until they reach a large size, they may cause symptoms due to local expansion and compression of surrounding structures. So they are often detected incidentally [4]. Because imaging procedures are being used more widely, incidentally detected ganglioneuromas have increased [5,8].
There are only four articles about ganglioneuroma during pregnancy in English on PubMed (Table 1) [9,10,11,12]. Patients in the articles had no symptoms, had incidental detection of their tumors, and underwent resection of the mass.
The ultrasonogram of ganglioneuroma shows a hypoechoic, homogenous, and well circumscribed mass. But it is hard to distinguish ganglioneuroma from other masses, such as an adnexal mass or leiomyoma. There are no known universal markers for the differential diagnosis. Computed tomography scanning is commonly used to evaluate neuroblastic tumors, but in this case, the patient was pregnant, so we checked the MRI. On MRI, the ganglioneuroma appeared homogeneous and had low signal intensity on T1-weighted images. On T2-weighted images, the signal intensity is dependent on the ratio of myxoid stroma, cellularity and collagen fibers. Tumors with intermediate to high signal intensity on T2-weighted images have higher cellularity or collagen fibers, and markedly high T2 signal intensity tumors have abundant myxoid stromal component [13]. In this case, the MRI showed high signal intensity in the retroperitoneal mass on T2-weighted images, and it showed extension to the central spinal canal. The MRI findings suggested a benign neurogenic tumor.
Ganglioneuromas can also uptake iodine-tagged metaiodobenzylguanidine, but using this is not an option during pregnancy due to the exposure to radiation [4,9]. The treatment of choice is surgical resection, when it is possible. In this case the ganglioneuroma was too large and might cause dystocia, so we decided to remove the mass at the time of cesarean section. Since ganglioneuroma is a benign tumor, preoperative or postoperative chemotherapy or radiotherapy does not have a role. If surgical removal is difficult, it may be observed without an operation due to the good prognosis of the tumor.
Notes
No potential conflict of interest relevant to this article was reported.
