Hybrid laparoscopic myomectomy: A novel technique
Article information
Abstract
The objective of this study was to report on a new surgical technique, hybrid laparoscopic myomectomy that integrates the advantages of transumbilical laparoendoscopic single-site surgery and those of isobaric laparoscopy, and the initial experience with 14 cases. All of the procedures were performed by a single surgeon who has over 18 years of experience in laparoscopic surgery and 4 years of experience in laparoendoscopic single-site surgery. All cases of hybrid laparoscopic myomectomy were completed safely and effectively without conversion to conventional laparoscopic procedure. The median operative time was 75 minutes (range, 30 to 100 minutes). No postoperative complication was observed. The findings show that hybrid laparoscopic myomectomy is a safe and feasible surgical technique, and therefore can be a feasible, minimally invasive alternative to either abdominal or laparoendoscopic single-site surgery myomectomy.
Introduction
Although the feasibility of laparoendoscopic single-site surgery (LESS) myomectomy has been confirmed in selected patients [12], laparoscopic myomectomy through a single-port approach remains technically difficult. Isobaric laparoscopic myomectomy is a suitable option for the surgical treatment of symptomatic myomas and offers advantages over open surgery or conventional laparoscopic myomectomy [345]. However, in isobaric laparoscopic myomectomy, visible scars remain at the suprapubic incision site [5] or the other trocar sites [34]. We introduced a new surgical technique, hybrid laparoscopic myomectomy, which integrates the advantages of LESS with a pneumoperitoneum and those of isobaric LESS using conventional laparotomy instruments. More recently, Kang et al. [6] have demonstrated the feasibility of a surgical technique that combined single-port laparoscopy and laparotomy, although the technique differs from hybrid laparoscopic myomectomy and not all of the steps are completed using LESS. Hybrid laparoscopy for myomectomy is a new type of surgery and this represents the first described cases of myomectomy using this novel technique.
Materials and methods
In this study, 14 consecutive patients underwent hybrid laparoscopic myomectomy performed at Eulji University Hospital between April 2014 and December 2014. All of the procedures were performed by a single surgeon (YS Yang) who has over 18 years of experience in conventional laparoscopic, general, and vaginal surgery, and 4 years of experience in LESS. The surgical indication for hybrid laparoscopic myomectomy was determined on the basis of the presence of subserosal or intramural myoma with symptoms. A history of pelvic surgery or the presence of multiple myomas (≥3 per patient), or large myoma measuring 8 cm or more on ultrasonographic examination were not considered a contraindication for hybrid laparoscopic myomectomy. However, women who had a submucosal myoma were excluded. This study was approved by the institutional review board of Eulji University Hospital (2015-02-006-001).
1. Operative techniques
Hybrid laparoscopic myomectomy was designed by integrating the surgical techniques of the LESS removal of a myoma and those of isobaric laparoscopic suturing by using conventional laparotomy instruments. For the LESS removal of a myoma (Fig. 1A), the use of a homemade glove port laparoscopic system and the glove port technique was established in previous reports by our group [67], through a 2- to 2.5-cm transumbilical incision. The homemade [78] glove port system was established as described in previous reports [910]. For the isobaric laparoscopic suturing with a conventional laparotomy needle holder, a simple abdominal wall-lifting method was conducted through the same 2- to 2.5-cm transumbilical incision. The abdominal wall around the umbilical incision was lifted by using a Richardson retractor (Fig. 1B, C). Hybrid laparoscopic myomectomy was performed with the following steps. The LESS removal of a myoma was performed using conventional, rigid, straight instruments in the same fashion as multiport laparoscopic myomectomy (Fig. 1A). The isobaric laparoscopic suturing was achieved by use of a large curved needle with the conventional laparotomy long needle holder and a laparoscopic traumatic grasper (Fig. 1B, C). Introducing the surgeon's index finger through the umbilical wound allows an extracorporeal or intracoporeal knot tying with the similar accuracy and strength as in laparotomy (Fig. 1C-E). The myomas were extracted through the umbilical wound, and then the incision was closed.

Enucleation performed by applying traction on the myoma with two conventional laparoscopic clamps (A). Suturing of the uterine defect by using a conventional laparotomy needle holder under isobaric laparoscopic observation (B). Intracorporeal knot tying with the aid of the surgeon's index finger introduced through the transumbilical wound (C, D). Uterine defect closed by two- to three-layered suturing (E). The umbilical incisions at 3 months after hybrid laparoscopic myomectomy (F).
2. Statistical analysis
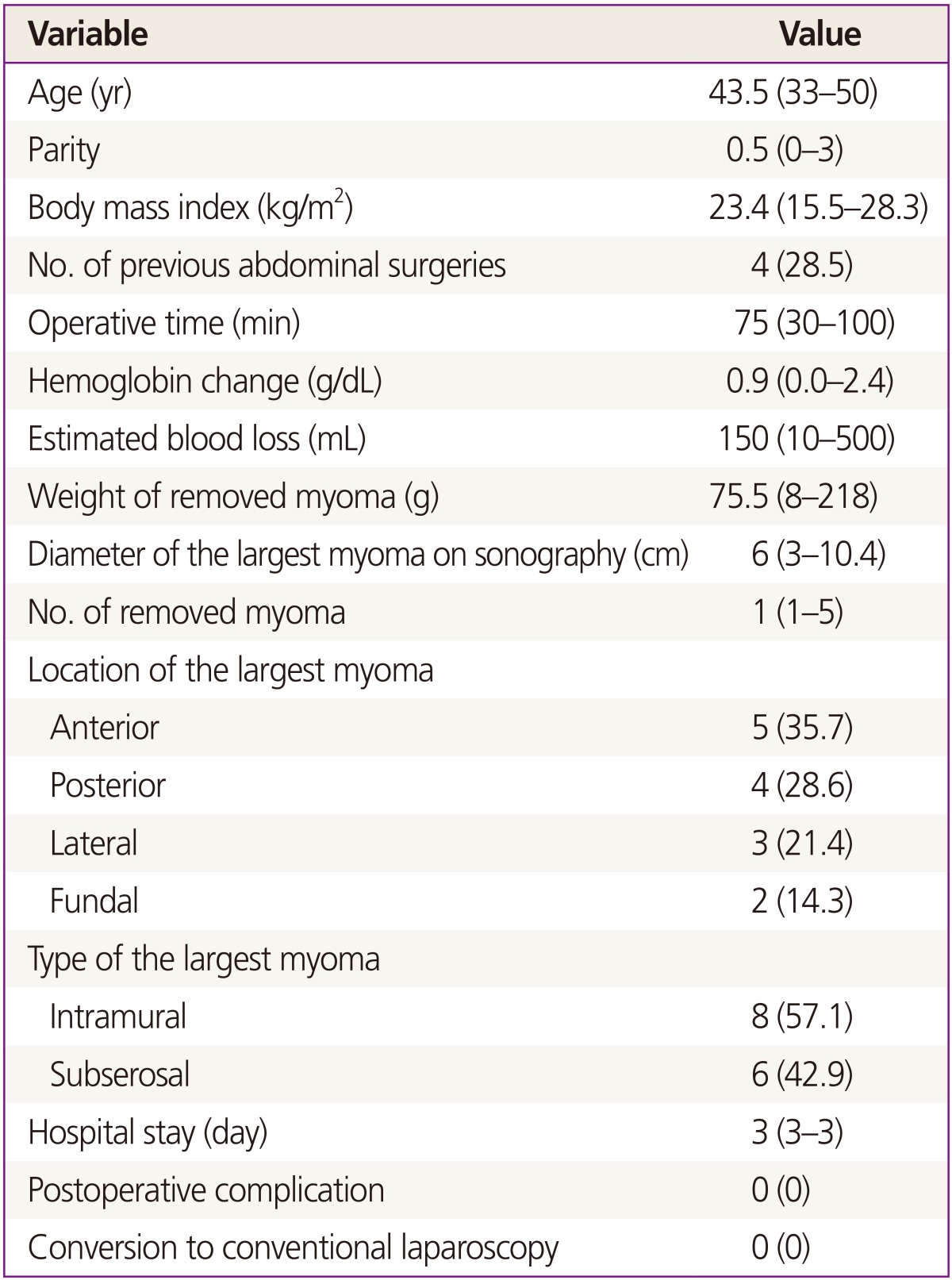
Patients' demographic and physical characteristics were obtained preoperatively. The number of removed myomas, weight of the removed myomas, location and type of the largest myoma, total operative time, estimated blood loss, hemoglobin concentration on postoperative day 1, length of postoperative hospital stay, and intraoperative and postoperative complications were also obtained. All statistical analyses were performed by using commercially available software SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarize the patient's demographics and operation results. All data were analyzed and reported as number (%) or median (range).
Results
The characteristics and surgical outcomes of the patients are listed in Table 1. The median age of the patients was 43.5 years (range, 33 to 50 years), and the median body mass index was 23.4 kg/m2 (range, 15.5 to 28.3 kg/m2). The median weight and number of the removed myomas were 75.5 g (range, 8 to 218 g) and 1 (range, 1 to 5), respectively. All hybrid laparoscopic myomectomy procedures were completed successfully without conversion to the standard laparoscopic approach. No intraoperative complications occurred. The median operative time was 75 minutes (range, 30 to 100 minutes).
Discussion
Isobaric laparoscopic myomectomy for the removal of large myomas is feasible and safe [11]. Moreover, isobaric laparoscopic suturing with a conventional laparotomy needle holder with a conventional curved needle is easy and quick to perform [511]. Isobaric two-port laparoscopic myomectomy [5] still leaves visible scars at the suprapubic incision site. Therefore, LESS myomectomy may offer better cosmetic satisfaction than isobaric two-port laparoscopic myomectomy. In contrast, LESS myomectomy can result in operative difficulty when attempted in large myoma measuring >8 cm [2].
In this study of hybrid laparoscopic myomectomy, the median operative time and hemoglobin change were 75 minutes (range, 30 to 100 minutes) and 0.9 g/dL (range, 0.0 to 2.4 g/dL), respectively. In recent studies on LESS myomectomy, the mean reported operating times and hemoglobin change were 81 to 100 minutes and 1.1 to 1.5 g/dL, respectively [1212]. As was expected, the median operative time was shorter and the hemoglobin change was less in comparison with previous reports on LESS myomectomy [1212]. Previous studies have shown that multiple myomectomies (more than 3) through LESS myomectomy with a pneumoperitoneum were rarely performed [1212]. Therefore, large intramural (larger than 8 cm) or multiple (more than 3) myomas are usually removed by means of open myomectomy. However, hybrid laparoscopic myomectomy allows the removal of very large myomas (10 cm) and multiple myomas (n=5) with satisfactory results. In this study, we were not limited by the size, number, location, and type of myoma in patients, and we did not use specialized instruments. Nevertheless, 14 hybrid laparoscopic myomectomies were completed without requiring conversion to laparotomy and without increased complication rates.
Our results show that hybrid laparoscopic myomectomy could enable a shorter operative time owing to its convenient suturing, and better anatomical reconstruction of uterine defects than that of LESS, with the similar strength and accuracy as laparotomy. In addition, the advantages of hybrid laparoscopic myomectomy are its better cosmetic outcome because LESS needs no additional incision except for a small umbilical incision that can be concealed (Fig. 1F). However, the clinical limitations of this study include the limited number of patients and its noncomparative design.
In conclusion, hybrid laparoscopic myomectomy can be a feasible, minimally invasive alternative to either LESS or abdominal myomectomy in the surgical treatment of patients with symptomatic intramural and subserosal myomas. Further prospective controlled studies are necessary to determine its clinical application.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.