Delayed hemorrhage effect of local anesthesia with epinephrine in the loop electrosurgical excisional procedure
Article information
Abstract
Objective
The aim of this study was to investigate factors preventing delayed hemorrhage after the loop electrosurgical excisional procedure (LEEP).
Methods
Medical records of patients who underwent LEEP at one university affiliated hospital from October 2013 to January 2015 were reviewed. Patients with or without delayed hemorrhage were classified. LEEP was performed either in an operating room under general anesthesia or in a procedure room with local anesthesia in the outpatient clinic. Delayed hemorrhage was defined as excisional site bleeding occurring between 1 and 30 days after the LEEP requiring intervention such as electro-cauterization, gauze packing, or application of another hemostatic agent.
Results
During the study period, 369 patients underwent LEEP. Twenty-three (6.2%) patients with delayed hemorrhage returned to our hospital either to the outpatient clinic or to the emergency unit. A third of the population (103, 27.9%) underwent LEEP in the operating room under general anesthesia without injection of local anesthesia. The remaining patients (266, 72.1%) underwent LEEP with local anesthesia (lidocaine HCl 2% with epinephrine 1:100,000) in the office procedure room. Patients given local anesthesia including epinephrine had significantly lower delayed hemorrhage compared to patients with general anesthesia without injection of local anesthesia (P=0.001). Hemostats, such as fibrin glue or patch, were used for the majority of patients (346, 93.8%) during the procedure. However, using hemostats was not statistically associated with delayed hemorrhage (P=0.163).
Conclusion
Local anesthesia with the powerful vasoconstrictor epinephrine is effective not only to control perioperative bleeding, but also to prevent delayed hemorrhage after LEEP.
Introduction
The loop electrosurgical excisional procedure (LEEP) is the preferred excisional procedure for higher-grade cervical intraepithelial neoplasia (CIN) and is used to simultaneously diagnose and treat patients [1]. Among conization modalities, there is no superior surgical technique for eradicating CIN and residual disease after the procedure [2]. However, because LEEP produces less hindered pathologic specimens and causes fewer complications, it has become more popular compared to cold knife or laser conization since the 1990s [1]. The most important advantage of LEEP compared to other modalities is that it can be performed in an ambulatory setting [12]. LEEP could ultimately lower the medical cost of treating CINs.
Delayed hemorrhage is the complication of most concern after LEEP not only for the patient but also for the physician, since it results in an unscheduled return to the clinic or sometimes to an emergency room. Of course, additional medical costs and efforts would thus be necessary. Oyesanya et al. [3] reported less intraoperative bleeding resulting from LEEP compared to cold knife conization (3.3±2.8 vs. 79.1±74.6 mL) (P<0.01). Even though immediate procedural bleeding decreases, a number of patients still return to the clinic after LEEP to control delayed excisional site bleeding.
In several studies, general complications after conization have been discussed such as perioperative bleeding, delayed hemorrhage, infection, vaginal discharge, cervical stenosis, and consequent obstetric outcomes [456]. Regarding hemorrhagic complications after cold knife conization, a meta-analysis identified that injection of vasopressin or using tranexamic acid may decrease perioperative bleeding [7]. However, there is limited data demonstrating delayed hemorrhage after LEEP. Thus, in this study, we attempted to investigate factors preventing delayed hemorrhage after LEEP.
Materials and methods
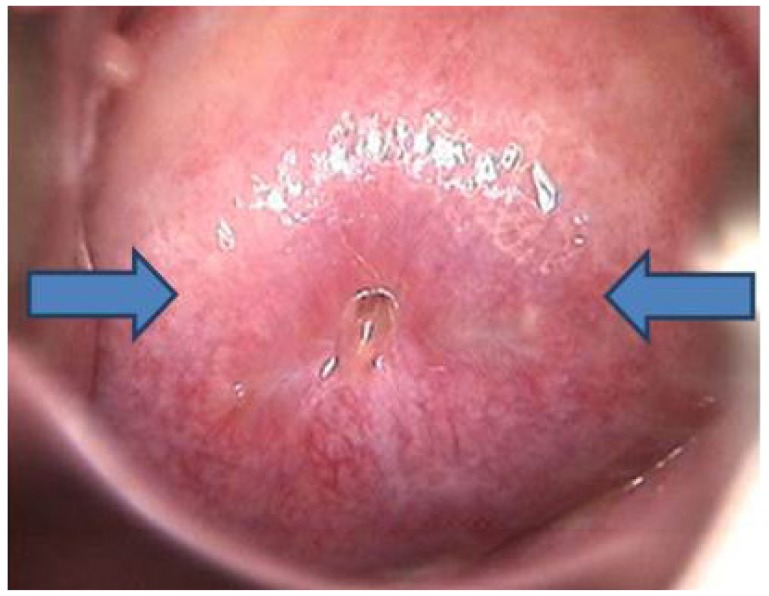
This is a retrospective cohort study of a population of patients diagnosed with CIN who underwent LEEP at the Severance Hospital, Yonsei University, from October 2013 to January 2015. LEEP was performed by five different gynecologic oncologists. The procedure sometimes was performed in an operation room under general anesthesia for various reasons such as the extent of cervical lesions, difficulty in exposure of the cervix in an ambulatory setting, patient preference, and so on. For procedures performed in the operating room, the injection of local anesthesia was omitted, since the patient was under general anesthesia. In the ambulatory setting, LEEPs were performed under local anesthesia in the outpatient clinic procedure room (Fig. 1). Ball tip electrocauterization was routinely performed to prevent both bleeding and to destroy any possible residual lesions. Suturing hemostasis has not been done in order to avoid any long-term complications, especially cervical stenosis, in any of the patients. Different hemostats were used depending on the amount of perioperative hemorrhage. Irrespective of whether the procedure was performed in the operation room or in outpatient procedure room, all patients were discharged after recovering from pain and being checked for post-operative hemorrhage. All patients were prescribed antibiotics after the procedure to prevent excisional site infection.
Age, parity, medical history related to hemorrhagic tendency of the patients, and indications for conization were collected from the medical records. Hemostats used and final pathologic diagnoses were also reviewed. Delayed hemorrhage was defined as hemorrhage which occurred between 1 and 30 days after the LEEP and required interventions such as electrocauterization, gauze packing, or application of another hemostatic agent. Multivariate analysis was performed with variables that considered significant in univariate analysis. A P-value of <0.05 was considered statistically significant.
Results
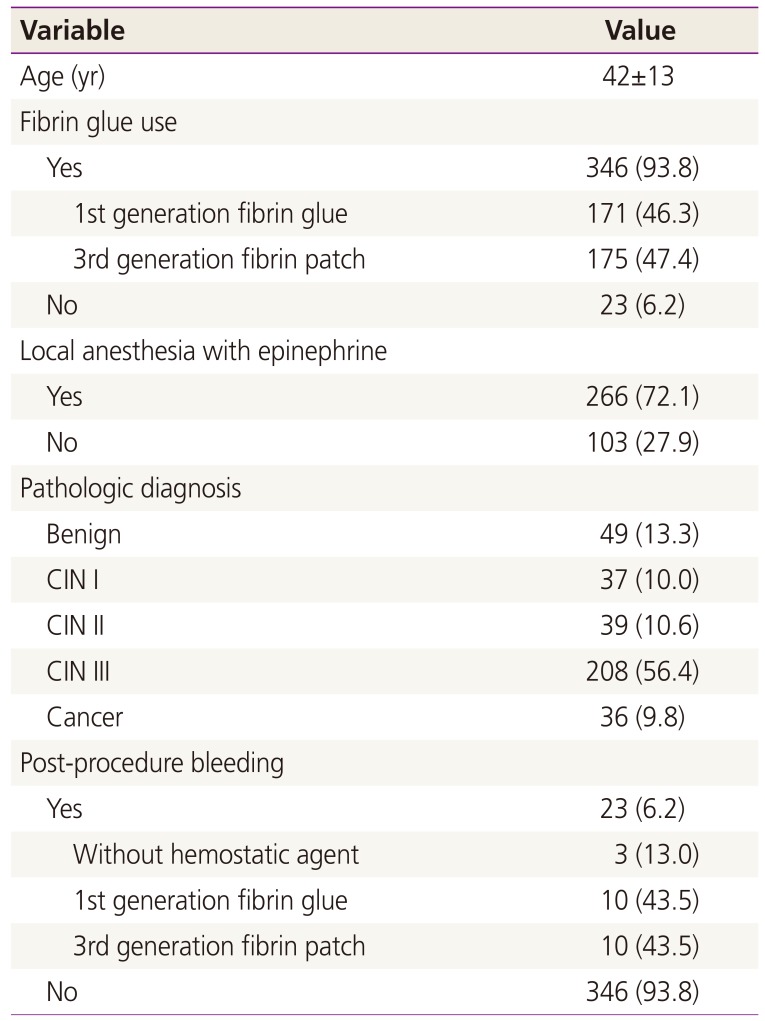
A total of 369 patients underwent LEEP during the study period. Overall 23 (6.2%) patients returned to the clinic or the emergency room because of delayed hemorrhage. The clinicopathological characteristics of the patients included in this study are listed in Table 1. A third of the population (103, 27.9%) underwent LEEP in the operation room under general anesthesia without injection of local anesthesia, the remaining patients (266, 72.1%) underwent LEEP with local anesthesia (lidocaine HCl 2% with epinephrine 1:100,000) in the office procedure room. Among the delayed hemorrhage patients, 13 patients underwent LEEP in the operation room, and 10 patients underwent LEEP in the office. Hemostats, such as fibrin glue or patch, were used for the majority of patients (346, 93.8%) for the procedure. Patients treated with the first generation fibrin glue were 171, while 175 patients were treated with the third generation fibrin sealant. The number of patients with delayed hemorrhage in each hemostatic group or without hemostat were as follows: 3 (13%) for the no hemostatic agent group; 10 (5.8%) for the first generation fibrin glue group; and 10 (5.8%) patients treated with the third generation fibrin sealant group.
Univariate and multivariate analyses of delayed hemorrhage in all patients are shown in Table 2. The multivariated analysis of delayed hemorrhage identified an injection of local anesthesia including epinephrine resulted in significantly lower delayed hemorrhage compared to LEEP without local anesthesia injection (P=0.02). However, using hemostats, regardless of types, did not have statistically significant effect on delayed hemorrhage but may be considered as a tendency toward significance. (P=0.061). Furthermore, age and the pathologic diagnosis did not differ significantly between the groups (P=0.256 and 0.228, respectively).
Discussion
From this study, epinephrine, a powerful vasoconstrictor, combined with local anesthesia reduced the incidence of delayed hemorrhage after LEEP. Vasoconstrictors such as vasopressin have been known to lower perioperative hemorrhage from knife cone biopsy. The major complication of the procedure is postoperative bleeding for which 5% to 20% of patients will require secondary procedures. A variety of technics and instruments have been introduced to reduce operative blood loss and prevent hemorrhage. One method is to inject vasopressin into the cervix before conization. In this study, vasopressin was injected circumferentially using a 18- to 20-gauge needle into the cervical stroma. The use of vasopressin before conization reduces the average blood loss by 100 mL [7]. However, there have been few studies examining factors that lower hemorrhage after LEEP. Furthermore, there are almost no reports describing the use of vasoconstrictors to prevent hemorrhage after LEEP.
Thanks to effective screening tools and the natural progression of uterine cervical cancer that although it is the second most common gynecologic cancer in the world, it is diagnosed at a relatively early stage [8]. However, progressive intraepithelial dysplasia occurring within the transformation zone of the cervix will result in invasive cervical squamous cell carcinoma in the absence of any intervention [9]. After Richart [10] defined the cervical intraepithelial dysplastic lesion as CIN, it has since been graded into three classes and managed according to its pathological classification. However, due to the subjectivity and poor reproducibility of the pathologic diagnosis of CIN, the two tiered-low and high-system was defined in 2012 [11]. Regardless of the classifying systems, higher-grade lesions are considered highly premalignant. Thus, excisional therapy for a highly squamous intraepithelial lesion is the treatment of choice to prevent its malignant progression.
LEEP is the most popular excisional therapy for cervical dysplasia [1]. Excisional therapy of the cervical transformation zone, so called cone biopsy or conization, can be performed using a scalpel, laser, or by electosurgery. Knife conization was generally performed before the introduction of colposcopy [2]. However, knife conization almost always required general anesthesia and was accompanied by various morbidities including perioperative or delayed hemorrhage, perioperative severe pain, cervical stenosis at follow-up, vaginal discharge, performing site infection, and consequent adverse pregnancy outcomes [5]. Laser conization is usually performed under general anesthesia and produces more artifacts at the excisional margin than other excisional procedures. LEEP has been popular since the 1990s, because it could be easily completed with successful treatment outcome and less complications [121314]. The procedure can be performed under local anesthesia in an office setting.
Delayed hemorrhage, defined as procedure site bleeding occurring several days after the operation, might be considered the most troubling complication of LEEP for physicians in outpatient settings. Delayed hemorrhage after LEEP, which usually requires medical assistance, requires both the patient and physician to invest more time and effort for its management. Thus, even if incidence of delayed hemorrhage after LEEP is relatively lower than that of other conization modalities [14], preventing delayed hemorrhage during the procedure would help not only physicians during practice, but also patients to improve their recovery. Therefore, we considered that investigating factors preventing delayed hemorrhage after LEEP would provide practical information to physicians in their practice.
To prevent perioperative hemorrhage or delayed hemorrhage, hemostasis must occur. This can be facilitated by applying hemostatic agents. In our institution, hemostatic agents, such as Beriplast (fibrin sealant containing fibrinogen, factor XIII, and thrombin), TachoComb (aprotinin, collagen, fibrinogen, and thrombin), or TachoSil (collagen, fibrinogen, and thrombin) were applied to the majority patients on the LEEP region during the procedure and used prophylactically against delayed hemorrhage. The prophylactic application of hemostatic agent to the cervical wound after LEEP did not significantly reduce delayed hemorrhage compared with not using hemostats.
Our findings also provide useful information for the gynecologic oncologist who often treats microinvasive cervical cancer with LEEP. Local anesthesia could be overlooked and omitted in an operation room using general anesthesia, because the patient would not complain of pain perioperatively and LEEP, itself, could prevent perioperative hemorrhage. However, according to our findings, local anesthesia with epinephrine could reduce not only perioperative hemorrhage or pain, but also the most concerning long-term complication: delayed hemorrhage.
A limitation of this article is the retrospective nature of the study which precludes the possibility to adjusted parameters such as extent of excision, degree of cauterization for controlling bleeding during the procedure, inflammation status, and others.
In conclusion, local anesthesia with the addition of a powerful vasoconstrictor, epinephrine, is effective not only to control perioperative bleeding, but also to prevent delayed hemorrhage after LEEP.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2014R1A1A1A05002926).
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.