Frequency of third trimester umbilical artery Doppler for improving neonatal outcomes in high-risk pregnancies: a randomized trial
Article information
Abstract
Objective
Umbilical artery Doppler ultrasonography is useful for high-risk prenatal surveillance. However, according to a systematic review and meta-analysis by the Cochrane pregnancy and childbirth group, the optimal frequency with which such surveillance should occur remains unclear. In the current study, we aimed to investigate whether performing umbilical artery Doppler on a weekly basis enables earlier detection of changes in utero-placental blood flow than the recommended bi-weekly (i.e., fortnightly) regimen and its impact on perinatal outcomes.
Methods
This randomized controlled study included 292 high-risk pregnant women in their third trimester who attended the Ain Shams University Maternity Hospital in Egypt from January 2018 to September 2019. The women were randomly assigned to two groups to undergo either bi-weekly or once-weekly umbilical artery Doppler ultrasound.
Results
In the primary analysis performed according to the intention-to-treat basis, we observed no difference in the primary outcome of fetal admission to the neonatal intensive care unit (NICU) within the first 24 hours (risk difference, −2.63; 95% confidence interval, −12.92 to 7.65). Furthermore, no significant differences in secondary outcomes were observed (apart from stillbirth).
Conclusion
Weekly umbilical artery Doppler is not superior to bi-weekly surveillance in preventing admission to the NICU and most other studied outcomes. Therefore, the bi-weekly regiment may be more convenient for women and more cost-effective for health care organizations (trial registration: NCT03584763 at clinicaltrials.gov).
Introduction
Pregnant women tend to be divided into low- and high-risk populations; however, the proportion of pregnancies classified as high-risk continues to increase significantly [1].
The placenta detects and responds to changes in the maternal environment by altering its structure and function, which can lead to changes in blood flow and fetal growth [2]. In a healthy fetus, the umbilical artery Doppler pulsatility index (PI) decreases with advancing gestation. This reflects a decrease in the placental vascular resistance. In fetuses with intrauterine growth restriction (IUGR), there is an increase in PI secondary to the decrease, absence, or reversal of end-diastolic flow. These changes in the waveforms are indicative of increased placental resistance. Hence, umbilical artery Doppler ultrasound is a useful prenatal test that can help to ensure fetal well-being and timely intervention [3].
Hypoxic cerebral damage may begin before labor, and intrapartum asphyxia is likely more damaging when super-imposed on such underlying hypoxia [4]. Abnormal Doppler results suggestive of hypoxia can aid obstetricians in making decisions that minimize the risk of intrauterine fetal death (IUFD). Despite its generally recognized value, a systematic review and meta-analysis by the Cochrane pregnancy and childbirth group indicates that the optimal frequency with which umbilical artery Doppler surveillance should be performed remains unclear [5].
In the current study, we aimed to investigate whether performing umbilical artery Doppler on a weekly basis enables earlier detection of changes in utero-placental blood flow than the recommended bi-weekly (fortnightly) regimen and its impact on perinatal outcomes.
Materials and methods
1. Study design
This randomized controlled study included women with high-risk pregnancies in their third trimester. Specifically, we aimed to determine the optimal frequency of umbilical artery Doppler for women at high risk of developing IUGR using a balanced randomization scheme and parallel-group design. The study was conducted in the special care unit of the Ain Shams University Maternity Hospital, Cairo, Egypt, from January 2018 to September 2019 (NCT03584763).
2. Recruitment
Eligible participants were all women with high-risk singleton pregnancies in their third trimester, including women with a previous obstetric history of preeclampsia or eclampsia, placental abruption, IUGR, or stillbirth and those with preexisting medical disorders (renal, pulmonary, cardiac, or autoimmune diseases). Women with current preeclampsia or pregnancy-induced hypertension were also included. Exclusion criteria were congenital anomalies of the fetus, multiple gestations, unconfirmed gestational age, or withdrawal of consent.
Simple randomization was performed using a computer-generated random number list prepared by the study supervisor, with no clinical involvement in the trial. The study investigator enrolled patients and assigned them to either group according to random allocation.
The randomized allocation was kept in opaque sealed envelopes, with enrollment numbers written in the envelopes. The envelope contained a card written by the designated study group. After completion of patient enrollment, the envelope marked with the study number was unsealed, and the patients were allocated to either group.
3. Intervention
A total of 292 women with high-risk pregnancies who fulfilled the inclusion criteria were randomly divided into two groups, with 146 patients in each group. Group I underwent Doppler bi-weekly, and group II underwent Doppler once weekly. Umbilical artery Doppler ultrasound was performed by an expert sonographer using a 3.5 MHz transabdominal probe connected to an ultrasound machine. All patients were placed in a semi-recumbent position with left lateral tilt. An area of the amniotic cavity with several loops of cord was selected. Then, using pulsed wave Doppler on a free loop of cord, the characteristic sound and shape of the umbilical artery were identified, and the resistance index was estimated by taking the average of three separate readings. Fetal weight was estimated using the commonly used Hadlock formula (using biparietal diameter, abdominal circumference, and femur length) [6]. The estimated fetal weight was plotted against standard fetal growth curves. An estimated fetal weight of <10th percentile was used to diagnose a small for gestational age (SGA) fetus.
4. Study outcomes
The primary outcome of this study was admission to the NICU for at least 24 hours. The secondary outcomes included fetal and maternal outcomes. Fetal outcomes included still-birth, neonatal death, fetal acidosis, Apgar score less than 7, preterm labor less than 37 weeks, neonatal resuscitation, respiratory distress syndrome (RDS), hypoxic ischemic encephalopathy (HIE), intraventricular hemorrhage (IVH), bronchopulmonary dysplasia (BPD), birth weight, gestational age at birth, and length of NICU stay. Maternal outcomes included cesarean section (CS), labor induction, and oxytocin augmentation.
5. Sample size calculation
The sample size in this study was calculated to be 292 patients. This was based on the results of a Cochrane review for fetal and umbilical Doppler ultrasound in high-risk pregnancies, which reported an ICU admission rate of 12% [7]. The above-mentioned sample size was then obtained based on a proportion p1 (target rate of ICU admission) of 0.03 and a proportion p2 (rate of ICU admission in Cochrane review) of 0.12, with an α error probability of 0.05 and power of 0.8. One hundred forty-six patients were allocated to each group, yielding an actual power of 0.8 and an actual α of 0.039.
6. Statistical analysis
We explored the data and reported the descriptive statistics using summary measures for continuous and dichotomous variables. The primary analysis included the intention-to-treat population, in which NICU admission and secondary outcomes were compared between the groups based on risk ratios (reported as risk difference) and 95% confidence intervals (CIs). We also conducted subgroup analyses for the following: mode of delivery (vaginal vs. CS), gestational age at birth (<34 weeks, 34–37 weeks, and >37 weeks), birth weight (<2,500 g vs. >2,500 g). A sensitivity analysis was conducted, including the per-protocol population, excluding patients with major protocol violations. All statistical tests were two-tailed. Statistical significance was set at P<0.05. We used SAS University Edition (SAS Institute Inc., Cary, NC, USA) to analyze the data. We followed the standards for reporting statistical analyses using the SAMPL Guidelines.
Results
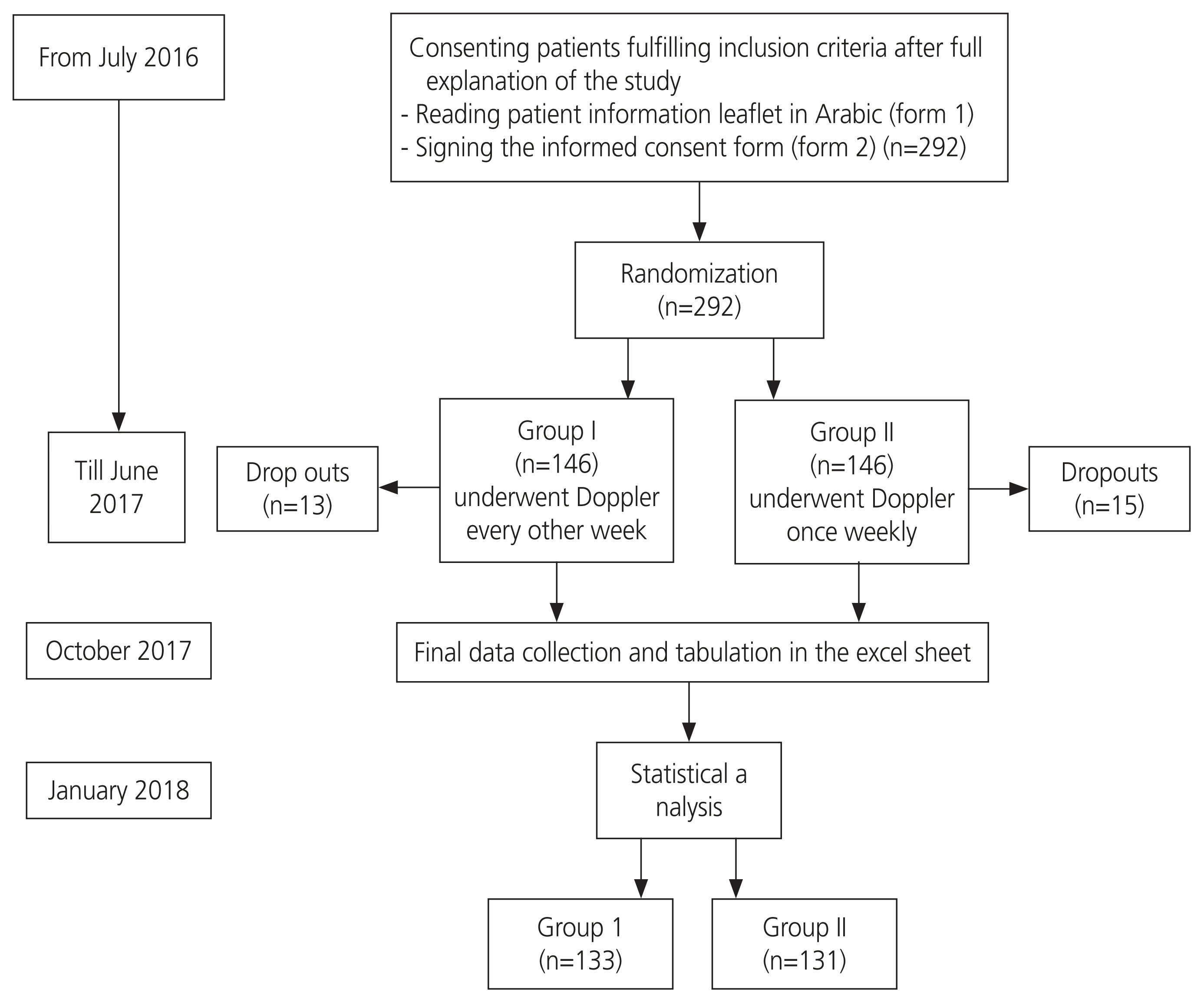
The participant timeline is shown in Fig. 1. The study was conducted in the third trimester, from 28 weeks of gestation until the time of delivery, with a maximum period of 13 weeks.
The baseline characteristics of the study group population are shown in Table 1, which includes data for maternal age, gestational age at enrollment, parity, and prior CS. There were no statistically significant between-group differences in demographic characteristics, including mean age in years, gestational age at enrollment in weeks, parity, and prior CS.
Risk factors in the study group were diabetes mellitus, chronic hypertension, renal disease, autoimmune diseases such as systemic lupus erythematosus and antiphospholipid antibody syndrome, and chronic hypoxemia, including asthma and preeclampsia. The number and percentage of these risk factors among the two groups are shown in Table 1.
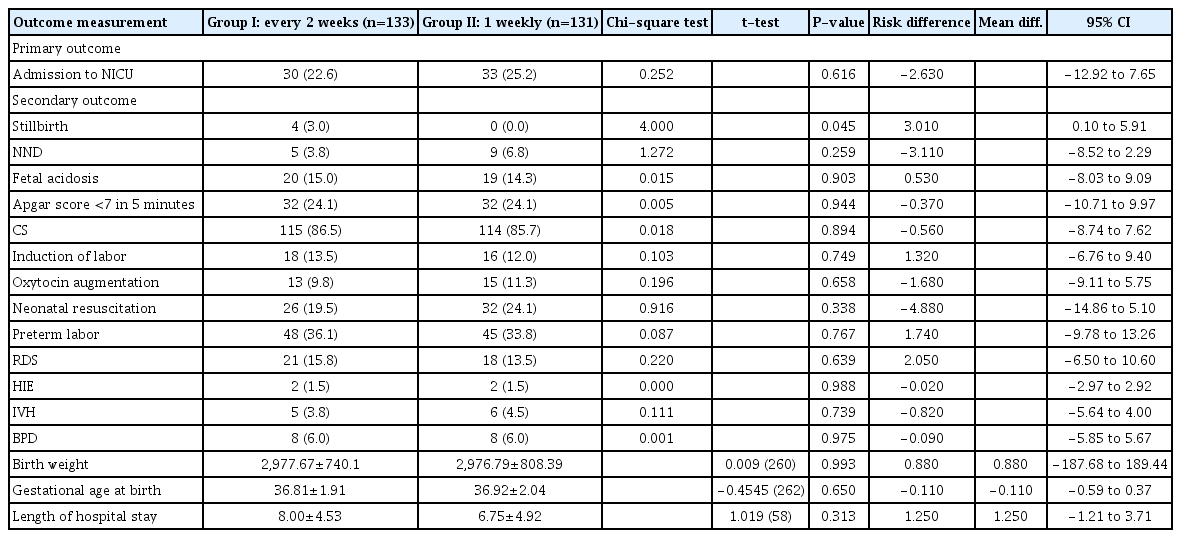
Comparisons between the groups according to the primary and secondary outcomes are shown in Table 2. There were 30 babies (22.6%) from group I and 33 babies (25.2%) from group II admitted to NICU, with a risk difference of −2.630 and 95% CI of −12.92 to 7.65. No significant differences were observed between the groups.
There were also no statistically significant differences in secondary outcomes between the groups, except for still-birth. There were four cases of stillbirth in group I and none in group II (risk difference, 3; 95% CI, 0.1 to 5.9). In three of these stillbirth cases, the women were originally recruited based on mild preeclampsia with no IUGR, did not follow their routine prenatal care, and developed severe preeclampsia and stillbirth within 2 weeks, at which time they presented. The fourth patient had uncontrolled gestational diabetes mellitus and was admitted to the hospital with sudden IUFD 2 weeks after the initial presentation.
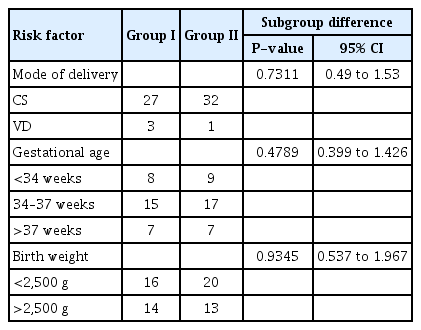
The results of the subgroup analysis for mode of delivery (vaginal vs. CS), gestational age at birth (<34 weeks, 34–37 weeks, and >37 weeks), and birth weight (<2,500 g vs. >2,500 g) are shown in Table 3. Neither the route of delivery nor the gestational age at delivery or infant weight at birth were confounders or effect modifiers for the primary outcome (NICU admission within the first 24 hours).
Discussion
At present, it is recommended that high-risk pregnancies, considered to be at risk of placental insufficiency, should be monitored with Doppler studies of the umbilical artery. Doppler assessment of placental circulation plays an important role in screening for impaired placentation and complications of IUGR [8]. The purpose of umbilical artery Doppler surveillance is to predict fetal acidemia, thereby allowing timely delivery prior to irreversible end-organ damage and IUFD [9].
According to a systematic review, Doppler velocimetry of umbilical and fetal arteries in high-risk pregnancies, when followed by the appropriate intervention, can reduce rates of perinatal mortality and stillbirth by 29% and 35%, respectively, despite a lack of statistical significance in this difference [4]. Another review article stated that Doppler ultrasonography of the umbilical artery in high-risk pregnancies significantly reduced the induction of labor and CS delivery for fetal distress. Moreover, the Doppler-guided actions lowered the probability of perinatal death by 38%. Post hoc analyses revealed a statistically significant decrease in intrapartum fetal distress and hypoxic encephalopathy [10].
In this randomized controlled study of 292 women, we aimed to determine whether weekly Doppler ultrasonography yields better pregnancy outcomes than a bi-weekly regimen for high-risk pregnancies. Our results indicated that the mean gestational age at birth was 36.81 (1.91%) in group I and 36.92 (2.04%) in group II, with a mean difference of −0.1 and 95% CI of −0.59 to 0.37. This difference translates to only 1 day earlier in group I, which is not a statistically significant difference. There were also no significant differences in mean birth weight between groups I and II (2,977 g vs. 2,976 g).
A pilot randomized trial conducted by McCowan and colleagues [11] at a tertiary center in New Zealand between 1993 and 1997 compared twice weekly with fortnightly Doppler ultrasonography in 167 pregnant women with SGA fetuses. The authors found no statistically significant difference in neonatal morbidity, which is consistent with our results. There were also no perinatal deaths in either of the study groups. This may be attributed to the types of participants in their study, which only recruited a subset of pregnancies with normal Doppler studies but excluded pregnancies with abnormal Doppler studies and oligohydramnios. The mean birth weights in their study were 2,534 in group I and 2,587 in group II, which were lower than those observed in our study. This is because the previous trial recruited pregnant women with ultrasonographic evidence of SGA fetuses (i.e., abdominal circumference <10th percentile). The mean gestational age at birth in the McCowan et al. [11] study was 264 days in the 2-weekly group and 268 days in the fortnightly group. Women in the twice-weekly surveillance group gave birth on average 4 days earlier than women in the fortnightly surveillance group. They could not conclude that fortnightly surveillance was safe because many of the women assigned to this regimen underwent additional tests of fetal well-being and their clinicians were not always comfortable with the planned reduced frequency of fetal surveillance [11].
It should be noted that there was a high rate of CS in our study, which was attributed to the patients being a high-risk population with potential fetal compromise. However, this is not the case for the normal population.
Among the limitations of our study is that it was primarily powered to detect a difference in the primary outcome (admission to the NICU for more than 24 hours) while being underpowered to detect differences in secondary outcomes. Hence, separate studies should be designed with adequate power for detecting potential differences in fetal and maternal outcomes between the two surveillance regimens.
In conclusion, our study demonstrated no difference in the primary outcome of admission to the NICU for more than 24 hours between once weekly and bi-weekly umbilical artery Doppler surveillance. Additionally, there were no significant differences in secondary outcomes, including maternal outcomes such as CS, induction or augmentation of labor, and fetal outcomes such as fetal acidosis, RDS, HIE, IVH, BPD, low Apgar score, neonatal resuscitation, and preterm labor. The notable exception was still birth, rates of which significantly differed between the two groups. Based on these findings, weekly umbilical artery Doppler is not superior to bi-weekly surveillance in preventing admission to the NICU and most other studied outcomes. Therefore, the bi-weekly regimen may be more convenient for women and more cost-effective for health care organizations.
Acknowledgements
Not applicable.
Notes
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study was approved by the Faculty of Medicine Research Ethics Committee (FWA 000017585; approval number: FMA-SU MS, 34).
Patient consent
All participants signed an informed consent form and were provided with a patient information leaflet about the study.
Authors’ contribution
The first author designed the study methodology and reviewed the results. The second author recruited the patients, followed them through pregnancy and delivery, and helped with the data collection and manuscript preparation. The third author reviewed the results and prepared the manuscript.
Funding information
This research was not funded by any organization.
Availability of data and materials
The data used to support our findings are available from the corresponding author if requested.