|
 |
- Search
| Obstet Gynecol Sci > Volume 66(6); 2023 > Article |
|
Abstract
Objective
We aimed to determine whether ovarian-preserving surgery for adnexal torsion helps preserve ovarian function without increasing the risk of postoperative complications.
Methods
We retrospectively evaluated 71 women who were surgically diagnosed with adnexal torsion between January 2015 and December 2019 at Severance Hospital, Yonsei University College of Medicine (ovarian preservation group, 56; oophorectomy, 15). Serum anti-Müllerian hormone (AMH) levels measured within 6 months before surgery were compared to levels measured 6-24 months after surgery. Surgical findings and postoperative complications were compared between the groups.
Results
There was a borderline significant difference in the decrease in serum AMH levels between the oophorectomy group and ovarian preservation group before and after surgery. There were no significant differences between the groups in terms of fever, infection, or duration of admission. Discoloration of the twisted ovary was found in 27.3% and 33.3% of the patients in the ovarian preservation and oophorectomy groups, respectively. There was no difference in the decrease in serum AMH levels between patients with and those without discoloration.
Conclusion
Ovarian-preserving surgery may not increase postoperative complications in patients with adnexal torsion, even if a twisted mass is suspected to be necrotic. Moreover, the ovarian reserve may not be affected by torsion if the ovary is preserved. Conservative ovarian surgery can be safely performed to preserve the reproductive potential of women with adnexal torsion and cystic masses.
Adnexal torsion is a state in which the adnexa and ovaries are twisted at least once in the infundibulopelvic and tubo-ovarian ligaments. Adnexal torsion can also occur in normal ovaries, benign masses, and malignant neoplasms [1-3]. The clinical presentation of adnexal torsion is nonspecific, and it is diagnosed surgically [4]. The incidence of adnexal torsion is 2-15% in women who undergo surgical treatment for adnexal masses; however, the incidence rate is likely underestimated, as it is not diagnosed if it is not surgically observed [5]. Adnexal torsion can occur at any age; however, it occurs most frequently in women of reproductive age, and its incidence rate is lower in premenarchal girls and postmenopausal women [6,7].
The blood supply to the ovary decreases during adnexal torsion occurrence, leading to ovarian ischemia. Without immediate treatment, it can progress to ovarian necrosis, which reduces ovarian function and fertility damage [8]. Therefore, if a patient visiting the hospital for acute abdominal pain is suspected of having adnexal torsion, the patient is treated with emergency surgery [9]. Oophorectomy was considered the standard treatment in the past, with the opinion that there was a risk of a thromboembolic event in the presence of adnexal torsion or that a necrotic ovary could cause peritonitis or intraperitoneal infections [7,10-17]. In particular, in the case of adnexal torsion, because the ovary is enlarged and discolored, clinicians often perform oophorectomy because of concerns about malignant neoplasm [18-20].
Several studies have recommended ovarian-preserving surgery. According to a recent study, even if the color change in the ovary resembles that of a necrotic ovary, there are few perioperative complications when conservative surgeries are performed [7,21]. Studies have also shown that the macroscopic appearance of ovaries does not reflect the degree of ovarian ischemia [7,14,21,22]. A recent large-scale study found that the incidence of malignancy in adults with adnexal torsion was 2.0%. Benign ovarian mass were 12.9 times (P<0.001) more likely to occur than malignant ovarian neoplasms [23]. In particular, in reproductive-aged women, oophorectomy can lead to infertility due to decreased ovarian function; therefore, conservative surgery should be considered [24]. However, many clinicians hesitate to preserve the ovary when they encounter a discolored ovary in the operation field, fearing possible complications.
This study aimed to analyze the changes in anti-Müllerian hormone (AMH) levels and any potential postoperative complications after ovarian preserving surgery in cases with adnexal torsion in premenopausal women. We ought to prove that conservative surgery helps to preserve ovarian function, even in cases where there is an ovarian color change on intraoperative findings.
The Institutional Review Board of Severance Hospital, Yonsei University College of Medicine approved this study (approval no. 4-2021-0049). The requirement for informed consent was waived due to the retrospective nature of the study. This retrospective study included women who were surgically diagnosed with adnexal torsion between January 2015 and December 2020 at Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. Women with no surgical findings of adnexal torsion were excluded. Patients with bilateral ovarian cysts who had undergone bilateral ovarian cystectomy were excluded from the study. Since bilateral ovarian cystectomy can affect the function of both ovaries, it is challenging to assess ovarian function after preservation surgery. Patients without AMH data before or after surgery were excluded. Menopausal patients were excluded from the study. A total of 71 patients were included in this study: 56 in the ovarian preservation group and 15 in the oophorectomy group. The following data were collected: age; height; body weight; duration of abdominal pain; interval time between symptoms and surgery; size and laterality of the adnexal mass on preoperative ultrasonography; and preoperative laboratory values, including hemoglobin, white blood cell, platelet, and AMH levels. Serum AMH levels were determined within 6 months before surgery and at 6-24 months after surgery. Data on the duration of admission, postoperative complications, and postoperative fever were also included. Postoperative fever was defined as a body temperature ≥37.8°C. Experienced obstetrics and gynecology physicians performed sonography using an ACCUVIX-XQ (Samsung Medison, Seoul, Korea) or Voluson E8 (GE Healthcare, Zipf, Austria). The maximum diameter of the adnexal mass was measured in centimeters by measuring the largest diameter and the diameter perpendicular to it; laterality was also measured. Each surgery was performed by an experienced gynecologist with expertise in minimally invasive surgery, making it a total of six surgeons. The laterality, size, twisting direction, degree, and presence of ovarian discoloration as well as whether oophoropexy was performed were determined. In addition, the operation types and pathologies of the ovarian masses were also included.
Patients with serum AMH values both before and after surgery were extracted from the ovarian preservation and oophorectomy groups; 19 patients were included in the ovarian preservation group and four in the oophorectomy group. For these patients, characteristics by age group, AMH values before and after surgery, and AMH changes were compared and analyzed. In addition, a partial correlation analysis was conducted by controlling for other factors to identify those affecting changes in serum AMH levels.
Continuous data are expressed as mean±standard deviation, and categorical data are expressed as numbers of cases (percentages). Student’s t-test or Mann-Whitney U-test was used to compare continuous variables. The chi-squared test was used to compare categorical variables between the ovarian preservation and oophorectomy groups. The paired t-test or Wilcoxon signed-rank test was used based on normality to compare pre-and postoperative serum AMH levels. All statistical analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA). A P-value <0.05 was considered to indicate statistical significance.
Cases of adnexal torsion in premenopausal women who underwent surgery were divided into ovarian preservation and oophorectomy. The baseline characteristics of the patients are shown in Table 1. Comparing the oophorectomy and ovarian preservation groups, the average age of the oophorectomy group was approximately 8 years. The average body mass index (BMI) was 25.69 in the oophorectomy group and 22.30 in the ovarian preservation group. In the two groups, lower abdominal pain was the most common symptom, and there was no significant difference in its severity. When expressed using the visual analog scale (VAS), the average pain rating was 2.35 in the ovarian conservation group and 3.16 in the oophorectomy group.
Regarding postoperative complications, only one patient in the group that underwent ovarian preservation surgery experienced complications, resulting in a complication rate of 1.8%. The patient had a postoperative wound infection in the umbilicus, the laparoscopic insertion site; however, the patient recovered with oral antibiotics and conservative management. No postoperative complications were observed in the oophorectomy group. Postoperative fever was confirmed in 21.0% of patients in the ovarian preservation group, and none of the patients had a postoperative fever in the oophorectomy group. However, all 12 patients with postoperative fever in the ovarian preservation group were discharged from the hospital without signs of pneumonia, intraperitoneal infections, or surgical site infections. The average number of days was confirmed as 2.60 and 3.13 in the ovarian preservation and oophorectomy groups, respectively. Regarding postoperative complications, there were no significant differences between the two groups in terms of fever (P=0.15), infection (P=0.6), or duration of admission (P=0.57).
Preoperative and postoperative AMH levels were compared between the two groups. The mean preoperative AMH level was 3.59±3.76 in the ovarian preservation group, which was higher than the value of 2.44±2.94 in the group that underwent oophorectomy. The mean postoperative AMH level was 2.98±1.87 in the ovarian preservation group and 1.78±2.08 in the oophorectomy group. In Table 2, only patients with serum AMH levels both before and after surgery were extracted, and the amount of serum AMH change was compared between the ovarian preservation and oophorectomy groups. There were 19 patients in the ovarian preservation group and four in the oophorectomy group. There was a significant difference in the decrease in serum AMH levels before and after surgery between the two groups, with a greater reduction observed in the oophorectomy group (P=0.004). There was no significant difference in the characteristics of the ovarian preservation group with those of the oophorectomy group, which had serum AMH values both before and after surgery.
Age is a crucial factor in analyzing changes in serum AMH; therefore, the serum AMH values of ovary preserved group in Table 2 (n=19) were analyzed by age group (age <20 [n=8], 20≤ age <30 [n=4], age ≥30 [n=7]). The mean preoperative AMH of age under 20 group was 2.71±0.79 and the mean postoperative AMH was 3.67±1.86. In the case of 20≤ age <30 group, mean preoperative AMH was 6.41±4.41, and mean postoperative AMH was 7.45±3.11. In the case of age over 30, mean preoperative AMH was 2.15±1.50, and mean postoperative AMH was 2.31±1.56. The mean values of preoperative AMH and postoperative AMH were significantly higher in the group aged 20-30 (preoperative AMH, P=0.017; postoperative AMH, P=0.04). However, the change in serum AMH levels was positive in all age groups, and there was no statistically significant difference (P=0.374).
Partial correlation analysis was performed by controlling for factors that may affect AMH levels before and after surgery (Fig. 1). After controlling for age, BMI, preoperative AMH, size of the twisted ovary, and time interval between symptoms and surgery, no significant association was noted between AMH changes and the size of the rotated ovary (r=−0.087, P=0.810) and time interval between symptoms and surgery (r=0.099, P=0.785).
Table 3 compares the two groups diagnosed with adnexal torsion based on the intraoperative and histological findings. There were no significant differences in the two groups in twisted sides or twist angles of the ovary. The incidence of adnexal torsion was high in the right adnexa in both the groups (60.7% and 66.7% in the ovarian preservation and oophorectomy groups, respectively). In addition, there was no difference in the average twisted angle (720 degree) between the groups. However, the ratio of adnexal torsion in the clockwise direction was higher in the oophorectomy group, while that in the clockwise direction in the ovarian preservation group was 56.3%, and that in the clockwise direction in the oophorectomy group was 66.7%. When comparing histological findings, mature cystic teratomas were the most common in the ovarian preservation group (33.9%). Paraovarian and paratubal cysts were observed in 19.6% of the patients. In the oophorectomy group, the proportion of benign cysts with hemorrhagic infarction was as high as 40.0%, and fibromas and serous cystadenofibromas accounted for the second largest proportion (13.3%).
When comparing cases in which an ovarian color change was noted in the intraoperative findings, ovarian discoloration was observed in 27.3% and 33.3% of patients in the ovarian preservation and oophorectomy groups, respectively. The rate of change in the serum AMH levels after surgery was compared between patients with and without ovarian discoloration in the ovarian preservation group (Table 4). In patients with ovaries without discoloration, the postoperative serum AMH levels increased by 0.2%, and in those with discoloration, the postoperative serum AMH levels increased by 40.0%. There was no significant difference in the change in serum AMH levels between the two groups (P=0.248).
Table 5 compares patients who had adnexal masses, including ovarian cysts, paraovarian cysts, or ovarian solid masses, in their actual operative findings to those who underwent detorsion surgery only due to adnexal torsion, even though there was no adnexal mass at all. There was no difference in the degree of abdominal pain reported by the patients when they visited the hospital, with an average of three points on the VAS scale reported by both the group with ovarian mass and the group without ovarian mass. When comparing both groups, the ovary size at adnexal torsion was 8.5 cm in the group with cysts and 5.0 cm without cysts. The twisting angle was 720 degree in the group with an ovarian mass and 540 degree in the group without an ovarian mass.
We compared the characteristics, intraoperative findings, and postoperative complications, surgical pathologies in women diagnosed with adnexal torsion who underwent ovarian preservation surgery and oophorectomy. In addition, the degree of ovarian function change in the oophorectomy and ovarian preservation surgery groups was compared using AMH level analysis. Our study showed that despite preserving the ovaries in adnexal torsion, there were no postoperative side effects such as thromboembolism or peritonitis. No significant difference was noted in the AMH levels before and after surgery in the case of ovarian preservation surgery, despite an ovarian color change due to adnexal torsion. Based on the final postoperative pathology results, solid masses accounted for approximately 20.0% of the cases in the oophorectomy group. Simultaneously, most were cystic masses in the ovarian conservation group and only 1.8% were solid masses. Therefore, this study recommends further ovarian conservation when adnexal torsion is diagnosed in premenopausal women and when the ovarian mass is cystic.
In this study, patients diagnosed with ovarian torsion who underwent surgical treatment were divided into oophorectomy and conservative surgery groups. The ratio of perioperative complications was analyzed, and AMH levels, which are indicative of ovarian function, were analyzed before and after surgery. The mean preoperative AMH level was lower in the oophorectomy group than in the ovarian preservation group because the average age was higher than in the oophorectomy group.
A comparison of patients in the ovarian preservation and oophorectomy groups with serum AMH levels both before and after surgery showed that the preoperative AMH levels were similar between the two groups. Postoperative serum AMH levels decreased on average in the oophorectomy group, while they increased slightly in the ovary-preserved group. In addition, when comparing patients by age in the ovarian preservation group, the postoperative serum AMH levels tended to increase slightly in all age groups. Further research is needed; however, previous studies have shown that the antral follicle count (AFC) of the ovary on the side where adnexal torsion was observed was lower after the conservative surgery compared to before, but AFC recovered to the same level as that in the opposite ovary in the 3 months after surgery. AMH decreased slightly from the preoperative level in the first month after surgery but increased slightly from the preoperative level in the third month after surgery [25]. Therefore, the slight increase in serum AMH levels after conservative surgery in this study showed similarity to that reported in a previous study. However, further research is required to understand the reasons and principles.
Although there were limitations to this study due to the small number of patients included, factors, such as the size of the twisted ovary or the time interval between symptoms and surgery, were not related to serum AMH changes when analyzing factors that could affect serum AMH changes. Therefore, even if time has passed since the onset of symptoms or the size of the ovarian cyst is large, it can be assumed that ovarian function can be preserved through conservative surgery.
Several studies have found it challenging to evaluate the viability of an ovary with a black-bluish appearance because it does not represent the degree of ischemia [7,16,21]. In our study, although discoloration of the ovary was noted in the operating room, there was no reduction in the patient’s AMH level when ovarian preservation surgery was performed. Accordingly, although ovarian necrosis is suspected due to discoloration, ovarian function is preserved when ovarian preservation surgery is performed in reproductive-aged women with adnexal torsion. Complications after ovarian preservation surgery were also compared among the patients; 21.4% of the patients in the ovarian preservation group experienced fever after surgery, and there was no fever in the oophorectomy group. However, even if there was fever after surgery in the ovarian preservation group, the patients were discharged without any specific findings on the third day after surgery. There was no significant difference between the ovarian preservation and oophorectomy groups in terms of admission duration, with an average of 3 days in both groups. In the ovarian preservation group, only one case of postoperative complication was identified. In this case, the skin infection was caused by a surgical wound. There were no symptoms such as abdominal pain or fever other than wound discharge, which improved within a few days without any specific findings after taking oral antibiotics. In addition, radical surgery, including oophorectomy, was often performed because of concerns regarding pulmonary thromboembolism. However, later studies reported that pulmonary thromboembolism after adnexal torsion occurred in only two cases in adults, and both cases were in the oophorectomy group [13]. There were no cases of thromboembolism or intraperitoneal infection in either group. In conclusion, as a result of this study, there were no significant difference between the two groups in postoperative complications.
According to the postoperative biopsy results, benign cysts accompanied by hemorrhagic infarction were most common in the oophorectomy group (40.0%), followed by solid masses such as cystadenofibroma/fibroma and intraligamentary leiomyoma (25.0%). In the ovarian preservation group, 33.9% of the cysts were mature cystic teratomas, 19.6% were paratubal or paraovarian cysts, and 17.9% were detorsion cases without cysts or masses. In particular, only 1.8% of the patients in the ovarian preservation group had solid masses. In conclusion, solid masses accounted for 25.0% of the oophorectomy group, which was a much larger proportion than that in the ovarian preservation group. In cases of adnexal torsion with a solid ovarian mass, oophorectomy is performed because of the high incidence of ovarian necrosis. Therefore, ovarian preservation is recommended in cases of a cystic mass rather than a solid mass when adnexal torsion is observed in premenopausal women. Adnexal torsion occurred more frequently in the right ovary in the preservation and oophorectomy groups. Notably, the right utero-ovarian ligament is physiologically longer than the left, and the sigmoid colon is present on the left side of the body. Therefore, torsion is more likely to occur on the right side.
One limitation of this study is that it was a retrospective study of patients who underwent emergency surgery for the diagnosis of adnexal torsion; therefore, the sample size was small. In particular, because emergency surgery for adnexal torsion was performed, the number of cases in which the AMH levels before and after surgery could be compared was small. In the case of adnexal torsion, it is difficult to conduct a prospective study because of the low incidence rate and emergency characteristics. However, this study is meaningful because, despite its emergence, the degree of preservation of ovarian function was compared numerically by checking AMH levels before and after surgery. In addition, by tracking the presence or absence of postoperative compositions and revealing no significant differences noted between the two groups, it was helpful to determine whether clinicians hesitated to perform ovarian preservation because of the fear of postoperative complications. We plan to study a larger number of patients, including a numerical scale, and encourage conservative treatment to preserve ovarian function.
Despite the above limitations, we conclude that ovarian-preserving surgery may not increase postoperative complications in patients with adnexal torsion, even if a twisted mass is suspected to be necrotic. Moreover, the ovarian reserve may not be affected by torsion if the ovary is preserved. Conservative ovarian surgery can be safely performed in women with adnexal torsion and cystic masses to preserve their reproductive potential, particularly in younger women.
Notes
Ethical approval
This study was approved by the Institutional Review Board (IRB) of the Yonsei University Health System, Severance Hospital. All procedures involving human participants performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Fig. 1
Partial correlation between serum AMH change and variables (A) size of the rotaed ovary, (B) time interval between symptoms and surgery, as determined by correcting for each variable. Control variables: age, BMI, preop AMH, size of the twisted ovary, the interval between symptoms to surgery. AMH, anti-Müllerian hormone; BMI, body mass index; preop, preoperative.
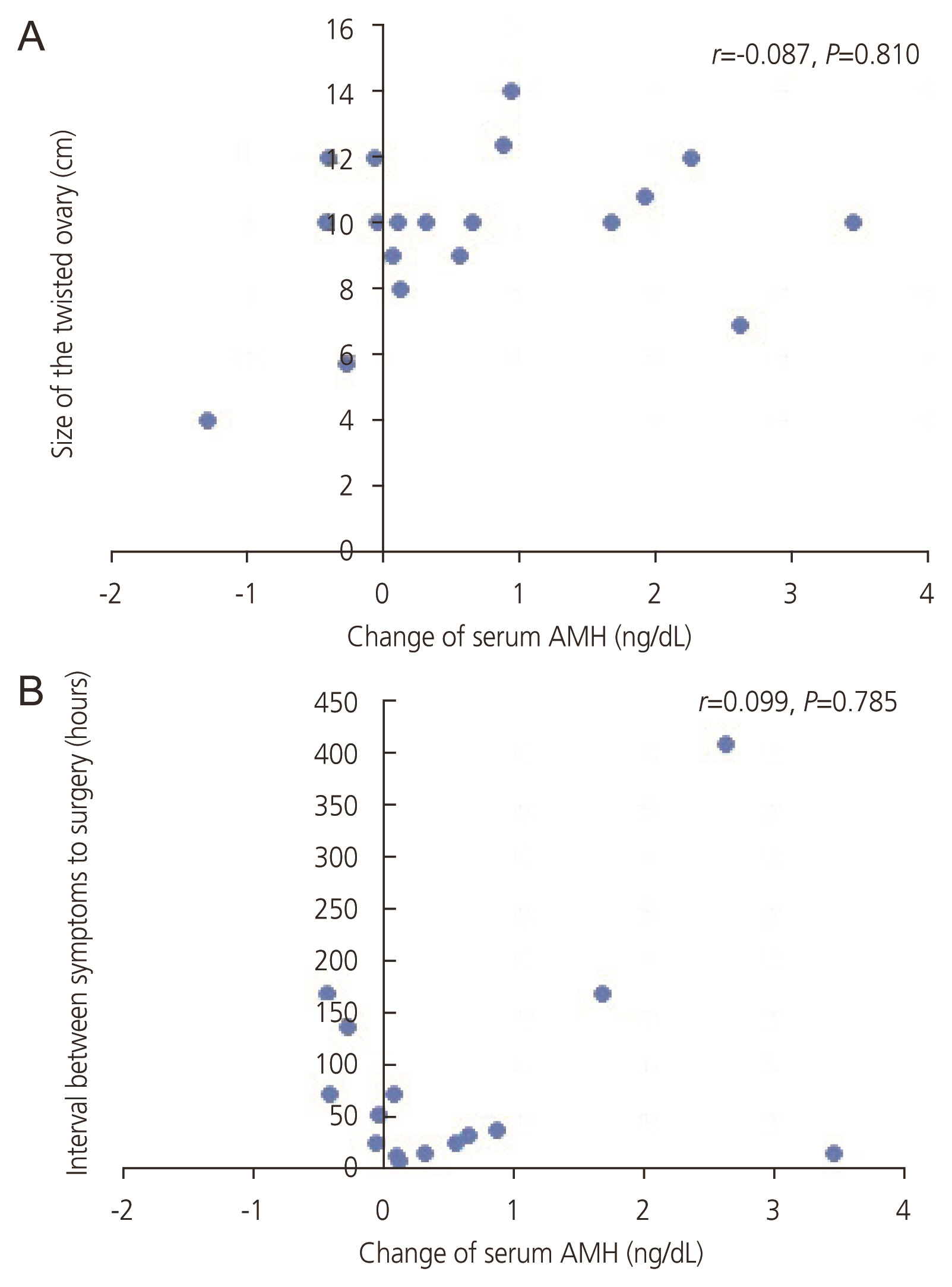
Table 1
Characteristics and postoperative complications of the ovarian preservation group and oophorectomy group
| Ovary preserved (n=56) | Oophorectomy (n=15) | P-value | |
|---|---|---|---|
| Age (yr) | 28.8±8.58 | 36.9±11.41 | 0.01 |
| BMI (kg/m2) | 22.30±3.76 | 25.69±5.74 | 0.05 |
| Preop AMH (ng/mL) | 3.59±3.83 | 2.44±2.94 | 0.11 |
| Preop Hb (g/dL) | 12.85±1.16 | 12.72±1.86 | 0.89 |
| Preop Plt (103/μL) | 275.50±115.41 | 303.26±61.17 | 0.3 |
| Preop WBC (/μL) | 7,922±3,055 | 8,682±4,395 | 0.64 |
| Paina) | 3.16±1.64 | 2.35±2.40 | 0.24 |
| The interval between symptoms to surgery (hours) | 49.77±74.44 | 146.63±430.86 | 0.08 |
| Postop AMH (ng/mL) | 2.98±1.87 | 1.78±2.08 | 0.21 |
| Postop Hb (g/dL) | 11.10±1.16 | 10.93±1.90 | 0.77 |
| Postop Plt (103/μL) | 221.90±52.96 | 238.53±58.40 | 0.32 |
| Postop WBC (/μL) | 8,290±3,399 | 9,536±2,240 | 0.03 |
| Size of the twisted ovary (cm) | 7.22±2.84 | 10.97±4.77 | 0.01 |
| Pregnancy | 7 (12.5) | 0.0 | 0.15 |
| Admission duration (days) | 2.60±1.00 | 3.13±2.29 | 0.57 |
| Postop complication | 1 (1.8) | 0.0 | 0.6 |
| Postop fever | 12 (21.4) | 0.0 | 0.15 |
Table 2
Changes in serum AMH and their characteristics in ovarian preserved group and oophorectomy group with serum AMH values both before and after surgery
| Ovary preserved (n=19)a) | Oophorectomy (n=4)a) | P-value | |
|---|---|---|---|
| Age (yr) | 23.89±9.17 | 36.25±10.17 | 0.025 |
| BMI (kg/m2) | 23.15±4.51 | 22.28±3.70 | 0.725 |
| Preop AMH (ng/mL) | 3.28±2.65 | 3.39±4.53 | 0.949 |
| Postop AMH (ng/mL) | 3.96±2.75 | 1.59±2.30 | 0.124 |
| Change of serum AMH (ng/dL) | 0.68±1.20 | −1.80±2.23 | 0.004 |
| Pain | 3.30±31.54 | 3.00±1.00 | 0.751 |
| The interval between symptoms to surgery (hours) | 83.60±105.10 | 7.33±4.16 | 0.238 |
| Twisted angle (degree) | 980.52±664.68 | 720.00±293.93 | 0.457 |
| Size of the twisted ovary (cm) | 9.78±2.39 | 11.75±4.50 | 0.214 |
| Admission duration (days) | 2.47±0.90 | 2.20±0.95 | 0.660 |
Table 3
Operation findings and types of operations performed in the ovarian preservation group and oophorectomy group
Table 4
Comparison of postoperative serum AMH change rates between patients with ovary discoloration and those without ovary discoloration in the ovarian preservation group
| Ovaries with discoloration (n=9) | Ovaries without discoloration (n=8) | P-value | |
|---|---|---|---|
| Change of serum AMH | 40.0 (−46.1 to +81.1) | 0.2 (−32.5 to +32.7) | 0.248 |
Table 5
Characteristics of patients with and without ovarian mass
| With mass (n=61) | Without mass (n=10) | P-value | |
|---|---|---|---|
| Paina) | 3 (0-7) | 3 (1-6) | 0.43 |
| Pregnancy | 4 (6.6) | 3 (30.0) | 0.02 |
| Size of the twisted ovary (cm) | 8.5 (2.5-20.0) | 5.0 (1.0-7.0) | 0.002 |
| Twisted angle (degree) | 720 (90-2,520) | 540 (180-900) | 0.03 |
| Twisted side | 0.89 | ||
| Right | 38 (62.3) | 6 (60.0) | |
| Left | 23 (37.7) | 4 (40.0) | |
| Twisted direction | 0.8 | ||
| Clockwise | 19 (57.6) | 5 (62.5) | |
| Counterclockwise | 14 (42.4) | 3 (37.5) | |
| Discoloration | 0.91 | ||
| Yes | 17 (28.3) | 3 (30.0) | |
| No | 43 (71.7) | 7 (70.0) | |
| Oophoropexy | 0.01 | ||
| Performed | 3 (4.9) | 3 (30.0) | |
| Not performed | 58 (95.1) | 7 (70.0) | |
| Postop complication | 1 (1.6) | 0.0 | 0.68 |
| Postop fever | 9 (14.8) | 3 (30.0) | 0.23 |
References
1. Spinelli C, Di Giacomo M, Cei M, Mucci N. Functional ovarian lesions in children and adolescents: when to remove them. Gynecol Endocrinol 2009;25:294-8.


2. Spinelli C, Di Giacomo M, Mucci N, Massart F. Hemorrhagic corpus luteum cysts: an unusual problem for pediatric surgeons. J Pediatr Adolesc Gynecol 2009;22:163-7.


3. Lawrence AE, Minneci PC, Deans KJ. Ovarian masses and torsion: new approaches for ovarian salvage. Adv Pediatr 2020;67:113-21.

4. Huchon C, Fauconnier A. Adnexal torsion: a literature review. Eur J Obstet Gynecol Reprod Biol 2010;150:8-12.


7. Göçmen A, Karaca M, Sari A. Conservative laparoscopic approach to adnexal torsion. Arch Gynecol Obstet 2008;277:535-8.



8. Adnexal torsion in adolescents: ACOG committee opinion no, 783 summary. Obstet Gynecol 2019;134:435-6.

9. Rey-Bellet Gasser C, Gehri M, Joseph JM, Pauchard JY. Is it ovarian torsion? A systematic literature review and evaluation of prediction signs. Pediatr Emerg Care 2016;32:256-61.


10. Beaunoyer M, Chapdelaine J, Bouchard S, Ouimet A. Asynchronous bilateral ovarian torsion. J Pediatr Surg 2004;39:746-9.


11. Galinier P, Carfagna L, Delsol M, Ballouhey Q, Lemasson F, Le Mandat A, et al. Ovarian torsion. Management and ovarian prognosis: a report of 45 cases. J Pediatr Surg 2009;44:1759-65.


12. Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000-2006. Pediatrics 2010;125:532-8.



13. McGovern PG, Noah R, Koenigsberg R, Little AB. Adnexal torsion and pulmonary embolism: case report and review of the literature. Obstet Gynecol Surv 1999;54:601-8.

14. Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Pediatric ovarian malignancy presenting as ovarian torsion: incidence and relevance. J Pediatr Surg 2010;45:135-9.


15. Savic D, Stankovic ZB, Djukic M, Mikovic Z, Djuricic S. Torsion of malignant ovarian tumors in childhood and adolescence. J Pediatr Endocrinol Metab 2008;21:1073-8.


16. Templeman C, Hertweck SP, Fallat ME. The clinical course of unresected ovarian torsion. J Pediatr Surg 2000;35:1385-7.


17. Robertson JJ, Long B, Koyfman A. Myths in the evaluation and management of ovarian torsion. J Emerg Med 2017;52:449-56.


18. Bergeron LM, Bishop KC, Hoefgen HR, Abraham MS, Tutlam NT, Merritt DF, et al. Surgical management of benign adnexal masses in the pediatric/adolescent population: an 11-year review. J Pediatr Adolesc Gynecol 2017;30:123-7.


19. Ashwal E, Krissi H, Hiersch L, Less S, Eitan R, Peled Y. Presentation, diagnosis, and treatment of ovarian torsion in premenarchal girls. J Pediatr Adolesc Gynecol 2015;28:526-9.


20. Lipsett SC, Haines L, Monuteaux MC, Hayes K, Michelson KA. Variation in oophorectomy rates for children with ovarian torsion across US children’s hospitals. J Pediatr 2021;231:269-72e1.


21. Celik A, Ergün O, Aldemir H, Ozcan C, Ozok G, Erdener A, et al. Long-term results of conservative management of adnexal torsion in children. J Pediatr Surg 2005;40:704-8.


22. Taskin O, Birincioglu M, Aydin A, Buhur A, Burak F, Yilmaz I, et al. The effects of twisted ischaemic adnexa managed by detorsion on ovarian viability and histology: an ischaemia-reperfusion rodent model. Hum Reprod 1998;13:2823-7.


23. Sommerville M, Grimes DA, Koonings PP, Campbell K. Ovarian neoplasms and the risk of adnexal torsion. Am J Obstet Gynecol 1991;164:577-8.


- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 978 View
- 109 Download
- Related articles in Obstet Gynecol Sci
-
Perioperative changes of serum leptin levels in women with uterine leiomyoma.2006 August;49(8)
The perinatal outcomes of pregnant women with cardiac disease.2007 October;50(10)