 |
 |
- Search
| Obstet Gynecol Sci > Volume 67(1); 2024 > Article |
|
Abstract
Objective
Gender incongruence (GI) is a condition in which an individual’s gender identity, role, and expression differ from their assigned sex. This study aimed to evaluate when GI first arises in transgender and non-binary individuals seeking hormone therapy and their years living untreated in South Korea.
Methods
This retrospective study analyzed GI patients seeking gender-affirming hormone therapy (GAHT) or surgery between 2015 and 2021. The recorded data included gender identity, legal transition status, age of onset of GI, age at the initiation of therapy, and total therapy duration.
Results
In total, 337 patients were enrolled, including 149 (44.2%) transgender men, 153 (45.4%) transgender women, and 35 (10.4%) non-binary individuals. The mean age of onset of GI was 10.6 years (standard deviation, 5.1). Of the total patients, 29% had an onset of GI before age 6 years (preschool), 61% before age 12 (elementary-school), and 87% before age 15 (middle-school). Patients lived with GI for almost 14 years before GAHT initiation at a median age of 23.0 years. 90% of transgender men, 82.3% of transgender women, and 85% of non-binary patients disclosed their gender identities to their families. Regarding social transition, 31.5% of transgender men, 16.3% of transgender women, and none of the non-binary patients (P<0.005) changed their legal gender markers.
Conclusion
Many transgender and non-binary individuals experience GI early in life. These findings emphasized the need for early evaluation, timely gender-affirming care, and more accessible legal processes for gender marker changes in South Korea, aiming to enhance the safety and well-being of these individuals.
Gender identity is an individual’s intrinsic sense of being male, female, or an alternative gender and is usually expressed in their gender role behavior [1]. Most people identify with the gender assigned to them and exhibit behaviors typical of their natal gender. However, very early in life, some people experience incongruence between their experiences and their assigned gender [2]. The development of gender identity and expression is a multidimensional process that involves interactions among numerous factors, such as psychological, social, and biological factors [3]. Although prenatal androgen exposure and specific genetic loci related to transmasculine identity and neuroanatomical regions, including the bed nucleus of the stria terminalis, have been identified as biological factors that influence sex development, their mechanisms remain unclear.
Knowledge of cognitive gender development in individuals with gender-variant identities at an early stage is limited. Children as young as 2 years may indicate that they are of another gender, expressing dislike for the gender associated with their natal sex and behave accordingly [4]. Zaliznyak et al. [5,6] reported that most transgender people first experience gender dysphoria at ≤7 years of age, persisting unaddressed for more than 20 years before commencing gender transition. Recently, 1.4% of youths aged 13-17 years in the USA were identified as transgender [7]. Unaddressed gender dysphoria in childhood and adolescence may have adverse mental and physical health effects, as it does in adulthood [8,9].
Many transgender and non-binary individuals undergo the important process of social gender affirmation to pursue legal gender affirmation by changing the legal gender markers in their identification documents. Possessing a valid government identity document (ID) is necessary to access healthcare, open a bank account, and secure employment resources from which transgender individuals are excluded and marginalized. Legal gender affirmation protects transgender individuals from negative emotional responses, such as depression, anxiety, somatization, and global psychiatric distress [10]. In Korea, transgender individuals can only change their legal gender markers in identification documents with a court order, which is issued to an individual who meets strict requirements, such as undergoing gender-affirming surgery (GAS), including gonadectomy and sterilization, being 19 years of age or older, being unmarried, and other requirements [11]. Based on these restrictions, changing legal gender markers is currently impossible for transgender youth in South Korea. Therefore, even if they have experienced gender incongruence for a long time, young people in Korea cannot change their gender markers until they are ≥19 years of age and meet the above requirements. This study aimed to assess the age at onset of gender incongruence in transgender and non-binary individuals seeking gender-affirming hormone therapy (GAHT), and the number of years that they spend living with untreated gender dysphoria.
This retrospective study was conducted by reviewing the charts of 337 consecutive patients who presented to gender clinic for GAHT or GAS or postoperative care after GAS between January 2015 and December 2021.
Ethics review approval was obtained from the the Institutional Review Board (IRB) at Soonchunhyang University Seoul Hospital (IRB No. 2022-08-004) prior to start of this study. Patients charts were included in the review if they were diagnosed with a gender identity disorder or incongruence by a mental health specialist according to the International Classification of Diseases (ICD)-10/ICD-11 criteria.
For each patients the following variables were recorded: their age and gender identity (male, female, and non-binary gender), legal gender transition status, age at which they began to experience gender incongruence, age at the start of GAHT including gonadotropin-releasing hormone agonists, and total duration of GAHT. Mean and standard deviation (SD) were used for normally distributed quantitative variables; otherwise, median and interquartile range (IQR) were used. Differences were considered statistically significant at a 2-tailed P-value of <0.05. The one-way analysis variance was used to compare the differences among the groups and the Scheffé’s test was used for the post hoc analysis of multiple comparisons. When normality or equal variance test was failed Kruskal-Wallis one-way analysis of variance on ranks was performed. Differences in legal gender transitions among the groups were tested using Pearson’s chi-square analysis. Data were analyzed using SPSS version 27.0 (IBM Corp., Chicago, IL, USA).
A total of 149 (44.2%) transgender men, 153 (45.4%) transgender women, and 35 (10.4%) non-binary individuals were included. The median age of the patients (n=337) included in the chart review was 28.0 years (IQR, 24.5-33.5) (Table 1).
A total of 299 patients reported the age at which they first experienced gender incongruence, with a mean age of 10.6 (SD, 5.1). No significant difference was observed in the age of first experiencing gender incongruence between transgender men (9.3 years old) and transgender women (11.1 years old), whereas non-binary patients reported a significantly older age (13.9 years old) (P=0.000). The earliest ages of experiencing the first gender incongruence were 2, 3, and 6 years for transgender men, transgender women, and non-binary patients, respectively (Table 1).
Furthermore, 87 (29.1%), 96 (32.1%), 78 (26.1%), 22 (7.4%), and 16 (5.4%) patients reported their first experience of gender incongruence in preschool (between the ages of 2 and 6), elementary school (between the ages of 7 and 12), middle school (between the ages of 13 and 15), high school (between the ages of 16 and 18), and 19 years or older, respectively (Fig. 1). Of the total patients, approximately 95% experienced it for the first time when they were children or adolescents. A total of 6.0% (8/133) and 14.3% (19/133) of transgender men and women, respectively, experienced gender incongruence after 16 years or order (after high school), whereas over 33.3% (11/33) of non-binary patients reported experiencing gender incongruence after 16 years or order.
GAHT was initiated at median age of 23.0 years (IQR, 20.0-28.0). No significant differences were observed in age between transgender men, transgender women, and non-binary patients at GAHT initiation (Table 2).
Transgender and non-binary patients had lived with gender dysphoria for almost 14 years before GAHT was initiated. Non-binary patients had the shortest mean number of years of living with gender dysphoria without GAHT (11.4 years [non-binary] vs. 15.0 years [transgender men] and 13.2 years [transgender women], P=0.001).
Transgender men had a mean total duration of hormone therapy of 47.7 months (approximately 4 years), whereas non-binary patients had a mean of 27.2 months, which was shorter than that of transgender men. The mean duration of therapy for transgender women was 35.6 months (Table 2).
A total of 63 (90.0%) transgender men, 79 (82.3%) transgender women, and 17 (85.0%) non-binary patients disclosed their gender identities to their families (Table 2). Furthermore, 47 (31.5%) transgender men and 25 (16.3%) transgender women patients have changed their gender markers, while none of the non-binary patients changed their gender markers in the legal documents (P=0.000) (Fig. 2).
In this study, the mean age at the onset of gender incongruence was 10.6 years, with 29.0%, 61.0%, and 87.0% of patients beginning to experience gender incongruence before the ages of 6, 12, and 15 years, respectively.
Gender incongruence can develop early in life, given that gender learning begins early, with most children identifying their own and others’ genders within 18 and 24 months [12]. One study found that 66.0% of transgender individuals had early onset in childhood compared to 34.0% with late onset after childhood in four countries that participated in the European network to investigate Gender Incongruence [13]. Similar to previous surveys, we found that most transgender individuals experienced gender incongruence early in their lives. Although the mean age was 3-5 years older than that of Zaliznyak et al. [5], the conceptualization of gender-related experiences is likely to be influenced by various factors such as age, race, culture, socioeconomic status, variations in language, and country, and was reported differently by the study, participants, and questionnaire [1,13-18] (Table 3).
Non-binary refers to gender-diverse people who experience and identify their gender as being outside the traditional gender binary of male or female. Many researchers either did not consider non-binary individuals as an independent group in the study population or excluded them from the sub-analysis of sex development owing to the small sample size (Table 3). Most studies on transgender individuals have focused on transgender men and women, whereas non-binary individuals have largely gone unnoticed in health research. However, non-binary individuals comprise approximately 24.0% to over 50.0% of the gender-diverse individuals in recent studies [19,20]. In extensive population-based surveys in Brazil, non-binary identities were more common than binary transgender identities (1.2% vs. 0.7%) [20]. Given that gender-related experiences, intrapersonal progression, and expressions can differ between non-binary and transgender individuals [21], applying a binary-oriented identity narrative to understand the development of non-binary individuals may marginalize the unique experiences of this gender-diverse population. Thus, a multidimensional gender spectrum should be included rather than a dichotomous categorization of gender identity. To the best of our knowledge, this study is the first to quantify the age of the first experience of gender incongruence in non-binary individuals and compare them with other transgender men and women. Non-binary individuals comprised 10.4% (35/337) of the transgender population in this study, and the mean age at which they first experienced gender incongruence was significantly older than that of transgender men and women (13.9 [non-binary] vs. 9.3 [transgender men] and 11.1 [transgender women], P=0.000). While 5.3% of transgender men and 12.4% of transgender women first experienced gender incongruence after 16 years or older (after high school age), over 30.0% of non-binary individuals experienced incongruence first after 16 years or older. Non-binary individuals who do not belong to the binary transgender group may have limited resources and language to explore and articulate their gender identities in the community and in interpersonal relationships. Previous studies have found that invalidation experiences, such as non-binary identity is not “real” or is the result of a “phase,” with self-doubt, confusion, and rumination prevalent among non-binary adolescents [22], and some are unsure or ambivalent about their transgender identity. In contrast, in another study, non-binary individuals reported significantly higher levels of gender and body satisfaction than binary transgender individuals [23]. This intersectional complexity may contribute to the delayed identification of sex among non-binary individuals. Otherwise, 88.6% (31/35) of non-binary individuals in our study reported taking hormone therapy. Even though some non-binary individuals do not have an interest in medical treatment or feel unsure about their needs, others seek gender-affirming care to alleviate gender dysphoria or incongruence and increase body satisfaction through medically necessary interventions. The specific goals of care for non-binary individuals remain unclear. Still, the World Professional Association for Transgender Health recommends health care professionals provide information and gender-affirming medical interventions (GAHT or GAS) for non-binary individuals that affirm their experience of gender in their clinical guidelines [1].
Our findings also showed that the median age at which GAHT therapy was initiated was 23.0 years, indicating that they had not received hormone therapy for a mean of 14 years, despite experiencing gender dysphoria. Childhood and adolescence may be critical periods for the recognition and development of gender identity in transgender individuals, and they can undergo retransition more than once [24]. The estimates of gender diversity ranged from 1.2% to 2.7% among children and adolescents and decreased from 0.3% to 0.5% among adults [25]. Moreover, in more than 25.0% of the cases, gender dysphoria does not persist from childhood to adulthood in the clinical population; however, many adolescents persist in their transgender identity [24,26]. Notably, non-binary youth tend to encounter negative experiences and trauma from gender diversity-related rejection or unaccepting interactions [27-29]. Unaddressed gender dysphoria in childhood and adolescence may have adverse mental and physical health effects, as it does in adulthood [8,9]. In contrast, non-binary children who were accepted for their identities by others and in their communities were generally well adjusted [30]. Timely and appropriate interventions with or without medical support improved mental health outcomes and prevented the harmful effects of growing up with a body that was incongruent with one’s gender identity. Moreover, many studies have found that gender-affirming care, such as puberty suppression, GAHT, or GAS, appears to contribute significantly to the well-being of both binary and non-binary adolescents as well as adults. Almost none of the youths in adulthood regretted the decisions they had taken in adolescence [1,24,31,32].
One of the barriers to accessing GAHT for transgender adolescents is a lack of family approval [33]. Some parents claim that their children’s gender dysphoria is simply an identity crisis common during growth that resolves over time. Other parents or caregivers found it difficult to accept the physical changes, and their reluctance stemmed from concerns about long-term side effects or the fear that their child would regret it later. Therefore, they did not allow their child to access medical care for GAHT. The lack of provider training and knowledge of transgender youths is an additional barrier. Health-care barriers may also lead to self-medication. Transgender youth in Canada are more likely to use non-prescribed hormone therapy if they have negative healthcare experiences or are denied hormone prescriptions [34]. Similarly, a secondary data analysis of a study on transgender women in the USA found that participants had greater odds of using non-prescribed hormones if they were verbally abused [35].
The findings of this study highlight the need for a change in social attitudes toward people with gender dysphoria. Social transition to match an individual’s affirmed gender has also improved psychosocial adjustment and well-being in transgender and non-binary individuals [36]. This process can include actions such as changing names, providing appropriate bathroom/locker rooms or allowing them to use their suitable bathroom/locker rooms for them, communicating affirmed gender to others (on social media, school, or social contacts), and changing sex/gender markers in identification documents. The possession of government ID can be essential to general social life, and transgender individuals are at risk of harassment, assault, and other forms of adverse treatment if they present with an ID that does not match their gender [37]. Nonetheless, changing legal gender markers requires many conditions and steps: they should self-certify inconsistent gender identity and may need certification of gender affirmation from a healthcare provider, a court order for gender change, a changed ID, and other records. According to the 2015 USA Transgender Report, 12.0% of transgender individuals in the US had all ID and documents that stated the updated gender they preferred, whereas more than two-thirds (67.0%) did not have any ID or documents that reflected the gender they preferred. Among those who did not change their ID or documents, one-third (32.0%) could not afford this cost and most (88.0%) of non-binary individuals had no available options (only male or female) that fit their gender-diverse identity [37]. Most individuals in our study who experienced gender incongruence early in life disclosed their gender identities to their families and received GAHT; however, only one in five (none among non-binary individuals) obtained a gender marker that reflected their gender identity. Although not all transgender and non-binary individuals wish to update their gender markers, these results suggest high eligibility barriers, such as procedural, legal, and financial barriers, in the sociocultural context of South Korea in terms of updating gender markers according to the respective genders these individuals identify with. In 2020, courts in South Korea gradually began to allow gender correction without prior GAS, such as phalloplasty or hysterectomy and ovariectomy [11]. In addition, in 2022, the plenary decision of the Korean Supreme Court declared that a transgender individuals who have had children could request a change of gender in the family register.
Our study requires caution in its interpretation due to some limitations. First, these results may not be generalizable to transgender and non-binary individuals who do not seek medical care. Regarding gender marker changes, our findings may not represent those who were trying or failed to change gender markers owing to age restrictions or harsh barriers. Second, answers regarding the age at first sex-related experience were dependent on the patient’s long-term memories, which are likely to be subject to recall bias. Finally, this study does not investigate other types of gender affirmation in social transitions or disclosure trajectories. There are various developmental contexts, disclosure stages, desires, and transition, processes from the onset of gender-nonconforming feelings to changing gender markers or initiating gender-affirming medical treatments. Furthermore, data on individual mental health problems were not collected. However, this issue was not within the scope of this study, and future studies should assess the risk of health outcomes associated with prolonged periods of care deprivation.
Summarily, our data showed that most transgender and non-binary individuals had existed without GAHT for several years or without changing their legal gender markers while experiencing gender incongruence early in life. Based on these results, providing early evaluation, timely gender-affirming care, and easing legal requirements for gender marker changes for the safety and well-being of transgender and non-binary individuals are necessary.
Notes
Fig. 1
Age distribution of initial gender incongruence experience in transgender men, transgender women, and non-binary individuals.
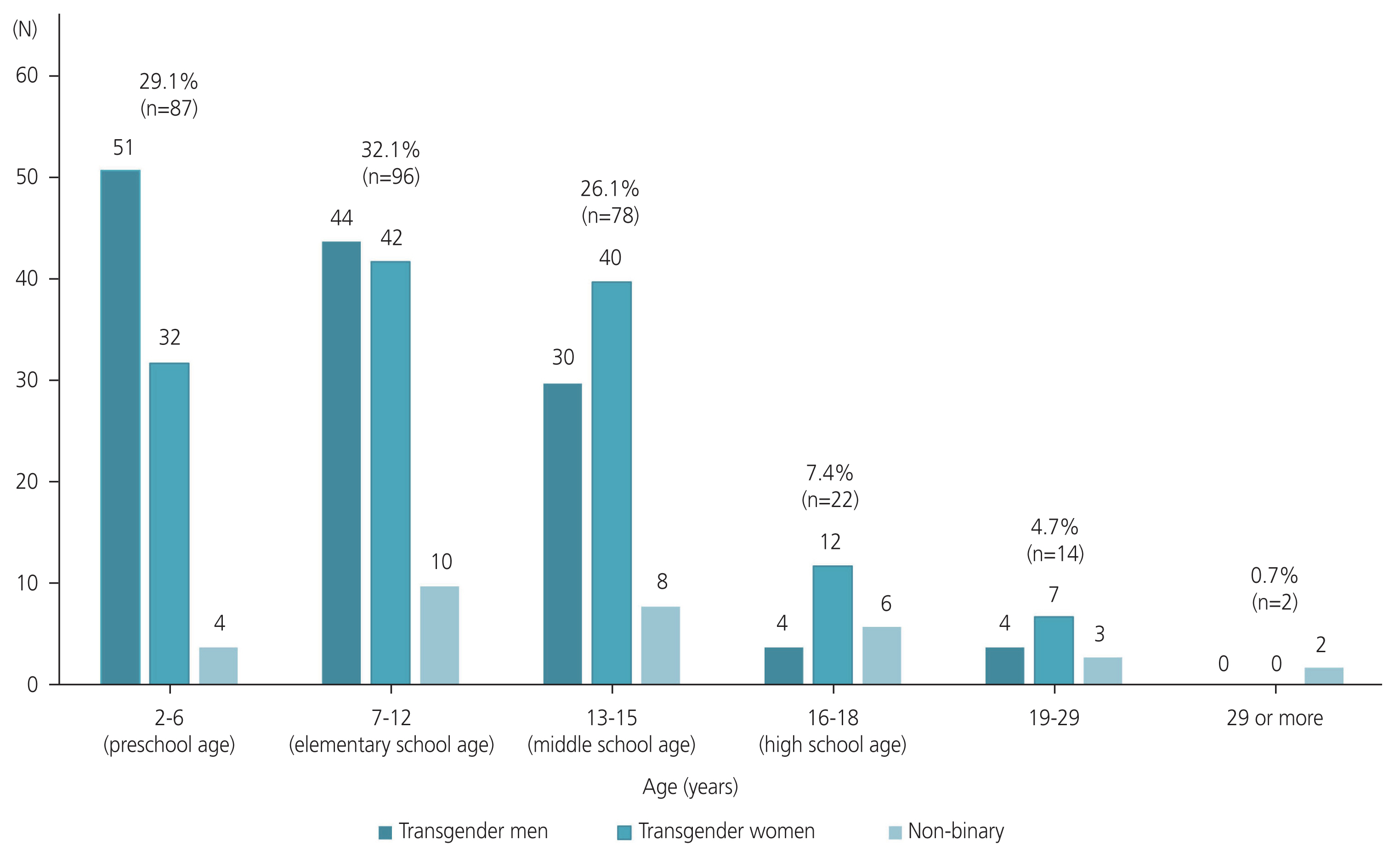
Table 1
Age of initial gender incongruence experience among transgender and non-binary individuals
| Clinical characteristic | Total (n=337) | Transgender men (n=149) | Transgender women (n=153) | Non-binary gender (n=35) | Significance |
|---|---|---|---|---|---|
| Age (yr) | 28.0 (24.5-33.5) | 29.0 (25.0-34.0) | 28.0 (24.0-33.0) | 26.0 (25.0-33.0) | 0.359a) |
| Age at first visit for gender affirming hormone therapy (yr) | 25.0 (21.0-30.0) | 25.0 (21.0-30.5) | 25.0 (21.0-29.0) | 25.0 (22.0-29.0) | 0.756a) |
| Age at which patient first experienced gender incongruence (yr) | 10.6±5.1 (2-38) | 9.3±4.6b) (2-23) | 11.1±4.8b) (3-26) | 13.9±6.9 (6-38) | 0.000c) |
| Responses, no | 299 | 133 | 133 | 33 |
Table 2
Gender affirming transition status
| Total (n=337; 100.0%) | Transgender men (n=149; 44.2%) | Transgender women (n=153; 45.4%) | Non-binary gender (n=35; 10.4%) | Significance | |
|---|---|---|---|---|---|
| Gender affirming hormone therapy, yes | 312 (92.6) | 136 (91.3) | 145 (94.8) | 31 (88.6) | 0.323a) |
| Age at which gender affirming hormone therapy was initiated (yr) | 23.0 (20.0-28.0) | 23.0 (20.0-28.0) | 23.0 (20.0-26.0) | 24.0 (22.0-28.25) | 0.321b) |
| Duration for which the patients lived with gender incongruence before initiating gender affirming hormone therapy (yr) | 13.8±7.7 | 15.0±7.4e) | 13.2±8.1d),e) | 11.4±6.9d) | 0.001c) |
| Total duration of gender affirming hormone therapy (months) | 40.2±42.5 | 47.7±47.5d) | 35.6±34.9d),e) | 27.2±44.1e) | 0.016c) |
| Did you disclose your gender incongruence to your family? | |||||
| No | 186 | 70 | 96 | 20 | |
| Yes | 159 (85.5) | 63 (90.0) | 79 (82.3) | 17 (85.0) | 0.379a) |
Table 3
Previous studies on the age of onset of gender incongruence among transgender and non-binary individuals
| Study | Country | Number of study population (FtM vs. MtF vs. non-binary) | Age group (yr) | Questions related to the development of gender identity | FtM, age (yr) | MtF, age (yr) | Significant difference between FtM and MtF | Whether the study population includes non-binary individuals | Classified non-binary as an independent group |
|---|---|---|---|---|---|---|---|---|---|
| Zaliznyak et al. [5,6] (2021) | USA | 210 (55 vs. 155 vs. N/A) | Older adolescents and adults (35.4±10.8 in FtM vs. 41.3±16.3 in MtF; range: over 16) | Age at which they first experienced gender dysphoria | 6.2±3.1 | 6.7±3.6 | Not significant | No | N/A |
| Grossman et al. [15] (2005) | USA | 55 (24 vs. 31 vs. N/A) | Youth (19.5±1.6 in FtM vs. 17.5±1.6 in MtF; range: 15-21) | Feeling different from others | 7.5±3.1 | 7.6±3.1 | Not significant | No | N/A |
| Olson et al. [16] (2015) | USA | 98 (44 vs. 44 vs. 10) | Youth (19.2±2.86; range: 12-24) | Age realized gender different from assigned | 8.4±4.7 | 8.2±4.4 | Not significant | Yesa) (gender queer, bigender, gender bender, gender fluid, and others) | N/A |
| Kuper et al. [17] (2019) | USA | 224 (133 vs. 86 vs. 5) | Children and youth (14.7±2.5; range: 6-17) | First self-identified with current gender | 10.7±3.6 | 9.9±4.6 | Not significant | Yesa) (male spectrum, female spectrum, and nonbinary) | No (participants who identified as non-binary were excluded from sub-analysis due to small size [n=5]) |
| Nieder et al. [18] (2011) | Four countries participated in the ENIGI network: The Netherlands, Belgium, Germany, and Norway | 170 (77 vs. 93 vs. N/A) | Older adolescents and adults (32.81±12.1; range: 16-75) | Early-onset transsexual development was defines as meeting Criteria A and B of Gender Identity Disorder in Childhood as outlined in DSM-IV (“a strong cross-gender identification,” “persistent discomfort about her or his assigned sex”) | 77.9% (60/77) developed early-onset FtM trans-sexual | 38.7% (36/93) developed early-onset MtF trans-sexual | Significant | No | N/A |
References
1. Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health 2022;23(Suppl 1):S1-259.


2. Cohen-Kettenis PT, Klink D. Adolescents with gender dysphoria. Best Pract Res Clin Endocrinol Metab 2015;29:485-95.


3. Korpaisarn S, Safer JD. Etiology of gender identity. Endocrinol Metab Clin North Am 2019;48:323-9.


4. Steensma TD, Kreukels BP, de Vries AL, Cohen-Kettenis PT. Gender identity development in adolescence. Horm Behav 2013;64:288-97.


5. Zaliznyak M, Bresee C, Garcia MM. Age at first experience of gender dysphoria among transgender adults seeking gender-affirming surgery. JAMA Netw Open 2020;3:e201236.



6. Zaliznyak M, Yuan N, Bresee C, Freedman A, Garcia MM. How early in life do transgender adults begin to experience gender dysphoria? Why this matters for patients, providers, and for our healthcare system. Sex Med 2021;9:100448.




7. Herman JL, Flores AR, O’Neill KK. How many adults and youth identify as transgender in the United States?. Los Angeles (CA): The Williams Institute, UCLA School of Law; 2022.
8. Lim HH, Jang YH, Choi GY, Lee JJ, Lee ES. Gender affirmative care of transgender people: a single center’s experience in Korea. Obstet Gynecol Sci 2019;62:46-55.




9. Connolly MD, Zervos MJ, Barone CJ 2nd, Johnson CC, Joseph CL. The mental health of transgender youth: advances in understanding. J Adolesc Health 2016;59:489-95.


10. Restar A, Jin H, Breslow A, Reisner SL, Mimiaga M, Cahill S, et al. Legal gender marker and name change is associated with lower negative emotional response to gender-based mistreatment and improve mental health outcomes among trans populations. SSM Popul Health 2020;11:100595.



11. Supreme Court in Korea. The guidelines for the handling of petition for legal sex change permit of transgender people [Internet] Seoul: Supreme Court in Korea; c2020 [cited 2023 Sep 20]. Available from: https://glaw.scourt.go.kr/wsjo/gchick/sjo330.do?contId=3226349#//
.
12. Serbin LA, Poulin-Dubois D, Colburne KA, Sen MG, Eichstedt JA. Gender stereotyping in infancy: visual preferences for and knowledge of gender-stereotyped toys in the second year. Int J Behav Dev 2001;25:7-15.


13. Heylens G, Elaut E, Kreukels BP, Paap MC, Cerwenka S, Richter-Appelt H, et al. Psychiatric characteristics in transsexual individuals: multicentre study in four European countries. Br J Psychiatry 2014;204:151-6.


14. Subramanian T, Chakrapani V, Selvaraj V, Noronha E, Narang A, Mehendale S. Mapping and size estimation of Hijras and other trans-women in 17 states of India: first level findings. Int J Health Sci Res 2015;5:1-10.
15. Grossman AH, D’Augelli AR, Howell TJ, Hubbard S. Parent’reactions to transgender youth’gender nonconforming expression and identity. J Gay Lesbian Soc Serv 2005;18:3-16.

16. Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Health 2015;57:374-80.



17. Kuper LE, Lindley L, Lopez X. Exploring the gender development histories of children and adolescents presenting for gender affirming medical care. Clin Pract Pediatr Psychol 2019;7:217-28.

18. Nieder TO, Herff M, Cerwenka S, Preuss WF, Cohen-Kettenis PT, De Cuypere G, et al. Age of onset and sexual orientation in transsexual males and females. J Sex Med 2011;8:783-91.


19. Burgwal A, Gvianishvili N, Hård V, Kata J, García Nieto I, Orre C, et al. Health disparities between binary and non binary trans people: a community-driven survey. Int J Transgend 2019;20:218-29.



20. Spizzirri G, Eufrásio R, Lima MCP, de Carvalho Nunes HR, Kreukels BPC, Steensma TD, et al. Proportion of people identified as transgender and non-binary gender in Brazil. Sci Rep 2021;11:2240.




21. Tatum AK, Catalpa J, Bradford NJ, Kovic A, Berg DR. Examining identity development and transition differences among binary transgender and genderqueer nonbinary (GQNB) individuals. Psychol Sex Orient Gend Divers 2020;7:379-85.

22. Johnson KC, LeBlanc AJ, Deardorff J, Bockting WO. Invalidation experiences among non-binary adolescents. J Sex Res 2020;57:222-33.


23. Jones BA, Pierre Bouman W, Haycraft E, Arcelus J. Gender congruence and body satisfaction in nonbinary transgender people: a case control study. Int J Transgend 2019;20:263-74.



24. Cohen-Kettenis PT, Steensma TD, de Vries AL. Treatment of adolescents with gender dysphoria in the Netherlands. Child Adolesc Psychiatr Clin N Am 2011;20:689-700.


25. Zhang Q, Goodman M, Adams N, Corneil T, Hashemi L, Kreukels B, et al. Epidemiological considerations in transgender health: a systematic review with focus on higher quality data. Int J Transgend Health 2020;21:125-37.



26. Martin A, Volkmar FR, Bloch MH. Lewis’s child and adolescent psychiatry: a comprehensive textbook. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2017.
27. Roberts AL, Rosario M, Slopen N, Calzo JP, Austin SB. Childhood gender nonconformity, bullying victimization, and depressive symptoms across adolescence and early adulthood: an 11-year longitudinal study. J Am Acad Child Adolesc Psychiatry 2013;52:143-52.



28. Gower AL, Rider GN, Brown C, McMorris BJ, Coleman E, Taliaferro LA, et al. Supporting transgender and gender diverse youth: protection against emotional distress and substance use. Am J Prev Med 2018;55:787-94.



29. Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex 2006;51:111-28.


30. Olson KR, Durwood L, DeMeules M, McLaughlin KA. Mental health of transgender children who are supported in their identities. Pediatrics 2016;137:e20153223.




31. Rider GN, Vencill JA, Berg DR, Becker-Warner R, Candelario-Pérez L, Spencer KG. The gender affirmative lifespan approach (GALA): a framework for competent clinical care with nonbinary clients. Int J Transgend 2019;20:275-88.



32. de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 2014;134:696-704.



33. Silberholz EA, Brodie N, Spector ND, Pattishall AE. Disparities in access to care in marginalized populations. Curr Opin Pediatr 2017;29:718-27.


34. Rotondi NK, Bauer GR, Scanlon K, Kaay M, Travers R, Travers A. Nonprescribed hormone use and self-performed surgeries: “do-it-yourself” transitions in transgender communities in Ontario, Canada. Am J Public Health 2013;103:1830-6.



35. de Haan G, Santos GM, Arayasirikul S, Raymond HF. Non-prescribed hormone use and barriers to care for transgender women in San Francisco. LGBT Health 2015;2:313-23.


36. Ehrensaft D, Giammattei SV, Storck K, Tishelman AC, Keo-Meier C. Prepubertal social gender transitions: what we know; what we can learn-a view from a gender affirmative lens. 1st ed. Routledge: Today’s Transgender Youth; 2020. p. 137-54.
37. James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The report of the 2015 US transgender survey. Washington, DC: National Center for Transgender Equality; 2016.






















