 |
 |
- Search
| Obstet Gynecol Sci > Volume 67(1); 2024 > Article |
|
Abstract
Objective
Parametrial tissue ligation during total laparoscopic hysterectomy (TLH) is important in large uteri with large vessels.
Methods
A retrospective study was performed at Asan Medical Center for comparing TLH performed with a new knotless parametrial tissue ligation method and conventional laparoscopic-assisted vaginal hysterectomy (LAVH) from March 2019 to August 2021. For TLH, after anterior colpotomy, the parametrial tissue was ligated by anchoring the suture and making a loop in one direction three times using 1-0 V-LocTM 180 (Covidien, Mansfield, MA, USA) suture. Subsequently, the cranial part of the loop was cut using an endoscopic device.
Results
A total of 119 and 178 patients were included in the TLH and LAVH groups, respectively. The maximal diameter of the uterus was larger in the TLH group (106.29±27.16 cm) than in the LAVH group (99.00±18.92 cm, P=0.01). The change in hemoglobin (Hb) level was greater in the LAVH group than in the TLH group (P<0.001). The weight of the removed uterus was greater in the TLH group than in the LAVH group (431.95±394.97 vs. 354.94±209.52 g; P=0.03). However, when the uterine weight was >1,000 g, the operative times and change in Hb levels were similar between the two groups. In both groups, no ureteral complications occurred during or after surgery.
Hysterectomy is one of the major surgeries performed for benign gynecological diseases. Laparoscopic hysterectomy (LH), including total laparoscopic hysterectomy (TLH) and laparoscopy-assisted vaginal hysterectomy (LAVH), has advantages over open abdominal hysterectomy, including faster recovery, shorter hospitalization, better cosmetic results, and fewer wound complications [1]. Recently, there has been a growing interest in minimally invasive surgery, with various attempts to reduce port incisions, such as by using one or two incisions instead of the traditional three incisions, even in LH [2,3]. However, advanced skills are needed to perform LH owing to technical difficulties such as crowding of instruments and lack of triangulation [4]. In particular, TLH requires more technical skills and has a steeper learning curve than LAVH because TLH requires dissection of the entire uterus, ligation of the uterine vessels, and suturing of the vaginal stump exclusively via a laparoscopic approach [5]. On the other hand, LAVH, which combines laparoscopic and vaginal access, may be difficult if there are pelvic adhesions from prior pelvic surgeries or if the vagina is narrow [5,6]. Therefore, choosing an appropriate hysterectomy method according to the patient’s characteristics, uterus size, and the surgeon’s experience is important [7].
Uterine vessel ligation is one of the most important aspects of hysterectomy procedures; however, this can be difficult if the patient has a pathological pelvic condition. In cases with pelvic adhesions or large uteri, uterine vessel ligation may be difficult due to distorted pelvic anatomies and congestion of the uterine vessels, especially during TLH [2,8,9]. In this context, several studies have reported techniques for uterine vessel ligation [10-12]. Among these, the use of conventional bipolar electrocautery or other advanced energy devices for vessel sealing is a simple and common method for vessel ligation. However, these tools are most suitable for vessels with a diameter of <7 mm due to the risk of thermal damage to adjacent tissues. Notably, surgical complications related to electrocautery occur in over 25.0% of cases; hence, caution is required, especially when sealing large vessels [13,14].
Classical suturing techniques can minimize the risk of thermal injury and typically result in acceptable levels of blood loss [10,12]. However, tying knots with laparoscopic instruments requires advanced knotting skills, with a constant need for traction to prevent the tie from loosening, which can lengthen the total operative time [15]. In a prior study, uterine vessel ligation using a Hem-o-lok clip demonstrated similar surgical outcomes as with conventional methods [11]. The Hem-o-lok clip has the advantages of being non-slip and providing good hemostasis due to its strong gripping force on the blood vessels; however, it has the disadvantage of easily tearing the venous vessels if applied incorrectly [11]. In addition, in order to apply the clip, it is necessary to apply the clip at an appropriate angle after sharp dissection of the uterine vessels and surrounding tissues. However, if the uterus is large and the uterine vessels are congested, tearing of the blood vessels can easily occur during uterine vessel skeletonization. Ultimately, the key is to make uterine vessel ligation simpler and safer during TLH, even in cases involving large uteri. Given that the surgeon typically has only two hands to work with, when performing TLH using a reduced port, if the size of the uterus is large and the pelvic cavity is narrow, the uterus must be pushed with one hand to expose the uterine vessels to secure the field of view. At the same time, the uterine vessels need to be ligated with the other hand, and because only one hand needs to be used, a simple and effective method of ligating the uterine blood vessels without a knot tie would be useful.
The novel surgical method we developed uses 1-0 V-LocTM 180 sutures (Covidien, Mansfield, MA, USA), which are knotless absorbable barbed sutures with a well-established record of safety and effectiveness in various surgeries in obstetrics and gynecology [16-18]. However, a surgical method for uterine vessel ligation using 1-0 V-LocTM 180 sutures during TLH has not yet been published. Therefore, the purpose of this study was to evaluate the safety and feasibility of a knotless uterine artery ligation method using 1-0 V-LocTM 180 suture and to compare it with LAVH techniques that are routinely performed for benign diseases. In addition, by providing our experience and surgical tips for this knotless uterine artery ligation method, we aim to offer another surgical option that allows the operator to perform TLH more easily and safely compared to LAVH.
We retrospectively analyzed the medical records of patients who underwent LAVH or TLH for benign uterine disease at Asan Medical Center Hospital from March 2019 to August 2021. We included TLH performed through both robotic and laparoscopic surgery. The exclusion criteria were as follows: patients who underwent chemotherapy or additional surgery after uterine malignancy was confirmed by biopsy after surgery, patients who underwent LH for extrauterine disease, patients who underwent blood vessel ligation only using an energy device, and LH performed by surgeons who performed less than four LH surgeries a month in their clinical practice.
The following variables were included as patient baseline characteristics: age, body mass index (BMI), number of gravida and vaginal deliveries, menopause status, and previous pelvic surgery. All patients underwent preoperative ultrasonography and measurement of the longitudinal, transverse, and anteroposterior diameters of the uterus. The primary outcome encompassed the surgical outcomes of TLH and LAVH. The following variables were collected to assess the operative outcomes: concomitant surgery, number of incisions required for port insertion, total operative time (incision to close), route of uterine retrieval (vaginal or umbilical), estimated blood loss (EBL), change in hemoglobin (Hb) level (difference between pre- and postoperative levels), transfusion rate, length of hospital stay, the weight of the removed uterus on pathological examination, and any complications during or after surgery over 1 month.
The secondary outcome encompassed the surgical outcomes (operative time and change in Hb levels) for both TLH and LAVH according to the largest diameter of the uterus and weight of the uterus. Patients were divided into three categories according to the maximal diameter of the uterus (<10 cm, 10 to <15 cm, and ≥15 cm) and four categories according to the weight of the uterus (<250 g, 250 to <500 g, 500 to <1,000 g, and ≥1,000 g). This study was approved by the Asan Medical Center Institutional Review Board (approval no. 2021-1101).
All surgeries were performed under general anesthesia, with patients placed in the dorsal lithotomy position, and a Foley catheter was inserted into the bladder. Subsequently, a uterine manipulator, such as the RUMI Arch™ (CooperSurgical Inc., Trumbull, CT, USA) or BUMI (Sejong Medical, Paju, Korea), was placed. A reduced-port method with a total of one to three skin incisions was used in all cases. A 2 cm intraumbilical incision was made using the open Hasson technique, and a multichannel single port (Gloveport A-Type; Nelis Meditech Inframed, Bucheon, Korea) was inserted for single-port LH. For multiport LH, a 5 mm port was placed in the suprapubic area with or without an additional 5 mm port in the left lower quadrant site. For robotic TLH, a da Vinci Si, Xi, or SP system (Intuitive Surgical, Sunnyvale, CA, USA) was used with a 2.5-2.7 cm intraumbilical incision, and one or two additional 8 mm ports were made on the left and right sides of the umbilicus. In our facility, robotic LAVH is rarely performed for benign uterine diseases, as robotic LAVH requires time to undock the robot arm and readjust the patient’s lithotomy position angle during a vaginal approach, which may affect the overall operative time. Therefore, robotic LAVH was excluded from this study.
During TLH, both the round and ovarian or infundibulopelvic ligaments were ligated using an electrosurgical bipolar vessel sealing device depending on whether the adnexa was removed. Subsequently, the anterior and posterior aspects of the broad ligament were dissected to the level of the uterine vessels. Next, vesicovaginal and rectovaginal space dissection and anterior and posterior colpotomy were performed with the help of an assistant pushing the manipulator. After anterior colpotomy, with the cervical cap exposed and the anterior vaginal cuff almost resected, the uterine vessels were sutured using 1-0 V-LocTM 180 (Fig. 1). At this time, one hand was used to push the uterus laterally using an endoscopic instrument such as a dissector or grasper to expose the uterine vessels. The other hand was used to ligate the uterine vessels by first anchoring one suture and then making a loop in one direction approximately 3-4 times using the endoscopic needle holder through the umbilical port. After that, the cranial part of the tie was cut using an endoscopic energy device. After circular colpotomy was completed, the uterus was detached from the vault, and the uterine manipulator was removed. If the size of the uterus was small or the pubic arch was wide, the uterus was delivered through the vagina. If not, the uterus was removed through the umbilicus using cold blade morcellation within an endobag before the operation was completed. If the uterus was too large to fit in the bag, manual morcellation with a cold blade was performed externally to avoid spillage. The vaginal cuff was laparoscopically sutured bi-directionally with a continuous running suture using the remaining 1-0 V-LocTM 180 after the ligation of both uterine vessels and then stitched at the midline. TLH with 1-0 V-LocTM 180 was performed by one surgeon (L.S.R.) who had previously performed over 1,000 TLH surgeries.
For LAVH, the procedure was conducted following the same steps as TLH up to the point above the level of the uterine vessels. After laparoscopic dissection of the vesicovaginal and rectovaginal spaces, the surgical procedure transitioned to the vaginal route. Anterior and posterior colpotomy was performed, and the uterosacral ligaments, cardinal ligaments, and uterine vessels were clamped, cut, and tied. After removal of the uterus through the vagina, the vaginal cuff was closed with a running suture. All ties were performed using delayed absorbable polyglactin 1-0 suture. LAVH was performed by one surgeon (K.S.H.) who had previously performed over 1,000 LAVH surgeries.
All patients received standard postoperative care, including the administration of patient-controlled analgesia or nonsteroidal anti-inflammatory drugs thrice a day until the second postoperative days. The patients were discharged on the second day after surgery when their vital signs were stable. If there were complications such as abdominal pain, fever, or bleeding after surgery, the patients were hospitalized for a few more days until the problem was resolved.
Categorical variables were presented as numbers with percentages, while continuous variables were presented as the mean±standard deviation or the median with the interquartile range. Paired t-tests or Wilcoxon signed-rank tests were performed for continuous variable comparisons between groups. The chi-squared test and Fisher’s exact test were used for categorical variables. A P-value <0.05 indicated statistical significance. All statistical analyses were conducted using R statistical software (version 3.6.3; R Foundation for Statistical Computing, Vienna, Austria) [19].
A total of 119 and 178 patients in the TLH and LAVH groups, respectively, were included in this study. Age, BMI, gravidity, menopause status, and preoperative Hb level did not significantly differ between the two groups (P>0.05). The number of vaginal deliveries was higher in the LAVH group (P=0.05); however, no difference was observed between the two groups when comparing patients with no history of vaginal delivery and those with more than one vaginal delivery (P=0.07). The TLH group had more patients who had undergone previous pelvic surgery (P=0.03). No difference was observed between the two groups in terms of surgical indications (P=0.28). The mean maximal diameter of the uterus measured by preoperative ultrasonography was larger in the TLH group (106.29±27.16 cm) than in the LAVH group (12.18±1.61 cm; P=0.01). When divided into three groups based on uterine size (<10 cm, 10 to <15 cm, and ≥15 cm), patients in the TLH group had larger uteri than those in the LAVH group, with a marginally significant difference (P=0.05) (Table 1).
The total operative time and length of hospital stay did not differ between the two groups. In the LAVH group, more concomitant surgeries occurred, all of which were adnexa surgeries. The three surgical cases other than adnexa surgery performed in the TLH group were posterior colporrhaphy in a patient with rectocele, tension-free vaginal taping for stress urinary incontinence, and bilateral double J ureteral stent insertion in a patient with severe pelvic adhesions due to four previous pelvic surgeries.
The TLH group had a greater number of ports than the LAVH group. The EBL, change in Hb level, and transfusion rate were significantly higher in the LAVH group than in the TLH group (P<0.001). The mean weight of the removed uterus was significantly higher in the TLH group than in the LAVH group (431.95±394.97 vs. 354.94±209.52 g; P=0.03). When divided into four groups based on uterine weight (<250 g, 250 to <500 g, 500 to <1,000 g, and ≥1,000 g), patients in the TLH group had a heavier uterus than those in the LAVH group; however, no significant difference (P=0.09) (Table 2) was observed.
The surgical outcomes according to the maximal diameter of the uterus based on preoperative ultrasonography are shown in Table 3. When the size of the uterus was <10 cm, in the TLH group, the median operative time was significantly shorter than that in the LAVH group (P<0.01). In addition, the median EBL and change in Hb level were significantly lower in the TLH group compared to the LAVH group. When the size of the uterus measured >10 cm and <15 cm, the median operative time was 105 minutes in the two groups, lacking a statistically significant difference (P=0.34). However, the median EBL and change in Hb level were lower in the TLH group than in the LAVH group (P<0.01). Moreover, when the size of the uterus measured >15 cm, the median operative time, EBL, and change in Hb level were not different between the two groups.
The surgical outcomes according to the weight of the uterus are shown in Table 4. The median operative time was shorter in the TLH group than in the LAVH group when the uterine weight was less than 250 g (P=0.01), but no difference was observed between the two groups when the uterine weight measured >250 g. The median EBL was significantly lower in the TLH group when the uterine weight was <1,000 g (P<0.01). In addition, when the uterine weight was >250 g and <1,000 g, the median change in Hb level was significantly lower in the TLH group than in the LAVH group (250 to <500 g, P<0.01; 500 to <1,000 g, P=0.03). However, when the uterine weight was >1,000 g, the median operative time, EBL, and change in Hb level were not different between the two groups.
Intraoperative complications occurred in two (1.7%) and four (2.2%) cases in the TLH and LAVH groups, respectively; all of these were bladder and bowel injuries, with no statistical difference between the two groups (P=0.94). All six complications occurred during adhesiolysis and were not related to the V-Loc suturing of the uterine vessels. Overall, no significant difference was observed in the postoperative complication rate between the two groups. In the TLH group, two cases of peritonitis were associated with intraoperative small bowel injury and a vault infection, respectively. In the case of hemoperitoneum in the TLH group, a hematoma without a bleeding focus was confirmed on computed tomography (CT), and after conservative care, the patient was stably discharged. In the LAVH group, peritonitis with complicated fluid collection was confirmed on CT in five cases. Two cases of hemoperitoneum were associated with adnexal bleeding. In both groups, no ureteral complications such as ureteral injury or ureteral kinking during or after surgery occurred (Table 5).
In this study, knotless uterine artery ligation using 1-0 V-LocTM 180 suture in TLH was found to be a feasible and effective surgical option, without an increased risk of ureteral injury or uterine vessel bleeding. In addition, this method can be safely applied even in complicated cases with large uteri.
The primary outcome encompassed the surgical outcomes of TLH and LAVH. Although the weight of the removed uterus was heavier in the TLH group compared to the LAVH group, the operative time was similar, and the EBL was lower. The secondary outcome encompassed the surgical outcomes of TLH and LAVH according to the largest diameter of the uterus and weight of the uterus. Based on the study results, TLH demonstrated reduced EBL and fewer changes in Hb levels in patients with large and heavy uteri in comparison to LAVH. However, when the uterine size was extremely large and heavy (over 15 cm or 1,000 g), no significant differences in EBL or changes in Hb levels were observed between the two surgeries.
Although several studies comparing TLH and LAVH have been reported, drawing conclusions about the effectiveness of these surgeries is difficult owing to the heterogeneity of the study populations and differences in the surgical skills of surgeons [1]. A multicenter retrospective study showed that TLH was associated with less blood loss than LAVH (173.1±188.2 mL vs. 456.8±893.7 mL, P<0.05) and reported similar operative times, uterine weight distributions, and complication rates to our study [20]. Similarly, in another retrospective study, TLH resulted in less drastic changes in Hb levels than LAVH [8]. However, the uterine weights were significantly heavier in the LAVH group than in the TLH group (270.87±145.93 g vs. 189.70±108.98 g, P<0.01); hence, the author concluded that LAVH may be preferred if the uterus is relatively large. A recent retrospective study also suggested that LAVH had the advantage of a shorter operative time compared to TLH (76.9±25 minutes vs. 124±39.7 minutes, P=0.0001) [5]. In the aforementioned studies, TLH surgery was performed with the use of bipolar coagulation, except at the vaginal cuff closure step. However, in our study, the EBL and change in Hb level in the TLH group were significantly lower than those in the LAVH group; the operative time was also shorter, although the difference was not statistically significant. Notably, in our study, which had the largest number of patients, the mean uterine weights for TLH and LAVH were much heavier than those reported in previous studies. Therefore, we suggest that both TLH and LAVH are feasible methods, and TLH with knotless uterine artery ligation using 1-0 V-LocTM 180 suture may have more advantages in terms of blood loss.
Adequate uterine vessel ligation is a key step in hysterectomy because most of the blood supply to the uterus enters through the uterine arteries [21]. In addition, as the size of the uterus increases, the volume of intraoperative blood loss increases [22]. However, when TLH is performed on a large uterus, there is a valid concern regarding limited access to the uterine vessels due to poor exposure. In addition, it may increase the risk of bleeding and injury to adjacent organs such as the bowel and ureter. Therefore, developing an appropriate surgical method is important for risk reduction, particularly in patients with large uteri.
Several studies have investigated the efficacy of TLH in patients with large uteri. In a retrospective study of 989 cases of TLH with uterine artery ligation using bipolar coagulation, it was reported that the heavier the uterus was, the longer the operative time and the greater the EBL [23]. However, the operative time was shorter in our study at all uterine weights, and the EBL was similar between uterine weights of 250 and 1,000 g. Sinha et al. [24] performed TLH using a modified technique in patients with an enlarged uterus larger than 500 g. In this approach, devascularization was achieved by ligating the uterine vessels using 1-0 Vicryl suture; then, the enlarged uterus was reduced through myoma morcellation or supracervical hysterectomy. The operative time and EBL closely resembled the findings in our study. However, a potential concern with this modified technique is that the morcellation technique in situ has a risk of disseminating leiomyosarcoma [25].
Given the advanced endosuturing skills required for uterine vessel ligation using the conventional suturing technique and the associated risk of thermal injury when using an energy device, there was a pressing need for a new method to address these challenges [10,26]. However, studies on new methods of uterine vessel ligation during TLH are very limited. Kang et al. [12] conducted ligation of the uterine vessels and cardinal ligament with a conventional suturing technique using delayed absorbable polyglactin 1-0 suture, which was then reinforced by a delayed absorbable polyglactin 1-0 round loop. The operative times and changes in Hb levels closely resembled our surgical outcomes; however, eight patients (1.1%) experienced urinary tract injuries. On the other hand, in our study, only one bladder serosa injury occurred during dissection of the vesicovaginal space, and no other ureteral injuries occurred.
An endo-loop is commonly used in laparoscopic appendectomy and has demonstrated success in closing the appendiceal base. However, the rate of intraoperative complications with the use of endo-loop ligatures was low at 2.5%; however, the rate of postoperative complications was 4.6%, and there was a heightened risk of abscess formation [27]. Additionally, suturing the uterine vessels and surrounding excessive tissue using an endo-loop may result in ureteral kinking [12] or slippage due to tissue ischemia [11].
Another method for ligation of the uterine vessels is the use of Hem-o-lock clips. Hem-o-lock clips are known to be effective for ligation of the renal blood vessels, have a low tendency to slip when controlling major blood vessels [28], and are more cost-effective than endo-loops [29]. Lee et al. [11] first conducted uterine vessel ligation using Hem-o-lok clips, and their results concerning surgical complications and changes in Hb levels were similar to those in our study. However, the operative time was approximately 60 minutes longer than that with our knotless 1-0 V-LocTM 180 suturing method. This may be attributed to the challenges of applying Hem-o-lock clips, including the necessity for complete dissection of the uterine vessels, even in cases with very engorged or embedded vessels. Moreover, there is a disadvantage in that the venous blood vessels can be easily perforated if the clip is applied incorrectly.
There are several advantages to using 1-0 V-LocTM 180 suture. Firstly, initial anchoring of the knotless suture requires less skill compared to applying conventional sutures. This can reduce the suturing time associated with the total operative time. Secondly, it can also reduce the risk of unequal tension on the knots when performing conventional knot tying, which requires constant tensile strength. Thirdly, unidirectional barbed absorbable sutures can provide equal tensile strength to conventional smooth suture materials and minimize tissue infection [30]. These advantages of V-LocTM 180 were associated with enhanced safety and efficacy based on the shorter operative times and reduced EBL and vaginal cuff granuloma formation rates during suturing of the vaginal cuff in TLH [16,31]. Therefore, the use of 1-0 V-LocTM 180 suture for uterine vessel ligation in TLH, as initiated in our study, appears suitable. However, more studies are needed to evaluate its safety and efficacy.
This study has several limitations. The primary limitation is the absence of TLH cases without the use of 1-0 V-LocTM 180 suture. This occurred because, during the study period, most TLH procedures in our institutions involved the use of 1-0 V-LocTM 180 suture, which led to the selection of LAVH as the control group. However, it is worth highlighting that both LAVH and TLH in our study employed suturing and tying of uterine vessels through different approaches, with LAVH doing so vaginally and conventional TLH frequently using an energy device for ligation. Nevertheless, since both procedures involved suturing for uterine vessel ligation in our study, we believe there is some significance in the way our study was structured. The aim of this study focused on the safety and feasibility of knotless uterine artery ligation during TLH, with the goal of achieving a more straightforward and secure TLH procedure compared to LAVH. However, to confirm the efficacy of TLH with 1-0 V-LocTM 180 suture, we plan to conduct a randomized controlled trial on its use in TLH.
The second limitation of our study is that the TLH group (n=119) included both robotic (n=31) and laparoscopic (n=88) surgery cases. However, when analyzing the data, no significant differences were observed in baseline characteristics, including maximal uterine diameter and operative outcomes, such as complication rates, EBL, and the weight of the removed uterus, between robotic and laparoscopic TLH cases (data not shown).
This study aimed to determine how to perform uterine artery ligation with knotless 1-0 V-LocTM 180 suture during TLH. In the case of robotic surgery in this study, a reduced port incision technique was employed, which meant that the surgeon operated with only two robotic arms, omitting the use of the third arm. In this situation, when the surgeon performed uterine vessel ligation, one hand was used to push the uterus to the side and the other hand was used for the ligation. At this time, the 1-0 V-LocTM 180 thread was only handled with one hand. Consequently, the surgical conditions for operating within a confined pelvic cavity using two hands were found to be similar to laparoscopic surgery. With this new knotless suturing method, the ligation of the uterine vessels entails tightening the barbed suture only 3-4 times; therefore, the difference between robotic and laparoscopic surgery for this procedure was not considered significant.
In the past, a large uterus was a relative contraindication for LH. However, with the development of minimally invasive surgery, even a large uterus can now be removed through laparoscopy [23,24]. As such, more studies are needed to make TLH safer and more effective. In this sense, this study is meaningful in that it proposes a new surgical option for TLH. The use of the knotless 1-0 V-LocTM 180 suture for uterine vessel ligation is a surgical procedure that minimizes the risk of thermal damage and reduces the risk of ureteral injury or uterine vessel bleeding, even in patients with large uteri, vessel engorgement, and limited space for tying knots, all within the constraints of a reduced port approach. Effective vessel ligation without loosening was achieved by tightening the suture with one hand and in one direction without the need for a tie. This procedure can be easily performed by anyone with one hand and can be safely used. In conclusion, the use of knotless 1-0 V-LocTM 180 suture for uterine vessel ligation can be considered one of the techniques for TLH, providing flexibility to surgeons and catering to the specific needs of patients.
Notes
Ethical approval
This study was approved by the Asan Medical Center Institutional Review Board (approval No. 2021-1101).
Fig. 1
Uterine vessel and parametrium ligation using 1-0 V-LocTM 180 (Covidien, Mansfield, MA, USA) suture in total laparoscopic hysterectomy. Uterine. V, uterine vein; Uterine. A, uterine artery.
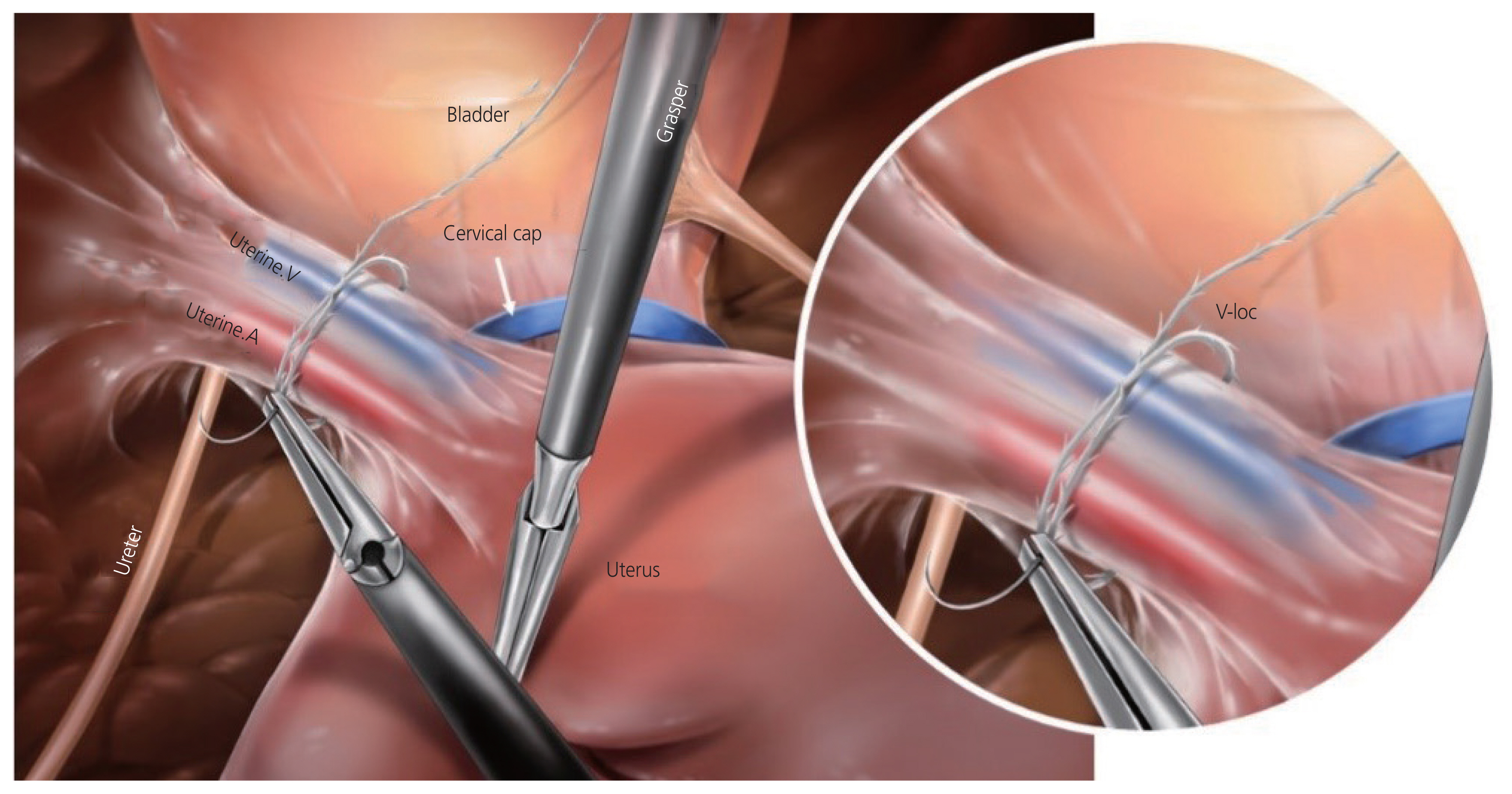
Table 1
Baseline patient characteristics
Table 2
Comparison of surgical outcome
Table 3
Surgical outcomes according to the maximal diameter of the uterus as determined by preoperative ultrasonography
Table 4
Surgical outcomes according to the weight of the uterus
Table 5
Intra- and postoperative complications
References
1. Aarts JW, Nieboer TE, Johnson N, Tavender E, Garry R, Mol BW, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2015;2015:CD003677.



2. Shen H, Torng PL, Chen IH, Hsu HC. Single-port laparoscopic hysterectomy for uteri greater than 500 grams. Taiwan J Obstet Gynecol 2020;59:502-7.


3. Song T, Lee Y, Kim ML, Yoon BS, Joo WD, Seong SJ, et al. Single-port access total laparoscopic hysterectomy for large uterus. Gynecol Obstet Invest 2013;75:16-20.



4. Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar H. Minimally invasive hysterectomies-a survey on attitudes and barriers among practicing gynecologists. J Minim Invasive Gynecol 2010;17:167-75.



5. Mani K, Govindarajan M, Selvaraj V. Comparison of total laparoscopic hysterectomy and laparoscopic assisted vaginal hysterectomy--a 2-year retrospective study. Int J Reprod Contracept Obstet Gynecol 2017;6:966-70.


6. Doucette RC, Sharp HT, Alder SC. Challenging generally accepted contraindications to vaginal hysterectomy. Am J Obstet Gynecol 2001 184:1386-9. discussion 1390-1.


7. Committee opinion no 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol 2017;129:e155-9.


8. Shin JW, Lee HH, Lee SP, Park CY. Total laparoscopic hysterectomy and laparoscopy-assisted vaginal hysterectomy. JSLS 2011;15:218-21.



9. Wang H, Li P, Li X, Gao L, Lu C, Zhao J, et al. Total laparoscopic hysterectomy in patients with large uteri: comparison of uterine removal by transvaginal and uterine morcellation approaches. Biomed Res Int 2016;2016:8784601.




10. Marwah V, Dutta S, Kedia S, Mittal P. Total laparoscopic hysterectomy (TLH) with endosuturing compared with conventional technique using energy sources. Facts Views Vis Obgyn 2021;13:149-58.



11. Lee JE, Kim KG, Lee DO, Seo SS, Kang S, Park SY, et al. Ligation of uterine vessels in total laparoscopic hysterectomy using Hem-o-lok clips. Taiwan J Obstet Gynecol 2015;54:8-12.


12. Kang HW, Lee JW, Kim HY, Kim BW, Moon CS. Total laparoscopic hysterectomy via suture and ligation technique. Obstet Gynecol Sci 2016;59:39-44.




13. Seehofer D, Mogl M, Boas-Knoop S, Unger J, Schirmeier A, Chopra S, et al. Safety and efficacy of new integrated bipolar and ultrasonic scissors compared to conventional laparoscopic 5-mm sealing and cutting instruments. Surg Endosc 2012;26:2541-9.



14. Wu MP, Ou CS, Chen SL, Yen EY, Rowbotham R. Complications and recommended practices for electrosurgery in laparoscopy. Am J Surg 2000;179:67-73.


15. Molinas CR, Binda MM, Sisa CM, Campo R. A randomized control trial to evaluate the importance of pretraining basic laparoscopic psychomotor skills upon the learning curve of laparoscopic intra-corporeal knot tying. Gynecol Surg 2017;14:29.




16. Cong L, Li C, Wei B, Zhan L, Wang W, Xu Y. V-Loc™ 180 suture in total laparoscopic hysterectomy: a retrospective study comparing Polysorb to barbed suture used for vaginal cuff closure. Eur J Obstet Gynecol Reprod Biol 2016;207:18-22.


17. Chan CC. The experience of the v-loc™ 180 wound closure device used in laparoscopic myomectomy. Fertil Steril 2013;100:S396.

18. Greenberg JA, Goldman RH. Barbed suture: a review of the technology and clinical uses in obstetrics and gynecology. Rev Obstet Gynecol 2013;6:107-15.


19. R Core Team. R: a language and environment for statistical computing [Internet] Vienna: R Foundation for Statistical Computing; c2020 [cited 2021 May 25]. Available from: https://www.R-project.org/
.
20. Twijnstra AR, Kianmanesh Rad NA, Smeets MJ, Admiraal JF, Jansen FW. Twenty-first century laparoscopic hysterectomy: should we not leave the vaginal step out? Gynecol Surg 2009;6:311-6.




21. Poojari VG, Bhat VV, Bhat R. Total laparoscopic hysterectomy with prior uterine artery ligation at its origin. Int J Reprod Med 2014;2014:420926.




22. Uccella S, Garzon S, Lanzo G, Gallina D, Bosco M, Porcari I, et al. Uterine artery closure at the origin vs at the uterus level in total laparoscopic hysterectomy: a randomized controlled trial. Acta Obstet Gynecol Scand 2021;100:1840-8.



23. O’Hanlan KA, McCutcheon SP, McCutcheon JG. Laparoscopic hysterectomy: impact of uterine size. J Minim Invasive Gynecol 2011;18:85-91.


24. Sinha R, Sundaram M, Lakhotia S, Mahajan C, Manaktala G, Shah P. Total laparoscopic hysterectomy for large uterus. J Gynecol Endosc Surg 2009;1:34-9.



25. Siedhoff MT, Wheeler SB, Rutstein SE, Geller EJ, Doll KM, Wu JM, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol 2015;212:591e1-8.

26. Huang HY, Yen CF, Wu MP. Complications of electrosurgery in laparoscopy. Gynecol Minim Invasive Ther 2014;3:39-42.

27. Makaram N, Knight SR, Ibrahim A, Patil P, Wilson MSJ. Closure of the appendiceal stump in laparoscopic appendectomy: a systematic review of the literature. Ann Med Surg (Lond) 2020;57:228-35.



28. Casale P, Pomara G, Simone M, Casarosa C, Fontana L, Francesca F. Hem-o-lok clips to control both the artery and the vein during laparoscopic nephrectomy: personal experience and review of the literature. J Endourol 2007;21:915-8.


29. Hue CS, Kim JS, Kim KH, Nam SH, Kim KW. The usefulness and safety of Hem-o-lok clips for the closure of appendicular stump during laparoscopic appendectomy. J Korean Surg Soc 2013;84:27-32.



-
METRICS

-
- 0 Crossref
- Scopus
- 632 View
- 85 Download
- Related articles in Obstet Gynecol Sci
-
The benefits of Non-coring technique in Laparoscopic Supracervical Hysterectomy.1998 November;41(11)
Study on Repairing Method of Vaginal Cuff in Total Laparoscopic Hysterectomy.2000 April;43(4)
The clinical studies on 600 cases of total laparoscopic hysterectomy (TLH).2006 November;49(11)
Three cases of vaginal evisceration after laparoscopic hysterectomy.2007 January;50(1)




















