Introduction
Conventional cancer treatments include surgery, chemotherapy, or radiotherapy, and are usually applicable in patients with early-stage or even locally advanced cervical cancer. However, there is no standard treatment for patients with metastatic cervical cancer because of its heterogeneous manifestations. The median survival time for metastatic cervical cancer is only 8 to 13 months [
1]. The 5-years survival rate for metastatic cervical cancer is 16.5% compared to 91.5% for localized cervical cancer [
2].
Isolated para-aortic lymph node (LN) metastasis after definitive initial treatment is quite rare, with radiologically detectable lesions varying from 1.7% to 2.1% [
3].
Surgical resection and additional adjuvant therapy is considered the most recommended modality. However, there are controversies regarding the treatment modalities for isolated para-aortic LN metastasis in uterine cervical cancer. Salvage radiotherapy or chemo-radiotherapy without surgery are sometimes done due to the risk of incomplete surgery and anatomical difficulties in accessing and removing metastatic lesions. It is difficult for surgeons to decide the extent of surgical resection without exact and clear anatomical information. To this effect, we tried 3-dimensional (3D) computed tomography (CT) angiography to visualize the area surrounding the lesion. We report a case of para-aortic lymphadenectomy for isolated enlarged LN after visualization with 3D CT angiography.
Case report
A 49-year-old woman visited us due to increased levels of carcinoembryonic antigen (CEA). In December 2012, the patient had undergone type III abdominal radical hysterectomy with bilateral salpingo-oophorectomy, and pelvic lymphadenectomy. Postoperative histopathologic examination indicated invasive adenosquamous cell carcinoma with involvement of the resected vaginal margin, left parametrium, and left pelvic LN. The patient received adjuvant intensity-modulated radiotherapy to the vagina and pelvic draining LNs (common, internal and external iliac, and presacral LN regions). The prescribed dose for the target volume was 50 Gy with 2 Gy fractions administered daily, 5 days per week.
Forty-five months after initial treatment, CEA levels increased up to 314 ng/mL (normal range <2.5 ng/mL). CT revealed a metastatic lesion more than 10 cm in size in the retroaortic and retrocaval basins. F18-fluorodeoxyglucose positron emission tomography (PET)-CT showed no other distant metastasis except the para-aortic lesion.
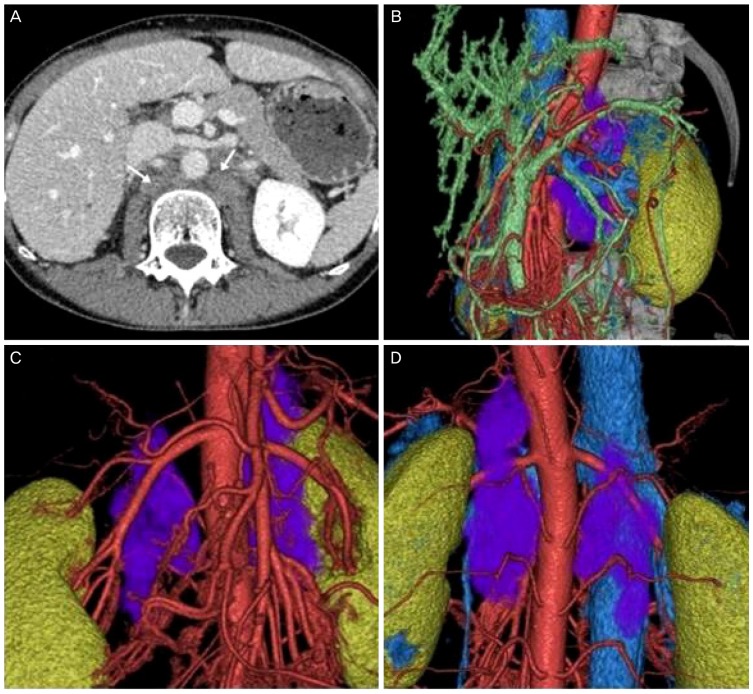
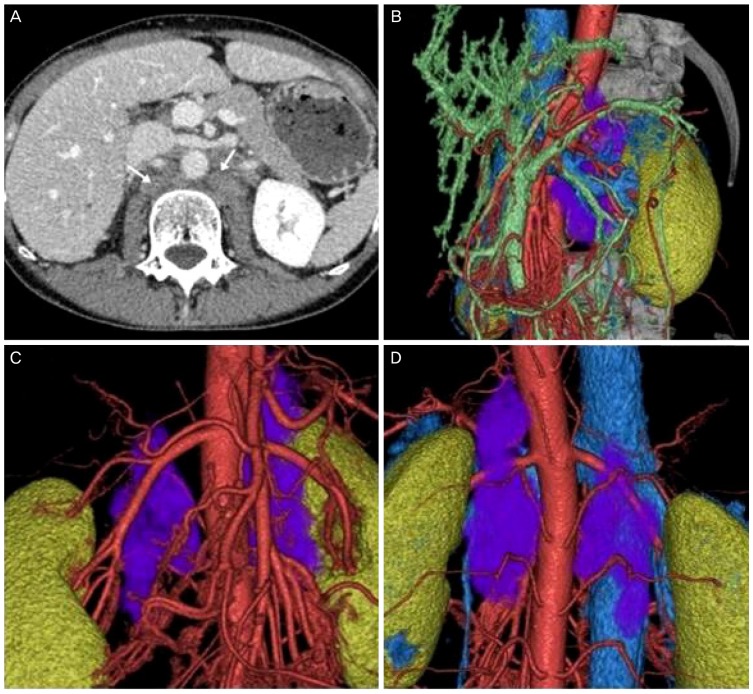
Preoperative 3D CT angiography showed a huge retro-crural metastatic LN with clear visualization and demarcation of the lesion. A metastatic lesion more than 10 cm in size was located behind the vena cava, aorta, and left kidney, encompassing the left renal and lumbar arteries (
Fig. 1). 3D CT angiography was performed with a 64 channel MDCT scanner (Aquilion 64; Toshiba Medical Systems, Tchigi, Japan). A total of 2.0 mL/kg of body weight of an iodine contrast medium, Iohexol (Omnipaque 300 syringe; Daiichi Sankyo, Tokyo, Japan) was administered at a rate of 3.5 mL/s with a power injector (Dual Shot GX; Nemoto Kyorindo, Tokyo, Japan), which was then flushed with 35 mL of normal saline solution, also at 3.5 mL/s. The obtained images were transferred to a computer workstation and reconstituted using 3D computer graphics software (Ziostation 2; Ziosoft, Tokyo, Japan).
Fig. 1
(A) Computed tomography (CT) image; arrows indicate the retro-crural metastatic lesions. (B) Three-dimensional (3D) CT angiography image, left side view; the purple color indicates the metastatic lesions. (C) 3D CT angiography image, anterior view. (D) 3D CT angiography image, posterior view.
Lymphadenectomy and left nephrectomy were performed as salvage surgery. The lesion was a 10×15-cm sized metastatic LN located on the left side of the vertebra. The lesion extended from the left kidney to the right renal vessels, encompassing the left renal artery and lumbar artery behind the aorta and vena cava. There were severe adhesions between the metastatic lesion and the posterior portion of the left kidney.
There was no invasion into the psoas muscle or the vertebra. All metastatic lesions were completely removed.
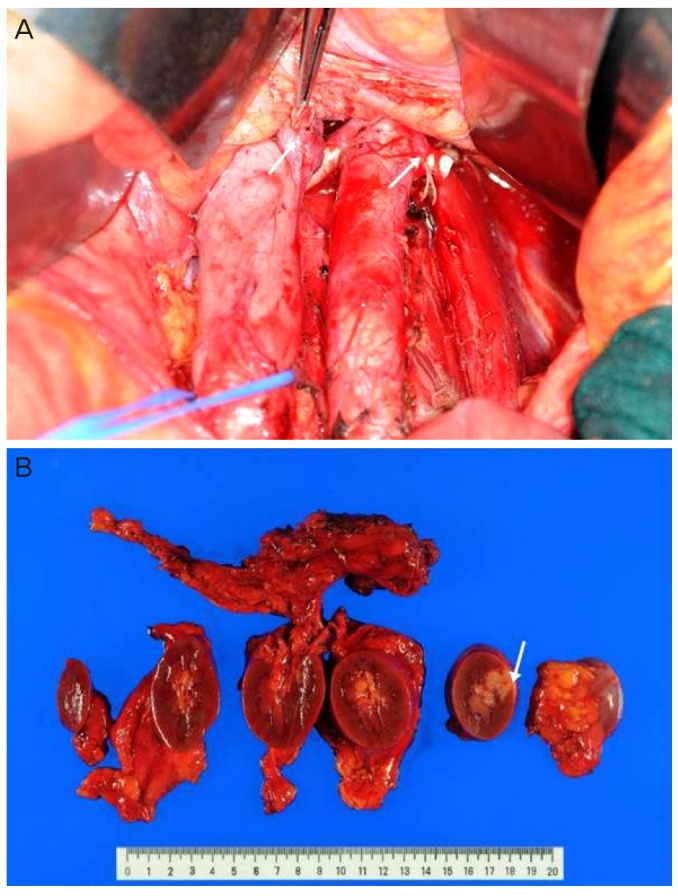
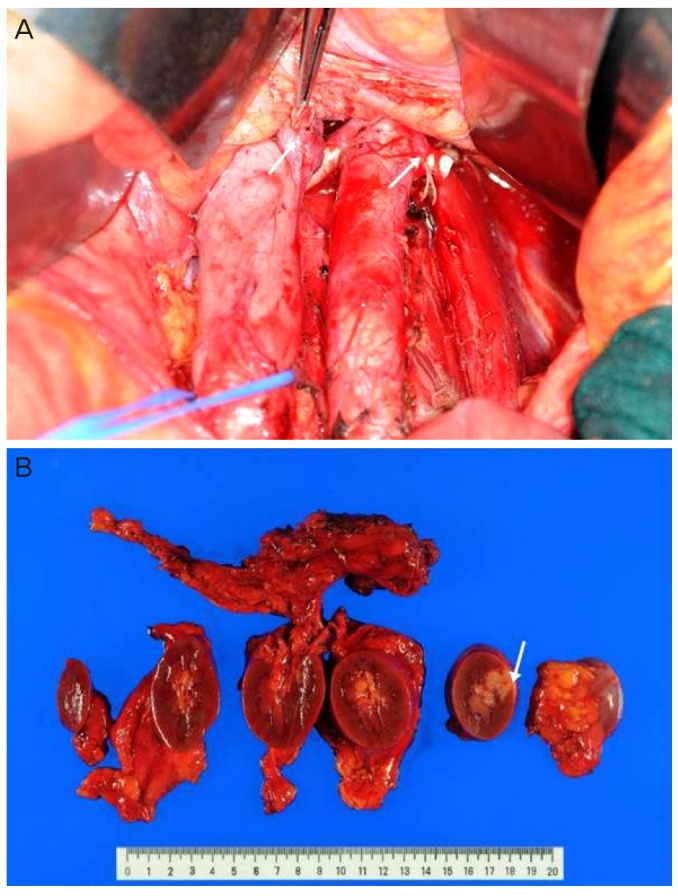
Histopathologic diagnosis revealed metastatic adenosquamous cell carcinoma in all the 5 resected para-aortic LNs. The tumor had also invaded into the pelvis of the left kidney (
Fig. 2). Cytological analysis of the peritoneal washing was negative for malignant cells.
Fig. 2
(A) Postoperative photography; arrows indicate the cut ends of left renal vein and left renal artery. (B) Resected retro-crural metastatic lymph node and left kidney; arrow indicates tumor invasion into the renal parenchyme.
Discussion
When para-aortic disease occurs, treatment is decided depending on the extent of the disease, primary treatment, performance status, or comorbidities present, if any. The management of this case was based on the size of the lesion (more than 10 cm), anatomical location (in the retroaortic and retrocaval basin), and histology (adenosquamous cell carcinoma). Salvage radiotherapy was not considered appropriate for this case as the enlarged metastatic lesion would require an external beam radiotherapy dose of approximately 55-60 Gy with conventional fractionation [
4]. In the current case, the metastatic lesion was located in the retroaortic and retrocaval basin encompassing the lumbar and left renal artery. Such a high radiotherapy dose can lead to significant injury of adjacent organs such as duodenum, small intestine, and kidney, considering the radiation tolerance [
5]. Huang et al. [
6] reported that adenosquamous cell carcinoma of cervix showed poor survival outcome compared with squamous cell carcinoma treated using the same radiotherapy protocol. Therefore, we decided to reduce the tumor volume to increase the response to the adjuvant therapy such as systemic chemotherapy or chemoradiotherapy.
Salvage surgery has a limited role in patients with isolated para-aortic LN metastasis considering the high associated morbidity and mortality rates (10% to 16%) [
7]. Recently with the development of laparoscopy surgical resection has reduced morbidity. However, for larger metastatic lesions both laparotomic and laparoscopic approaches are not easy as the procedure needs lifting up of the aorta and the vena cava, along with meticulous dissection along the neighboring organs. Metastatic LN in the retroaortic or retrocaval basins sometimes show extracapsular invasion into neighboring organs, encompassing the neighboring arteries and veins [
8]. Before salvage surgery for a metastatic lesion that is located at a site that gynecologists are unfamiliar with, a complete understanding of the anatomy and spatial perception are required. Currently, CT and magnetic resonance imaging (MRI) are the standard tools available to determine the proximity of a LN recurrence to vital structures. However, previous studies have often underestimated the level of involvement, which requires the surgeon to perform a much more extensive and complex dissection than anticipated [
9]. CT, MRI, and PET-CT are good tools for the detection and diagnosis of recurrence, however, these imaging modalities lack providing useful anatomical information such as the exact size, margin of lesion, spatial relation with neighboring organs, along with clear colorful visualization and demarcation to surgeons who are unfamiliar with images in black and white. There are few studies comparing the usefulness of 3D CT angiography and conventional imaging modalities such as conventional CT and MRI. 3D CT angiography is considered useful in the mapping of vascular structures surrounding the lesion [
10,
11]. We have previously reported a study on preoperative 3D CT angiography of the uterine artery in patients with uterine cervical cancer [
12]. The authors have used 3D CT angiography to understand the anatomical relations surrounding the metastatic lesion, with neighboring organs visualized in different colors, similar to images in anatomy textbooks. It clearly demarcated the lesion and distinctly demonstrated anatomical relations between organs. The surgeon can visualize the lesion from all directions and can have spatial perception of the lesion. Thus 3D CT angiography can be helpful for surgeons to decide the operability, the extent of resection, and which organs would be sacrificed.
Although there are controversies regarding appropriate treatment modalities for isolated extra-pelvic recurrence of uterine cervical cancer, surgical resection and additional adjuvant therapy is considered the most recommended modality, provided they do not result in severe morbidity or delay of sequential treatment. For surgery in recurrent cancer, exact and clear anatomical information and experienced surgeons are required, as it has a high risk of failure.
There are cases of incomplete removal of metastases with laparotomy because of the higher incidence of extracapsular invasion in cervical cancers than in ovarian cancers. Among 15 patients with recurrent cervical cancer and metastatic bulky LNs, an experienced surgeon was unable to perform complete removal in 5 patients because of such extracapsular invasion [
13].
Compared with conventional imaging techniques, 3D CT angiography can more clearly visualize lesions, as it provides useful anatomical information such as the exact size and location with clear visualization and demarcation.
Our experience suggests that for salvage surgery in recurrent gynecological cancer, 3D CT angiography would be helpful in reducing the risk of incomplete surgery and minimizing the morbidity caused by more extensive resection.